Abstract
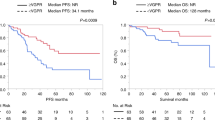
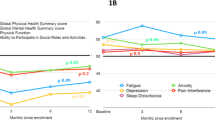
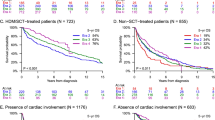
Autologous stem cell Transplant (ASCT)-related mortality (TRM) in AL amyloidosis remains elevated. AL amyloidosis patients (n = 1718) from 9 centers, transplanted 2003–2020 were included. Pre-ASCT variables of interest were assessed for association with day-100 all-cause mortality. A random forest (RF) classifier with 10-fold cross-validation assisted in variable selection. The final model was fitted using logistic regression. The median age at ASCT was 58 years. Day-100 TRM occurred in 75 patients (4.4%) with the predominant causes being shock, high-grade arrhythmia, and organ failure. Ten factors were associated with day-100 TRM on univariate analysis. RF classifier using these variables generated a model with an area under the curve (AUC) of 0.72 ± 0.12. To refine the model selection using importance hierarchy function, a 4-variable model [NT-proBNP/BNP, serum albumin, ECOG performance status (PS), and systolic blood pressure] was built with an AUC of 0.70 ± 0.12. Based on logistic regression coefficients, ECOG PS 2/3 was assigned two points while other adverse predictors 1-point each. The model score range was 0–5, with a day-100 TRM of 0.46%, 3.2%, 5.8%, and 14.5% for 0, 1, 2, and ≥3 points, respectively. This model to predict day-100 TRM in AL amyloidosis allows better-informed decision-making in this heterogeneous disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset of this study is not publicly available due to the proprietary nature of the electronic health records and maintaining patient anonymity mandated by the institutional review boards.
References
Sanchorawala V, Boccadoro M, Gertz M, Hegenbart U, Kastritis E, Landau H, et al. Guidelines for high dose chemotherapy and stem cell transplantation for systemic AL amyloidosis: EHA-ISA working group guidelines. Amyloid. 2022;29:1–7. https://doi.org/10.1080/13506129.2021.2002841.
Cibeira MT, Sanchorawala V, Seldin DC, Quillen K, Berk JL, Dember LM, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation: long-term results in a series of 421 patients. Blood. 2011;118:4346–52. https://doi.org/10.1182/blood-2011-01-330738.
D’Souza A, Dispenzieri A, Wirk B, Zhang MJ, Huang J, Gertz MA, et al. Improved outcomes after autologous hematopoietic cell transplantation for light chain amyloidosis: a center for international blood and marrow transplant research study. J Clin Oncol. 2015;33:3741–9. https://doi.org/10.1200/JCO.2015.62.4015.
Gertz MA, Schonland S. Stem cell mobilization and autologous transplant for immunoglobulin light-chain amyloidosis. Hematol Oncol Clin North Am. 2020;34:1133–44. https://doi.org/10.1016/j.hoc.2020.07.007.
Gutierrez-Garcia G, Cibeira MT, Rovira M, Fernandez de Larrea C, Tovar N, Rodriguez-Lobato LG, et al. Improving security of autologous hematopoietic stem cell transplant in patients with light-chain amyloidosis. Bone Marrow Transplant. 2019;54:1295–303. https://doi.org/10.1038/s41409-019-0447-y.
Jaccard A, Moreau P, Leblond V, Leleu X, Benboubker L, Hermine O, et al. High-dose melphalan versus melphalan plus dexamethasone for AL amyloidosis. N Engl J Med. 2007;357:1083–93. https://doi.org/10.1056/NEJMoa070484.
Sharpley FA, Petrie A, Mahmood S, Sachchithanantham S, Lachmann HJ, Gillmore JD, et al. A 24-year experience of autologous stem cell transplantation for light chain amyloidosis patients in the United Kingdom. Br J Haematol. 2019;187:642–52. https://doi.org/10.1111/bjh.16143.
Skinner M, Sanchorawala V, Seldin DC, Dember LM, Falk RH, Berk JL, et al. High-dose melphalan and autologous stem-cell transplantation in patients with AL amyloidosis: an 8-year study. Ann Intern Med. 2004;140:85–93. https://doi.org/10.7326/0003-4819-140-2-200401200-00008.
Tandon N, Muchtar E, Sidana S, Dispenzieri A, Lacy MQ, Dingli D, et al. Revisiting conditioning dose in newly diagnosed light chain amyloidosis undergoing frontline autologous stem cell transplant: impact on response and survival. Bone Marrow Transplant. 2017;52:1126–32. https://doi.org/10.1038/bmt.2017.68.
Tsai SB, Seldin DC, Quillen K, Berk JL, Ruberg FL, Meier-Ewert H, et al. High-dose melphalan and stem cell transplantation for patients with AL amyloidosis: trends in treatment-related mortality over the past 17 years at a single referral center. Blood. 2012;120:4445–6. https://doi.org/10.1182/blood-2012-09-457341.
Gertz MA, Lacy MQ, Dispenzieri A, Kumar SK, Dingli D, Leung N, et al. Refinement in patient selection to reduce treatment-related mortality from autologous stem cell transplantation in amyloidosis. Bone Marrow Transplant. 2013;48:557–61. https://doi.org/10.1038/bmt.2012.170.
Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Dingli D, et al. Autologous stem cell transplant for immunoglobulin light chain amyloidosis: a status report. Leuk Lymphoma. 2010;51:2181–7. https://doi.org/10.3109/10428194.2010.524329.
Dingli D, Tan TS, Kumar SK, Buadi FK, Dispenzieri A, Hayman SR, et al. Stem cell transplantation in patients with autonomic neuropathy due to primary (AL) amyloidosis. Neurology. 2010;74:913–8. https://doi.org/10.1212/WNL.0b013e3181d55f4d.
Kastritis E, Palladini G, Minnema MC, Wechalekar AD, Jaccard A, Lee HC, et al. Daratumumab-based treatment for immunoglobulin light-chain amyloidosis. N Engl J Med. 2021;385:46–58. https://doi.org/10.1056/NEJMoa2028631.
Kastritis E, Wechalekar AD, Dimopoulos MA, Merlini G, Hawkins PN, Perfetti V, et al. Bortezomib with or without dexamethasone in primary systemic (light chain) amyloidosis. J Clin Oncol. 2010;28:1031–7. https://doi.org/10.1200/JCO.2009.23.8220.
Manwani R, Cohen O, Sharpley F, Mahmood S, Sachchithanantham S, Foard D, et al. A prospective observational study of 915 patients with systemic AL amyloidosis treated with upfront bortezomib. Blood. 2019;134:2271–80. https://doi.org/10.1182/blood.2019000834.
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Colby C, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30:989–95. https://doi.org/10.1200/JCO.2011.38.5724.
Wechalekar AD, Schonland SO, Kastritis E, Gillmore JD, Dimopoulos MA, Lane T, et al. A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood. 2013;121:3420–7. https://doi.org/10.1182/blood-2012-12-473066.
Dispenzieri A, Kyle RA, Gertz MA, Therneau TM, Miller WL, Chandrasekaran K, et al. Survival in patients with primary systemic amyloidosis and raised serum cardiac troponins. Lancet. 2003;361:1787–9. https://doi.org/10.1016/S0140-6736(03)13396-X.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9. https://doi.org/10.1182/blood-2005-05-2004.
Leung N, Kumar SK, Glavey SV, Dispenzieri A, Lacy MQ, Buadi FK, et al. The impact of dialysis on the survival of patients with immunoglobulin light chain (AL) amyloidosis undergoing autologous stem cell transplantation. Nephrol Dial Transplant. 2016;31:1284–9. https://doi.org/10.1093/ndt/gfv328.
Rezk T, Lachmann HJ, Fontana M, Naharro AM, Sachchithanantham S, Mahmood S, et al. Cardiorenal AL amyloidosis: risk stratification and outcomes based upon cardiac and renal biomarkers. Br J Haematol. 2019;186:460–70. https://doi.org/10.1111/bjh.15955.
Park MA, Mueller PS, Kyle RA, Larson DR, Plevak MF, Gertz MA. Primary (AL) hepatic amyloidosis: clinical features and natural history in 98 patients. Medicine. 2003;82:291–8. https://doi.org/10.1097/01.md.0000091183.93122.c7.
Dispenzieri A, Gertz MA, Kyle RA, Lacy MQ, Burritt MF, Therneau TM, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751–7. https://doi.org/10.1200/JCO.2004.03.029.
Palladini G, Sachchithanantham S, Milani P, Gillmore J, Foli A, Lachmann H, et al. A European collaborative study of cyclophosphamide, bortezomib, and dexamethasone in upfront treatment of systemic AL amyloidosis. Blood. 2015;126:612–5. https://doi.org/10.1182/blood-2015-01-620302.
Muchtar E, Kumar SK, Gertz MA, Grogan M, AbouEzzeddine OF, Jaffe AS, et al. Staging systems use for risk stratification of systemic amyloidosis in the era of high-sensitivity troponin T assay. Blood. 2019;133:763–6. https://doi.org/10.1182/blood-2018-10-875252.
Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–49. https://doi.org/10.1002/mpr.329.
Barrett CD, Dobos K, Liedtke M, Tuzovic M, Haddad F, Kobayashi Y, et al. A changing landscape of mortality for systemic light chain amyloidosis. JACC Heart Fail. 2019;7:958–66. https://doi.org/10.1016/j.jchf.2019.07.007.
Khwaja J, Ravichandran S, Bomsztyk J, Cohen O, Foard D, Martinez-Naharro A, et al. Limited utility of Mayo 2012 cardiac staging system for risk stratification of patients with advanced cardiac AL amyloidosis—analysis of a uniformly treated cohort of 1,275 patients. Haematologica. 2024;109:1598–602. https://doi.org/10.3324/haematol.2023.284348.
Sidiqi MH, Aljama MA, Buadi FK, Warsame RM, Lacy MQ, Dispenzieri A, et al. Stem cell transplantation for light chain amyloidosis: decreased early mortality over time. J Clin Oncol. 2018;36:1323–9. https://doi.org/10.1200/JCO.2017.76.9554.
Ho M, Moscvin M, Low SK, Evans B, Close S, Schlossman R, et al. Risk factors for the development of orthostatic hypotension during autologous stem cell transplant in patients with multiple myeloma. Leuk Lymphoma. 2022;63:2403–12. https://doi.org/10.1080/10428194.2022.2084729.
Muchtar E, Lin G, Grogan M. The challenges in chemotherapy and stem cell transplantation for light-chain amyloidosis. Can J Cardiol. 2020;36:384–95. https://doi.org/10.1016/j.cjca.2019.11.032.
Biran N, Sehgal P, Sahni G, Doucette J, Chari A. Outcome of patients with multiple myeloma and hypotension during high-dose chemotherapy. Am J Hematol. 2015;90:E125–127. https://doi.org/10.1002/ajh.23991.
Hryciw N, Joannidis M, Hiremath S, Callum J, Clark EG. Intravenous albumin for mitigating hypotension and augmenting ultrafiltration during kidney replacement therapy. Clin J Am Soc Nephrol. 2021;16:820–8. https://doi.org/10.2215/CJN.09670620.
Lee SY, Meehan RS, Seldin DC, Sloan JM, Quillen K, Shelton A, et al. Effect of severe hypoalbuminemia on toxicity of high-dose melphalan and autologous stem cell transplantation in patients with AL amyloidosis. Bone Marrow Transplant. 2016;51:1318–22. https://doi.org/10.1038/bmt.2016.132.
Levy BI, Schiffrin EL, Mourad JJ, Agostini D, Vicaut E, Safar ME, et al. Impaired tissue perfusion: a pathology common to hypertension, obesity, and diabetes mellitus. Circulation. 2008;118:968–76. https://doi.org/10.1161/CIRCULATIONAHA.107.763730.
Sharma PP, Payvar S, Litovsky SH. Histomorphometric analysis of intramyocardial vessels in primary and senile amyloidosis: epicardium versus endocardium. Cardiovasc Pathol. 2008;17:65–71. https://doi.org/10.1016/j.carpath.2007.05.008.
Mellgard GS, Bhutani D, Mapara MY, Maurer MS, Radhakrishnan J, Lentzsch S, et al. High-dose melphalan-autologous hematopoietic cell transplantation in systemic AL amyloidosis following daratumumab-based frontline therapy. Bone Marrow Transplant. 2024;59:1181–3. https://doi.org/10.1038/s41409-024-02301-7.
Funding
This study was supported by the Mayo Clinic Transplant Center Scholarly Award.
Author information
Authors and Affiliations
Contributions
Conceptualization: Eli Muchtar, Morie Gertz. Data curation: Eli Muchtar, Angela Dispenzieri, Vaishali Sanchorawala, Hamza Hassan, Francis Buadi, Hans C. Lee, Muzaffar Qazilbash, Andrew Kin, Jeffrey Zonder, Sally Arai, Michelle M. Chin, Rajshekhar Chakraborty, Suzanne Lentzsch, Hila Magen, Eden Shkury, Caitlin Sarubbi, Heather Landau, Stefan Schönland, Ute Hegenbart, Morie Gertz. Formal and statistical analysis: Eli Muchtar, Angela Dispenzieri, Raphael Mwangi, Matthew Maurer, Morie Gertz. Original draft writing: Eli Muchtar, Morie Gertz, Draft editing and critical review: All authors. Approval of final draft: All authors.
Corresponding author
Ethics declarations
Competing interests
EM received a consultation fee from Protego (a fee paid to the institution). AD received research funding from Celgene, Millennium Pharmaceuticals, Pfizer, and Janssen and received a travel grant from Pfizer. VS received research support from Celgene, Millennium-Takeda, Janssen, Prothena, Sorrento, Karyopharm, Oncopeptide, Caelum, serves as a consultant for Janssen and Pfizer and served on the advisory board for Proclara, Caelum, Abbvie, Janssen, Regeneron, Protego, Pharmatrace, Telix, Prothena. MM received research funding from Roche/Genentech, BMS, and GenMab and provided consultancy/Advisory Board for AstraZeneca and BMS. HCL received research funding from Amgen, Bristol Myers Squibb, Janssen, GlaxoSmithKline, Regeneron, and Takeda Pharmaceuticals and provided consultancy to Abbvie, Bristol Myers Squibb, Janssen, Regeneron, GlaxoSmithKline, Sanofi, Takeda Pharmaceuticals, Allogene Therapeutics, and Pfizer. RC serves as Consultant/Advisory Board for Janssen, Sanofi, Adaptive Biotech and received research funding from Genentech, AbbVie. UH received honoraria from Janssen, Pfizer, Alnylam, Prothena, Astra Zeneca, received financial support for congress participation from Janssen, Prothena, and Pfizer, serves on advisory Boards for Pfizer, Prothena, Janssen, Alexion, Alnylam and received financial sponsoring of Amyloidosis Registry from Janssen. MAG served as a consultant for Millennium Pharmaceuticals and received honoraria from Celgene, Millennium Pharmaceuticals, Onyx Pharmaceuticals, Novartis, GlaxoSmithKline, Prothena, Ionis Pharmaceuticals, and Amgen). The remaining authors declare no competing financial interests.
Ethics approval and consent to participate statement
All methods were performed in accordance with the relevant guidelines and regulations. The study was approved by the IRBs in all participating centers [lead site (Mayo Clinic) IRB number 20-011936]. Informed consent for medical research was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muchtar, E., Dispenzieri, A., Sanchorawala, V. et al. A model for predicting day-100 stem cell transplant-related mortality in AL amyloidosis. Bone Marrow Transplant 60, 595–602 (2025). https://doi.org/10.1038/s41409-025-02535-z
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02535-z