Abstract
The benefits of palliative care (PC) for hematopoietic cell transplant (HCT) patients are well established, however, uptake in pediatric HCT remains limited. To understand pediatric transplant physicians’ attitudes towards PC, we conducted a cross-sectional study with a 28-question survey. A composite score and regression model identified factors associated with positive attitudes towards subspecialty PC. Ninety-eight participants reported caring for pediatric patients. Most (81%) trust PC clinicians to care for their patients, yet 33% feel PC clinicians lack enough HCT knowledge to counsel patients. Nearly half (46%) see the name “PC” as a barrier to referral. Multivariable analysis showed that spiritual practice (β = 1.53, p = 0.029), <10 years of clinical practice (β = 2.23, p = 0.007), and perceived PC quality (β = 0.73, p < 0.001) were associated with a more positive attitude towards PC. More training in PC (β = −2.70, p = 0.003) and a higher sense of ownership over PC issues (β = −0.51, p = 0.001) were associated with a more negative attitude towards subspecialty PC. These findings highlight barriers to pediatric HCT and PC collaboration, including concerns about PC team knowledge of HCT and patient perceptions. While most pediatric transplant physicians trust PC to enhance patient care, interventions are needed to improve collaboration.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Parsons SK, Tighiouart H, Terrin N. Assessment of health-related quality of life in pediatric hematopoietic stem cell transplant recipients: progress, challenges and future directions. Expert Rev Pharmacoecon Outcomes Res [Internet]. 2013;13:217.
Bense JE, Haverman L, von Asmuth EGJ, Louwerens M, Luijten MAJ, Stiggelbout AM, et al. Late effects in pediatric allogeneic hematopoietic stem cell transplantation for nonmalignant diseases: proxy- and patient-reported outcomes. Transpl Cell Ther [Internet]. 2023;29:186.e1–186.e10.
Eriksson LV, Holmberg K, Lundh Hagelin C, Wengström Y, Bergkvist K, Winterling J. Symptom burden and recovery in the first year after allogeneic hematopoietic stem cell transplantation. Cancer Nurs [Internet]. 2023;46:77–85.
Pidala J, Anasetti C, Jim H. Quality of life after allogeneic hematopoietic cell transplantation. Blood. 2009;114:7–19.
Bevans M, El-Jawahri A, Tierney DK, Wiener L, Wood WA, Hoodin F, et al. National Institutes of Health hematopoietic cell transplantation late effects initiative: the patient-centered outcomes Working Group Report. Biol Blood Marrow Transpl. 2017;23:538–51.
Phipps S, Dunavant M, Lensing S, Rai SN. Acute health-related quality of life in children undergoing stem cell transplant: II. Medical and demographic determinants. Bone Marrow Transpl. 2002;29:435–42.
Phipps S, Dunavant M, Garvie PA, Lensing S, Rai SN. Acute health-related quality of life in children undergoing stem cell transplant: I. Descriptive outcomes. Bone Marrow Transpl. 2002;29:425–34.
Feudtner C, Friebert S, Jewell J. Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013;132:966–72.
Dans M, Kutner JS, Agarwal R, Baker JN, Bauman JR, Beck AC, et al. NCCN Guidelines® Insights: Palliative Care, Version 2.2021: Featured Updates to the NCCN Guidelines. J Natl Compr Cancer Netw [Internet]. 2021;19:780–8.
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N. Engl J Med [Internet]. 2010;363:733–42.
Bakitas MA, Tosteson TD, Li Z, Lyons KD, Hull JG, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33:1438–45.
Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet [Internet]. 2014;383:1721–30.
Ferrell BR, Temel JS, Temin S, Smith TJ. Integration of palliative care into standard oncology care: ASCO clinical practice guideline update summary. J Oncol Pr. 2017;13:119–21.
Sanders JJ, Temin S, Ghoshal A, Alesi ER, Ali ZV, Chauhan C, et al. Palliative Care for Patients With Cancer: ASCO Guideline Update. [Internet]. 2024 May 15 [cited 2024 May 20]; Available from: https://doi.org/10.1200/JCO.24.00542.
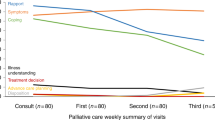
El-Jawahri A, Le BlancT, Van DusenH, Traeger L, Greer JA, Pirl WF, et al. Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: a randomized clinical trial. JAMA. 2016;316:2094–103.
El-Jawahri A, Traeger L, Greer JA, Van DusenH, Fishman SR, Pirl WF, et al. Effect of inpatient palliative care during hematopoietic stem-cell transplant on psychological distress 6 months after transplant: Results of a randomized clinical trial. J Clin Oncol. 2017;35:3714–21.
Phelan R, Chen M, Bupp C, Bolon YT, Broglie L, Brunner-Grady J, et al. Updated trends in hematopoietic cell transplantation in the united states with an additional focus on adolescent and young adult transplantation activity and outcomes. Transpl Cell Ther. 2022;28:409.e1–409.e10.
Armenian SH, Sun CL, Kawashima T, Arora M, Leisenring W, Sklar CA, et al. Long-term health-related outcomes in survivors of childhood cancer treated with HSCT versus conventional therapy: a report from the bone marrow transplant survivor study (BMTSS) and childhood Cancer survivor study (CCSS). Blood. 2011;118:1413–20.
Ward J, Smith J, Powers K, Hellsten M, Murray P Parent psychological distress is associated with symptom burden and health-related quality of life in children and adolescents undergoing stem cell transplantation or chimeric antigen receptor T cell therapy. Transplant Cell Ther. 2023.
Ullrich CK, Rodday AM, Bingen K, Kupst MJ, Patel SK, Syrjala KL, et al. Parent outlook: how parents view the road ahead as they embark on hematopoietic stem cell transplantation for their child. Biol Blood Marrow Transpl. 2016;22:104–11. https://doi.org/10.1016/j.bbmt.2015.08.040.
Bense JE, Stiggelbout AM, Lankester AC, de Pagter APJ. Long-term parental distress after pediatric hematopoietic stem cell transplantation for nonmalignant diseases. Pediatr Blood Cancer. 2023;70:e30638.
Levine DR, Mandrell BN, Sykes A, Pritchard M, Gibson D, Symons HJ, et al. Patients’ and parents’ needs, attitudes, and perceptions about early palliative care integration in pediatric oncology. JAMA Oncol. 2017;3:1214–20.
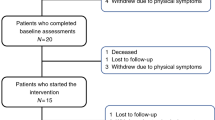
Lafond DA, Kelly KP, Hinds PS, Sill A, Michael M. Establishing feasibility of early palliative care consultation in pediatric hematopoietic stem cell transplantation. J Pediatr Oncol Nurs. 2015;32:265–77.
Fraint E, Abdel-Azim H, Bhatt NS, Broglie L, Chattha A, Kohorst M, et al. Evaluation of children with malignancies for blood and marrow transplantation: A Report from the ASTCT Committee on Practice Guidelines. Transpl Cell Ther. 2023;29:293–301.
Levine DR, Baker JN, Wolfe J, Lehmann LE, Ullrich C. Strange bedfellows no more: How integrated stem-cell transplantation and palliative care programs can together improve end-of-life care. J Oncol Pr. 2017;13:569–77.
Collins GS, Beaman H, Ho AM, Hermiston ML, Cohen HJ, Dzeng EW. Perceptions of specialty palliative care and its role in pediatric stem cell transplant: A multidisciplinary qualitative study. Pediatr Blood Cancer. 2022;69:e29424
Manitta VJ, Philip JAM, Cole-Sinclair MF. Palliative care and the hemato-oncological patient: can we live together? A review of the literature. J Palliat Med. 2010;13:1021–5.
El-Jawahri A, LeBlanc TW, Burns LJ, Denzen E, Meyer C, Mau LW, et al. What do transplant physicians think about palliative care? A national survey study. Cancer. 2018;124:4556–66.
Cherny NI, Catane R Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survey by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer [Internet]. 2003 Dec 1 [cited 2024 Feb 20];98:2502–10. Available from: https://pubmed-ncbi-nlm-nih-gov.offcampus.lib.washington.edu/14635087/.
Fadul N, Elsayem A, Palmer JL, Del Fabbro E, Swint K, Li Z, et al. Supportive versus palliative care: what’s in a name? A survey of medical oncologists and midlevel providers at a comprehensive. Cancer Cent Cancer [Internet]. 2009;115:2013–21.
Milne D, Aranda S, Jefford M, Schofield P. Development and validation of a measurement tool to assess perceptions of palliative care. Psychooncology. 2013;22:940–6.
Buzgova R, Kozakova R, Sikorova L, Zelenikova R, Jarosova D. Development and psychometric evaluation of patient needs assessment in palliative care (PNAP) instrument. Palliat Support Care. 2016;14:129–37.
Johnsen AT, Petersen MA, Pedersen L, Groenvold M. Development and initial validation of the Three-Levels-of-Needs Questionnaire for self-assessment of palliative needs in patients with cancer. J Pain Symptom Manag. 2011;41:1025–39.
Hui D, Park M, Liu D, Reddy A, Dalal S, Bruera E. Attitudes and beliefs toward supportive and palliative care referral among hematologic and solid tumor oncology specialists. Oncologist. 2015;20:1326–32.
Ward AM, Agar M, Koczwara B. Collaborating or co-existing: A survey of attitudes of medical oncologists toward specialist palliative care. Palliat Med. 2009;23:698–707.
Ullrich CK, Dussel V, Hilden JM, Sheaffer JW, Lehmann L, Wolfe J. End-of-life experience of children undergoing stem cell transplantation for malignancy: parent and provider perspectives and patterns of care. Blood. 2010;115:3879–85.
Snaman JM, Kaye EC, Lu JJ, Sykes A, Baker JN. Palliative care involvement is associated with less intensive end-of-life care in adolescent and young adult oncology patients. J Palliat Med. 2017;20:509–16.
Levine DR, Epperly R, Collins G, Talleur AC, Mandrell B, Pritchard M, et al. Integration of palliative care in hematopoietic cell transplant: pediatric patient and parent needs and attitudes. J Pain Symptom Manag. 2023;66:248–57.
Mekelenkamp H, Schröder T, Trigoso E, Hutt D, Galimard J-E, Kozijn A, et al. Specialized pediatric palliative care services in pediatric hematopoietic stem cell transplant centers. Child (Basel, Switzerland) [Internet]. 2021 Jul 21 [cited 2022 Jun 5];8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/34438506.
Santivasi WL, Childs DS, Wu KL, Partain DK, Litzow MR, Leblanc TW, et al. Perceptions of Hematology Among Palliative Care Physicians: Results of a Nationwide Survey Key Message. J Pain Symptom Manage [Internet]. 2021 [cited 2024 Apr 23];62. Available from: https://doi.org/10.1016/j.jpainsymman.2021.04.021.
Laronne A, Granek L, Wiener L, Feder-Bubis P, Golan H. Organizational and individual barriers and facilitators to the integration of pediatric palliative care for children: A grounded theory study. Palliat Med. 2021;35:1612–24.
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, et al. Pediatric palliative care programs in children’s hospitals: a cross-sectional national survey. Pediatrics [Internet]. 2013;132:1063–70.
Rogers MM, Friebert S, Williams CSP, Humphrey L, Thienprayoon R, Klick JC Pediatric palliative care programs in US hospitals. Pediatrics. 2021;148.
Autrey AK, James C, Sarvode Mothi S, Stafford C, Morvant A, Miller EG, et al. The landscape of outpatient pediatric palliative care: a national cross-sectional assessment. J Pain Symptom Manag. 2023;66:1–23.
Dalal S, Palla S, Hui D, Nguyen L, Chacko R, Li Z, et al. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist. 2011;16:105–11.
Barata A, Abrams HR, Meyer C, Mau L-W, Mattila D, Burns LJ, et al. What do patients think about palliative care? A national survey of hematopoietic stem cell transplant recipients. Blood Adv. 2023;7:2032–41.
Salins N, Ghoshal A, Hughes S, Preston N. How views of oncologists and haematologists impacts palliative care referral: a systematic review. BMC Palliat Care. 2020;19:1–19.
Dalberg T, McNinch NL, Friebert S. Perceptions of barriers and facilitators to early integration of pediatric palliative care: A national survey of pediatric oncology providers. Pediatr Blood Cancer]. 2018;65:e26996.
Holder P, Coombes L, Chudleigh J, Harding R, Fraser LK. Barriers and facilitators influencing referral and access to palliative care for children and young people with life-limiting and life-threatening conditions: a scoping review of the evidence. Palliat Med. 2024;38:981.
Niehaus JZ, Palmer MM, Slaven J, Hatton A, Scanlon C, Hill AB. Neonatal palliative care: perception differences between providers. J Perinatol. 2020;40:1802–8.
Levine A, Winn PA, Fogel AH, Lelkes E, McPoland P, Agrawal AK, et al. Barriers to pediatric palliative care: trainee and faculty perspectives across two academic centers. J Palliat Med. 2023;26:1348–56.
Knapp C, Thompson L Factors associated with perceived barriers to pediatric palliative care: a survey of pediatricians in Florida and California. https://doi.org/10.1177/0269216311409085 [Internet]. 2011 Jun 16 [cited 2025 Jan 24];26:268–74. Available from: https://journals.sagepub.com/doi/10.1177/0269216311409085?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed.
Balkin EM, Kirkpatrick JN, Kaufman B, Swetz KM, Sleeper LA, Wolfe J, et al. Pediatric cardiology provider attitudes about palliative care: a multicenter survey study. Pediatr Cardiol. 2017;38:1324–31.
Szymczak JE, Schall T, Hill DL, Walter JK, Parikh S, DiDomenico C, et al. Pediatric oncology providers’ perceptions of a palliative care service: the influence of emotional esteem and emotional labor. J Pain Symptom Manag. 2018;55:1260–8.
Baker JN, Torkildson C, Baillargeon JG, Olney CA, Kane JR. National survey of pediatric residency program directors and residents regarding education in palliative medicine and end-of-life care. J Palliat Med. 2007;10:420–9.
Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77:1121–34.
Gude T, Finset A, Anvik T, Bærheim A, Fasmer OB, Grimstad H, et al. Do medical students and young physicians assess reliably their self-efficacy regarding communication skills? A prospective study from end of medical school until end of internship. BMC Med Educ [Internet]. 2017 Jun 30 [cited 2024 Mar 14];17. Available from: https://pubmed.ncbi.nlm.nih.gov/28666440/.
Rahmani M. Medical trainees and the Dunning-Kruger effect: when they don’t know what they don’t know. J Grad Med Educ. 2020;12:532–4.
DeCarli K, Rodenbach R, Sedhom R, Von Roenn J, Ketterer B. Integrated dual training in palliative care and oncology. Curr Probl Cancer. 2023;47:101012.
Sedhom R, Gupta A, Kamal AH. Case for dual training in medical oncology and palliative care. 2020 May 19 [cited 2024 Apr 23];16:537–9. Available from: https://doi.org/10.1200/OP.20.00137.
Acknowledgements
ECM was supported in part by National Institutes of Health training grants (T32CA009351 and T32HL125195). AEJ and TWL are Scholars in Clinical Research for the Leukemia and Lymphoma Society. The opinions herein represent those of the authors and not necessarily those of their funders.
Author information
Authors and Affiliations
Contributions
CLM, TWL, and AEJ contributed to the study conception, design, and acquisition of data. CLM was responsible for data analysis and the creation of tables and figures. ECM, CLM, RAY, CKU, and AEJ contributed to the interpretation of data. The first draft of the manuscript and reference list were written by ECM. All authors (ECM, CLM, RAF, CFM, DLK, DRL, TWL, CKU, and AEJ) provided feedback, contributed to critical revisions, and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was determined to be exempt by the institutional review board of NMDP (formerly known as the National Marrow Donor Program; IRB-2016-0374). All methods were performed in accordance with relevant guidelines and regulations. Participation was voluntary, and survey completion indicated informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merkel, E.C., Meyer, C.L., Yusuf, R.A. et al. What do pediatric transplant physicians think about palliative care? Results from a national survey study. Bone Marrow Transplant 60, 1129–1136 (2025). https://doi.org/10.1038/s41409-025-02597-z
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02597-z