Abstract
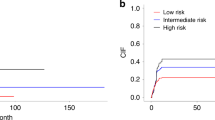
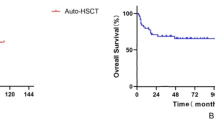
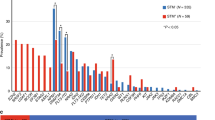
Central nervous system(CNS) is a common site of extramedullary involvement after allogeneic hematopoietic stem cell transplantation(allo-HSCT). It may confer inferior survival when combined with bone marrow(BM) relapse in leukemia patients. We performed a retrospective study to investigate the associated risk factors and prognosis in adult patients with post-transplant CNS relapse. Between 2016 and 2024 in our center, 74 leukemia patients developed CNS relapse after allo-HSCT, with 23 cases of isolated CNS(iCNS) relapse and 51 cases of combined CNS and BM(CNS&BM) relapse. Patients with CNS&BM relapse after allo-HSCT conferred inferior 5-year overall survival (OS) compared with those with iCNS relapse, and independent risk factors related with CNS&BM relapse were identified, including male gender(relative risk ratio[RR] = 4.09, 95% confidence interval [CI] = 1.29–13.02, p = 0.017), HLA-identical transplantation (RR = 4.11, 95% CI = 1.10–15.32, p = 0.035), and without chronic graft-versus-host disease occurrence (RR = 3.73, 95% CI = 1.00–13.84, p = 0.049). Early CNS relapse was identified as an independent predictor of worse 5-year OS from HSCT for patients with CNS&BM relapse (n = 51, <12 months after allo-HSCT, hazard ratio=7.35, p = 0.003). Systemic therapy after CNS relapse reduced subsequent BM relapse for ALL and CML patients (p = 0.038). These findings demonstrate the outcome of patients with post-transplant CNS&BM relapse remains very poor. HLA-haploindentical allo-HSCT and systemic therapy after CNS relapse may better reduce BM relapse.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data supporting the findings are not publicly available due to privacy or ethical restrictions. The data are available upon reasonable request from the corresponding author.
References
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M, et al. The consensus from The Chinese Society of Hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol. 2021;14:145. https://doi.org/10.1186/s13045-021-01159-2.
Sauerer T, Velázquez GF, Schmid C. Relapse of acute myeloid leukemia after allogeneic stem cell transplantation: immune escape mechanisms and current implications for therapy. Mol Cancer. 2023;22:180. https://doi.org/10.1186/s12943-023-01889-6.
D’Souza A, Fretham C, Lee SJ, Arora M, Brunner J, Chhabra S, et al. Current Use Of And Trends In Hematopoietic Cell Transplantation in the United States. Biol Blood Marrow Transpl. 2020;26:e177–e182. https://doi.org/10.1016/j.bbmt.2020.04.013.
Horowitz M, Schreiber H, Elder A, Heidenreich O, Vormoor J, Toffalori C, et al. Epidemiology and biology of relapse after stem cell transplantation. Bone Marrow Transpl. 2018;53:1379–89. https://doi.org/10.1038/s41409-018-0171-z.
Oshima K, Kanda Y, Yamashita T, Takahashi S, Mori T, Nakaseko C, et al. Central nervous system relapse of leukemia after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2008;14:1100–7. https://doi.org/10.1016/j.bbmt.2008.07.002.
Hamdi A, Mawad R, Bassett R, di Stasi A, Ferro R, Afrough A, et al. Central nervous system relapse in adults with acute lymphoblastic leukemia after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2014;20:1767–71. https://doi.org/10.1016/j.bbmt.2014.07.005.
Chen Q, Zhu XL, Zhao X, Liu X, Fu HX, Zhang YY, et al. Prognosis and risk factors for central nervous system relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia. Ann Hematol. 2021;100:505–16. https://doi.org/10.1007/s00277-020-04380-0.
Blum S, Chalandon Y, Labopin M, Finke J, Gedde-Dahl T, Othman TB, et al. Incidence and outcome of central nervous system relapse after hematopoietic stem cell transplantation in patients suffering from acute myeloid leukemia and acute lymphoblastic leukemia: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2024;109:2346–50. https://doi.org/10.3324/haematol.2023.284858.
Lee JH, Yoon J-H, Kwag D, Min G-J, Park S-S, Park S, et al. Incidence and risk factors for central nervous system relapse after allogeneic hematopoietic stem cell transplantation in adult patients with acute lymphoblastic leukemia. Blood. 2023;142:2210–2210. https://doi.org/10.1182/blood-2023-181540.
Thompson CB, Sanders JE, Flournoy N, Buckner CD, Thomas ED. The risks of central nervous system relapse and leukoencephalopathy in patients receiving marrow transplants for acute leukemia. Blood. 1986;67:195–9.
Dargenio M, Bonifacio M, Chiaretti S, Vitale A, Fracchiolla NS, Papayannidis C, et al. Incidence, treatment and outcome of central nervous system relapse in adult acute lymphoblastic leukaemia patients treated front-line with paediatric-inspired regimens: A retrospective multicentre Campus ALL study. Br J Haematol. 2023;200:440–50. https://doi.org/10.1111/bjh.18537.
Hu LJ, Fu GM, Zhang YY, Wang YZ, Qin YZ, Lai YY, et al. Cytology or multiparameter flow cytometry positivity in the cerebrospinal fluid before transplantation is predictive of poor outcomes after allotransplantation in acute myeloid leukemia patients. Clin Transpl. 2024;38:e15396. https://doi.org/10.1111/ctr.15396.
Huang R, Wang X, Zhang X. Unity brings strength: combination of CAR-T cell therapy and HSCT. Cancer Lett. 2022;549:215721. https://doi.org/10.1016/j.canlet.2022.215721.
Wang Y, Chang YJ, Chen J, Han M, Hu J, Hu J, et al. Consensus on the monitoring, treatment, and prevention of leukaemia relapse after allogeneic haematopoietic stem cell transplantation in China: 2024 update. Cancer Lett. 2024;605:217264. https://doi.org/10.1016/j.canlet.2024.217264.
Mo XD, Lv M, Huang XJ. Preventing relapse after haematopoietic stem cell transplantation for acute leukaemia: the role of post-transplantation minimal residual disease (MRD) monitoring and MRD-directed intervention. Br J Haematol. 2017;179:184–97. https://doi.org/10.1111/bjh.14778.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood. 2015;125:3956–62. https://doi.org/10.1182/blood-2015-02-627786.
Wang Y, Liu QF, Wu DP, Xu ZL, Han TT, Sun YQ, et al. Mini-dose methotrexate combined with methylprednisolone for the initial treatment of acute GVHD: a multicentre, randomized trial. BMC Med. 2024;22:176. https://doi.org/10.1186/s12916-024-03395-y.
van den Brink MR, Porter DL, Giralt S, Lu SX, Jenq RR, Hanash A, et al. Relapse after allogeneic hematopoietic cell therapy. Biol Blood Marrow Transpl. 2010;16:S138–145. https://doi.org/10.1016/j.bbmt.2009.10.023.
Liu S, Luo X, Zhang X, Xu L, Wang Y, Yan C, et al. Preemptive interferon-α treatment could protect against relapse and improve long-term survival of ALL patients after allo-HSCT. Sci Rep. 2020;10:20148. https://doi.org/10.1038/s41598-020-77186-9.
Gao L, Zhang Y, Wang S, Kong P, Su Y, Hu J, et al. Effect of rhG-CSF combined with decitabine prophylaxis on relapse of patients with high-risk MRD-negative AML after HSCT: an open-label, multicenter, randomized controlled trial. J Clin Oncol. 2020;38:4249–59. https://doi.org/10.1200/jco.19.03277.
Ozga M, Nicolet D, Mrózek K, Yilmaz AS, Kohlschmidt J, Larkin KT, et al. Sex-associated differences in frequencies and prognostic impact of recurrent genetic alterations in adult acute myeloid leukemia (Alliance, AMLCG). Leukemia. 2024;38:45–57. https://doi.org/10.1038/s41375-023-02068-8.
Savino AM, Fernandes SI, Olivares O, Zemlyansky A, Cousins A, Markert EK, et al. Metabolic adaptation of acute lymphoblastic leukemia to the central nervous system microenvironment is dependent on Stearoyl CoA desaturase. Nat Cancer. 2020;1:998–1009. https://doi.org/10.1038/s43018-020-00115-2.
Kim SJ, Choi H, Park SS, Chang C, Kim E. Stearoyl CoA desaturase (SCD) facilitates proliferation of prostate cancer cells through enhancement of androgen receptor transactivation. Mol Cells. 2011;31:371–7. https://doi.org/10.1007/s10059-011-0043-5.
Kaphan E, Bettega F, Forcade E, Labussière-Wallet H, Fegueux N, Robin M, et al. Late relapse after hematopoietic stem cell transplantation for acute leukemia: a retrospective study by SFGM-TC. Transpl Cell Ther. 2023;29:362.e361–362.e312. https://doi.org/10.1016/j.jtct.2023.02.020.
Weisdorf D, Zhang MJ, Arora M, Horowitz MM, Rizzo JD, Eapen M. Graft-versus-host disease induced graft-versus-leukemia effect: greater impact on relapse and disease-free survival after reduced intensity conditioning. Biol Blood Marrow Transpl. 2012;18:1727–33. https://doi.org/10.1016/j.bbmt.2012.06.014.
Storb R, Gyurkocza B, Storer BE, Sorror ML, Blume K, Niederwieser D, et al. Graft-versus-host disease and graft-versus-tumor effects after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2013;31:1530–8. https://doi.org/10.1200/jco.2012.45.0247.
Yeshurun M, Weisdorf D, Rowe JM, Tallman MS, Zhang MJ, Wang HL, et al. The impact of the graft-versus-leukemia effect on survival in acute lymphoblastic leukemia. Blood Adv. 2019;3:670–80. https://doi.org/10.1182/bloodadvances.2018027003.
Ostronoff M, Domingues MC, Ostronoff F, Matias C, Florêncio R, Matias K, et al. Reduced intensity conditioning allogeneic bone marrow transplantation following central nervous system (CNS) relapse of acute promyelocytic leukemia: evidence for a graft-versus-leukemia effect in the CNS. Am J Hematol. 2006;81:387–8. https://doi.org/10.1002/ajh.20616.
Classen CF, Debatin KM, Friedrich W, Schulz AS. Long-term remission of APL with a second allogeneic BMT after CNS relapse following HLA-identical allogeneic BMT. Bone Marrow Transpl. 2003;32:843–6. https://doi.org/10.1038/sj.bmt.1704225.
Sparber-Sauer M, Hönig M, Schulz AS, zur Stadt U, Schütz C, Debatin KM, et al. Patients with early relapse of primary hemophagocytic syndromes or with persistent CNS involvement may benefit from immediate hematopoietic stem cell transplantation. Bone Marrow Transplant. 2009;44:333–8. https://doi.org/10.1038/bmt.2009.34.
Kopmar NE, Cassaday RD. How I prevent and treat central nervous system disease in adults with acute lymphoblastic leukemia. Blood. 2023;141:1379–88. https://doi.org/10.1182/blood.2022017035.
Barredo JC, Devidas M, Lauer SJ, Billett A, Marymont M, Pullen J, et al. Isolated CNS relapse of acute lymphoblastic leukemia treated with intensive systemic chemotherapy and delayed CNS radiation: a pediatric oncology group study. J Clin Oncol. 2006;24:3142–9. https://doi.org/10.1200/jco.2005.03.3373.
Jabbour E, Guastad Daver N, Short NJ, Huang X, Chen HC, Maiti A, et al. Factors associated with risk of central nervous system relapse in patients with non-core binding factor acute myeloid leukemia. Am J Hematol. 2017;92:924–8. https://doi.org/10.1002/ajh.24799.
Funding
This work was partly supported by the National Key Research and Development Program of China (No. 2023YFC2508905), the National Natural Science Foundation of China (82470214 & 82270227 & 82200240), Major Program of the National Natural Science Foundation of China (No. 82293630), Beijing Municipal Science & Technology Commission (No. Z211100002921071), Peking University Medicine Fund for world’s leading discipline or discipline cluster development (No.71003Y3035).
Author information
Authors and Affiliations
Contributions
YW and XJH conceived, designed the study. YW supervised the manuscript preparation. LPG collected patient data with the help of LJH, XDM, YQS, YFC, LPX, XHZ. LPG performed data analysis and wrote the manuscript under supervision of YW. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, Lp., Hu, Lj., Mo, Xd. et al. Characteristics and prognosis of central nervous system relapse after allogeneic hematopoietic stem cell transplantation in adult patients with leukemia. Bone Marrow Transplant 60, 1333–1343 (2025). https://doi.org/10.1038/s41409-025-02673-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02673-4