Abstract
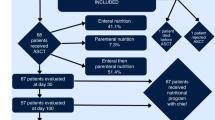
Food insecurity (FI), defined as the lack of continuous access to adequate food, affects 17–55% of cancer patients. Effects may be exacerbated in hematopoietic stem cell transplant (HSCT) patients, who face nutritional challenges due to treatment side effects, leading to weight loss and malnutrition. We hypothesize that pre-HSCT FI increases the risk of malnutrition, requiring nutrition support, and adverse psychosocial outcomes. Between February 2018 and August 2022, 284 patients were screened before HSCT for FI. 71 (25%) were excluded due to missing data. Of the remaining 213, 20 (9.4%) reported pre-HSCT FI. Patients with FI were more likely to develop malnutrition during HSCT (70% vs. 45.1%, p = 0.034) and need total parenteral nutrition compared to those without FI (65% vs. 34.2%, p = 0.013). Patients with FI also were more likely to screen positive for depression (40% vs. 10.4%, p = 0.002) and financial toxicity (75% vs. 25%, p < 0.001). There were no significant differences in survival or other secondary outcomes. Our study demonstrates that pre-HSCT FI significantly increases likelihood of malnutrition, the need for total parenteral nutrition, and adverse psychosocial outcomes in HSCT patients. These findings highlight the critical importance of early identification and interventions to address FI as part of comprehensive cancer care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Raber M, Jackson A, Basen-Engquist K, Bradley C, Chambers S, Gany FM, et al. Food Insecurity Among People With Cancer: Nutritional Needs as an Essential Component of Care. JNCI: J Natl Cancer Inst. 2022;114:1577–83.
America F. Hunger in America 2014: National Report. 2014 August 2014.
Reeder N, Tolar-Peterson T, Bailey RH, Cheng WH, Evans MW Jr. Food Insecurity and Depression among US Adults: NHANES 2005-2016. Nutrients. 2022;14:5.
Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: a review of the literature. Am J Prev Med. 2011;40:166–73.
Gundersen C, Ziliak JP. Food Insecurity And Health Outcomes. Health Aff (Millwood). 2015;34:1830–9.
Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The Relationship Between Food Insecurity and Depression, Diabetes Distress and Medication Adherence Among Low-Income Patients with Poorly-Controlled Diabetes. J Gen Intern Med. 2015;30:1476–80.
Bleich SN, Koma JW, Jernigan VBB. The Worsening Problem of Food Insecurity. JAMA Health Forum. 2023;4:e234974–e.
Khaddour K, Hana CK, Mewawalla P Hematopoietic Stem Cell Transplantation. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC. 2023.
Hong S, Majhail NS. Increasing access to allotransplants in the United States: the impact of race, geography, and socioeconomics. Hematology. 2021;2021:275–80.
Ogland-Hand C, Ciesielski TH, Daunov K, Bean MK, Nock NL Food Insecurity and Nutritional Challenges in Adolescent and Young Adult Cancer Survivors in the U.S.A.: A Narrative Review and Call to Action. Nutrients. 2023;15.
Blue BJ, Brazauskas R, Chen K, Patel J, Zeidan AM, Steinberg A, et al. Racial and Socioeconomic Disparities in Long-Term Outcomes in ≥1 Year Allogeneic Hematopoietic Cell Transplantation Survivors: A CIBMTR Analysis. Transplant Cell Ther, Off Publ Am Soc Transplant Cell Ther. 2023;29:7–10.
Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, Barone C, et al. Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget. 2017;8:79884–96.
Carvajal-Aldaz D, Cucalon G, Ordonez C. Food insecurity as a risk factor for obesity: A review. Front Nutr. 2022;9:1012734.
Hazzard VM, Loth KA, Hooper L, Becker CB. Food Insecurity and Eating Disorders: a Review of Emerging Evidence. Curr Psychiatry Rep. 2020;22:74.
Darling KE, Fahrenkamp AJ, Wilson SM, D’Auria AL, Sato AF. Physical and mental health outcomes associated with prior food insecurity among young adults. J Health Psychol. 2017;22:572–81.
Silva FR, de Oliveira MG, Souza AS, Figueroa JN, Santos CS. Factors associated with malnutrition in hospitalized cancer patients: a croos-sectional study. Nutr J. 2015;14:123.
Gyan E, Raynard B, Durand JP, Lacau Saint Guily J, Gouy S, Movschin ML, et al. Malnutrition in Patients With Cancer: Comparison of Perceptions by Patients, Relatives, and Physicians-Results of the NutriCancer2012 Study. JPEN J Parenter Enter Nutr. 2018;42:255–60.
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140:304–10.
Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals. JAMA Netw Open. 2019;2:e1911514. e
Wiener L, Sannes T, Randall J, Lahijani S, Applebaum A, Gray T, et al. Psychosocial Assessment Practices for Hematopoietic Stem Cell Transplantation: A National Survey Study. Res Sq. 2023;58:6–9.
Lew MV, Ren Y, Lowder YP, Siamakpour-Reihani S, Ramalingam S, Romero KM, et al. Geriatric Assessment Reveals Actionable Impairments in Hematopoietic Stem Cell Transplantation Candidates Age 18 to 80 Years. Transpl Cell Ther. 2022;28:498.e1–e9.
Medicaid CfMa. The Accountable Health Communities Health-Related Social Needs Screening Tool 2022 [Available from: https://www.cms.gov/priorities/innovation/files/worksheets/ahcm-screeningtool.pdf.
Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26–32.
U.S. Department of Agriculture ERSnd. Key statistics & graphics. USDA, accessed 14 November, 2023.
Gray TW, Podewils LJ, Rasulo RM, Weiss RP, Tomcho MM. Examining the Implementation of Health-Related Social Need (HRSN) Screenings at a Pediatric Community Health Center. J Prim Care Community Health. 2023;14:21501319231171519.
Holcomb J, Highfield L, Ferguson GM, Morgan RO. Association of Social Needs and Healthcare Utilization Among Medicare and Medicaid Beneficiaries in the Accountable Health Communities Model. J Gen Intern Med. 2022;37:3692–9.
Murray E, Roosevelt GE, Vogel JA. Screening for health-related social needs in the emergency department: Adaptability and fidelity during the COVID-19 pandemic. Am J Emerg Med. 2022;54:323.e1–e4.
Lew MV, Ren Y, Lowder YP, Siamakpour-Reihani S, Ramalingam S, Romero KM, et al. Geriatric Assessment Reveals Actionable Impairments in Hematopoietic Stem Cell Transplantation Candidates Age 18 to 80 Years. Transplant Cell Ther. 2022;28:498.e1–e9.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
McQuellon RP, Russell GB, Cella DF, Craven BL, Brady M, Bonomi A, et al. Quality of life measurement in bone marrow transplantation: development of the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale. Bone Marrow Transpl. 1997;19:357–68.
de Souza JA, Yap BJ, Hlubocky FJ, Wroblewski K, Ratain MJ, Cella D, et al. The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer. 2014;120:3245–53.
Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18:381–90.
West MA, Wischmeyer PE, Grocott MPW. Prehabilitation and Nutritional Support to Improve Perioperative Outcomes. Curr Anesthesiol Rep. 2017;7:340–9.
White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN. J Parenter Enter Nutr. 2012;36:275–83.
El Chaar D, Mattar L, Fakih El Khoury C. AND/ASPEN and the GLIM malnutrition diagnostic criteria have a high degree of criterion validity and reliability for the identification of malnutrition in a hospital setting: A single-center prospective study. J Parenter Enter Nutr. 2022;46:1061–70.
Hussaini SMQ, Ren Y, Racioppi A, Lew MV, Bohannon L, Johnson E, et al. Financial Toxicity and Quality of Life in Patients Undergoing Stem-Cell Transplant Evaluation: A Single-Center Analysis. JCO Oncol Pr. 2024;20:351–60.
Kamiya T, Hira D, Hoshino N, Kurihara M, Nakagawa M, Sasaki M, et al. Low Body Mass Index and Myeloablative Conditioning Regimen Prolong the Duration of Parenteral Nutrition During Hematopoietic Stem Cell Transplantation. Ann Nutr Metab. 2019;74:107–14.
Mattsson J, Westin S, Edlund S, Remberger M. Poor oral nutrition after allogeneic stem cell transplantation correlates significantly with severe graft-versus-host disease. Bone Marrow Transpl. 2006;38:629–33.
Beckerson J, Szydlo RM, Hickson M, Mactier CE, Innes AJ, Gabriel IH, et al. Impact of route and adequacy of nutritional intake on outcomes of allogeneic haematopoietic cell transplantation for haematologic malignancies. Clin Nutr. 2019;38:738–44.
El-Ghammaz AMS, Ben Matoug R, Elzimaity M, Mostafa N. Nutritional status of allogeneic hematopoietic stem cell transplantation recipients: influencing risk factors and impact on survival. Support Care Cancer. 2017;25:3085–93.
Rzepecki P, Barzal J, Oborska S. Blood and marrow transplantation and nutritional support. Support Care Cancer. 2010;18:S57–65.
Horsley P, Bauer J, Gallagher B. Poor nutritional status prior to peripheral blood stem cell transplantation is associated with increased length of hospital stay. Bone Marrow Transpl. 2005;35:1113–6.
Eglseer D, Bauer S, Huber-Kraßnitzer B, Greinix H. Malnutrition risk prior to hematopoietic stem cell transplantation predicts mortality in adults. Bone Marrow Transpl. 2021;56:2268–71.
Bona K, Brazauskas R, He N, Lehmann L, Abdel-Azim H, Ahmed IA, et al. Neighborhood poverty and pediatric allogeneic hematopoietic cell transplantation outcomes: a CIBMTR analysis. Blood. 2021;137:556–68.
Pourmotabbed A, Moradi S, Babaei A, Ghavami A, Mohammadi H, Jalili C, et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutr. 2020;23:1778–90.
Reesor-Oyer L, Cepni AB, Lee CY, Zhao X, Hernandez DC. Disentangling food insecurity and maternal depression: which comes first? Public Health Nutr. 2021;24:5506–13.
Cain KS, Meyer SC, Cummer E, Patel KK, Casacchia NJ, Montez K, et al. Association of Food Insecurity with Mental Health Outcomes in Parents and Children. Acad Pediatr. 2022;22:1105–14.
Commission TJ. New requirements to reduce health care disparities. 2022.
Shoag J, Rotz SJ, Hanna R, Buhtoiarov I, Dewey EN, Bruckman D, et al. Disparities in access to hematopoietic cell transplant persist at a transplant center. Bone Marrow Transpl. 2024;59:1258–63.
Author information
Authors and Affiliations
Contributions
Conception and design: MAB, YPL, EJJ, HMW, IJ, BW, YZ, ADS. Financial support: ADS. Administrative support: MAB, YPL, EJJ, ATB, AX, LH, IG, BW, YZ. Provision of study materials or patients: MAB, YPL, EJJ, HMW, ATB, LH, IG, BW, YZ, EPA, NJC, TC, GC, MEH, GDL, RDL, SR, SS, KMH, PEW, ADS. Collection and assembly of data: MAB, YPL, EJJ, HW, ATB, AX, LH. Data analysis and interpretation: MAB, EJJ, YL, ADS. Manuscript writing: All authors. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors. Manuscript revision: MAB, EJJ, HMW, ADS.
Corresponding author
Ethics declarations
Competing interests
Dr Sung’s work has been funded by Merck, Novartis, Enterome, and Seres. He has received research product for studies from DSM/iHealth, Clasado, and BlueSpark Technologies. He has consulted for Targazyme, Acrotech, Geron, and Janssen.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. CPOP was implemented as a standard of care program. Therefore, patients were not consented as data was collected as part of routine care. The Duke Health Institutional Review Board approved the analysis of data collected as a quality improvement (QI) study (Pro00111631).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bergens, M.A., Lowder, Y.P., Li, Y. et al. Food insecurity prior to hematopoietic stem cell transplant is associated with malnutrition and worse outcomes. Bone Marrow Transplant 60, 857–863 (2025). https://doi.org/10.1038/s41409-025-02587-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02587-1