Abstract
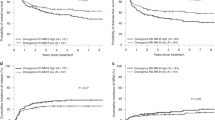
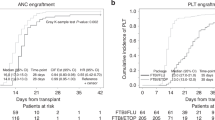
Matching HLA between donor and recipient pairs significantly improves engraftment and decreases GvHD. However, even in HLA matched siblings, the risk of graft failure and GvHD still exist and is partially attributed to the bidirectional alloreactivity generated from minor histocompatibility antigens (miHA) mismatching between donors and recipients. Consanguineous marriage increases the chance of miHA matching. This fact may be an advantage or disadvantage in consanguineous MSD transplants. We retrospectively reviewed our institutional transplant registry and selected AML and ALL patients who received a MSD allo-HCT between January 2006 and December 2020. The objective was to compare the outcomes of transplant among consanguineous vs non-consanguineous pairs. Analysis was conducted using RStudio. Version 1.4.1106 © 2009-2021 RStudio, PBC. 271 patients met the eligibility criteria were included in this study. Sixty-three were consanguineous and 208 were not. The median follow-up time was 72.6 months. The five years OS and DFS were not statistically different between consanguineous and non-consanguineous group. A trend toward a higher relapse rate in the consanguineous group was observed. The five years NRM for the whole group was 10.5% with no statistically significant difference between groups. The grade II-IV aGvHD incidence was 25.8% for the whole group with no statistically significant difference between groups. The all grade cGvHD incidence was 52.8% with no statistically significant difference between groups. Populations with high levels of consanguinity, complex consanguinity loops often arise from cousin marriages across multiple generations. This means that even individuals who consider themselves non-consanguineous may still share genetic traits associated with consanguinity. Therefore, high level of homozygosity probably exist in the non-consanguineous cohort and explain these results.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available upon request.
References
Bittles AH, Black ML. Consanguinity, human evolution, and complex diseases. Proc Natl Acad Sci. 2010;107:1779–86.
Modell B, Darr A. Genetic counselling and customary consanguineous marriage. Nat Rev Genet. 2002;3:225–9.
Bittles AH. Consanguinity, genetic drift, and genetic diseases in populations with reduced numbers of founders. In: Vogel and Motulsky’s Human Genetics. Springer, pp 507-28 (2010).
El-Hazmi M, Al-Swailem A, Warsy A, Al-Swailem A, Sulaimani R, Al-Meshari A. Consanguinity among the Saudi Arabian population. J Med Genet. 1995;32:623–6.
Merten M. Keeping it in the family: consanguineous marriage and genetic disorders, from Islamabad to Bradford. BMJ: Br Med J (Online). 2019;365:l1851.
Corry PC. Consanguinity and prevalence patterns of inherited disease in the UK Pakistani community. Hum Heredity. 2014;77:207–16.
Hamamy H. Consanguineous marriages. J Community Genet. 2012;3:185–92.
Hamamy H, Antonarakis SE, Cavalli-Sforza LL, Temtamy S, Romeo G, Ten Kate LP, et al. Consanguineous marriages, pearls and perils: Geneva international consanguinity workshop report. Genet Med. 2011;13:841–7.
Bittles AH, Mason WM, Greene J, Rao NA. Reproductive behavior and health in consanguineous marriages. Science. 1991;252:789–94.
Jaber L, Halpern GJ, Shohat M. The impact of consanguinity worldwide. Public Health Genomics. 1998;1:12–7.
Bennett RL, Motulsky AG, Bittles A, Hudgins L, Uhrich S, Doyle DL, et al. Genetic counseling and screening of consanguineous couples and their offspring: Recommendations of the National Society of Genetic Counselors. J Genet Couns. 2002;11:97–119.
Thomas ED, Blume KG. Historical markers in the development of allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transpl. 1999;5:341–6.
Martin P, Gooley T, Anasetti C, Petersdorf E, Hansen J. HLAs and risk of acute graft-vs.-host disease after marrow transplantation from an HLA-identical sibling. Biol Blood Marrow Transpl. 1998;4:128–33.
Pei J, Martin P, Longton G, Masewicz S, Mickelson E, Petersdorf E, et al. Evaluation of pretransplant donor anti-recipient cytotoxic and helper T lymphocyte responses as correlates of acute graft-vs.-host disease and survival after unrelated marrow transplantation. J Am Soc Blood Marrow Transpl. 1997;3:142–9.
Progress in bone marrow transplantation for leukemia: a preliminary report from the Advisory Committee of the International Bone Marrow Transplant Registry. Transplantation proceedings, (1991).
Martin P. Increased disparity for minor histocompatibility antigens as a potential cause of increased GVHD risk in marrow transplantation from unrelated donors compared with related donors. Bone marrow Transpl. 1991;8:217–23.
Beatty P, Hervé P. Immunogenetic factors relevant to acute graft-versus-host disease. Graft-versus-host disease: immunology. Pathophysiol Treat. 1990;12:415.
Chao N. Treatment of acute GVHD. Graft versus host disease. 2nd ed. Austin (TX): RG Landes Co 1999: 103-8.
Korngold R, Sprent J. Lethal graft-versus-host disease after bone marrow transplantation across minor histocompatibility barriers in mice. Prevention by removing mature T cells from marrow. J Exp Med. 1978;148:1687–98.
Korngold R, Sprent J. Variable capacity of L3T4+ T cells to cause lethal graft-versus-host disease across minor histocompatibility barriers in mice. J Exp Med. 1987;165:1552–64.
Martin PJ, Levine DM, Storer BE, Warren EH, Zheng X, Nelson SC, et al. Genome-wide minor histocompatibility matching as related to the risk of graft-versus-host disease. Blood J Am Soc Hematol. 2017;129:791–8.
Vincent K, Roy D-C, Perreault C. Next-generation leukemia immunotherapy. Blood J Am Soc Hematol. 2011;118:2951–9.
Chao NJ, Schmidt GM, Niland JC, Amylon MD, Dagis AC, Long GD, et al. Cyclosporine, methotrexate, and prednisone compared with cyclosporine and prednisone for prophylaxis of acute graft-versus-host disease. N. Engl J Med. 1993;329:1225–30.
Przepiorka D, Weisdorf D, Martin P, Klingemann H, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone marrow Transpl. 1995;15:825.
Sullivan KM. Acute and chronic graft‐versus‐host disease in man. Int J Cell Cloning. 1986;4:42–93.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014; 123: 3664-71. e-pub ahead of print 2014/04/20; https://doi.org/10.1182/blood-2014-01-552984
Goulmy E, Schipper R, Pool J, Blokland E, Falkenburg F, Vossen J, et al. Mismatches of minor histocompatibility antigens between HLA-identical donors and recipients and the development of graft-versus-host disease after bone marrow transplantation. N. Engl J Med. 1996;334:281–5.
Cieri N, Hookeri N, Stromhaug K, Li L, Keating J, Díaz-Fernández P, et al. Systematic identification of minor histocompatibility antigens predicts outcomes of allogeneic hematopoietic cell transplantation. Nat Biotechnol. 2024. https://doi.org/10.1038/s41587-024-02348-3.
Niederwieser D, Grassegger A, Aubock J, Herold M, Nachbaur D, Rosenmayr A, et al. Correlation of minor histocompatibility antigen-specific cytotoxic T lymphocytes with graft-versus-host disease status and analyses of tissue distribution of their target antigens. Blood. 1993;81:2200-8.
Bittles AH. Consanguinity and its relevance to clinical genetics. Clin Genet. 2001;60:89–98.
Fuchs KJ, van de Meent M, Honders MW, Khatri I, Kester MG, Koster EA, et al. Expanding the repertoire reveals recurrent, cryptic, and hematopoietic HLA class I minor histocompatibility antigens. Blood. 2024;143:1856–72.
Author information
Authors and Affiliations
Contributions
RE designed the research and wrote the first draft. MIS, SA, SS, AA, YA collected the data. TE analyzed the data. All the co-authors (SA, FA, SA, SOA, MS, NC, FA, AH, AS, AA, AA, MA, AAA, HA, ASA, FA, AA, GM, WR, HA, MA) revised the initial draft and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
El Fakih, R., Sharif, M.I., Alotaibi, S. et al. Outcomes of human leukocyte antigen matched sibling transplant from consanguineous versus non-consanguineous parents, a single center experience. Bone Marrow Transplant 60, 1108–1113 (2025). https://doi.org/10.1038/s41409-025-02609-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02609-y