Abstract
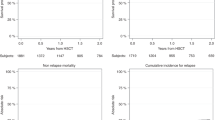
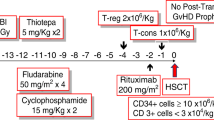
Acute leukemias are prevalent among children and adolescents, with survival rates exceeding 90%, but high-risk cases often require hematopoietic stem cell transplantation (HSCT). Limited data are available on HSCT outcomes for pediatric acute lymphoblastic leukemia (ALL) in low- and middle-income countries. This Brazilian multicenter retrospective cohort study analyzed outcomes of ALL patients aged up to 18 years who underwent HSCT from January 2010 to June 2020. A total of 439 patients were included (69% male, 78.9% B-ALL). Unrelated donor transplants accounted for 49.9%, and haploidentical transplants for 18.9%. Bone marrow (82.6%) was the predominant stem cell source. Transplants occurred in the first or second complete remission (CR) in 38.7% and 44.2% of cases, respectively. The 100-day cumulative incidence of acute GvHD was 46.1%, and chronic GvHD after 100 days occurred in 25.5%. At five years, overall survival and event-free survival were 52.4% and 51.7%. By day +100, sepsis was the leading cause of mortality (42.3%), whereas relapse accounted for 76.3% of deaths thereafter. Findings align with HSCT literature, demonstrating similar outcomes despite challenges in developing countries and providing a basis for further research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Wayne AS, Baird K, Egeler RM. Hematopoietic stem cell transplantation for leukemia. Pediatr Clin North Am. 2010;57:1–25.
Inaba H, Pui CH. Immunotherapy in pediatric acute lymphoblastic leukemia. Cancer Metastasis Rev. 2019;38:595–610.
National Cancer Institute (NIH): Cancer in Children and Adolescents. 2023 Sep. Available from: https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet. [Accessed 2023 Oct 16].
Da Silva FF, De Oliveira Latorre MDRD Survival from acute lymphocytic leukemia in children in the city of São Paulo, Brazil. Public Health J. 2020;36. https://doi.org/10.1590/0102-311X00008019.
Silva KA, de S, Spagnol F, Farias MG, Alegretti AP, Michalowski MB, et al. Influence of minimal residual disease by multiparametric flow cytometry at day 15 of induction in risk stratification of children with B-cell acute lymphoblastic leukemia treated at a referral hospital in southern Brazil. Hematol Transfus Cell Ther. 2020;42:348–55.
Michalowski MB, Cecconello DK, Lins MM, Carvalho MPSS, Silva KA, de S, et al. Influence of different asparaginase formulations in the prognosis of children with acute lymphocytic leukaemia in Brazil: a multicentre, retrospective controlled study. Br J Haematol. 2021;194:168–73.
Tavares RCB, Bonfim CS, Seber A, Pereira Lermontov S, Coulturato V, Zecchin VG, et al. Hematopoietic cell transplantation in pediatric patients with acute leukemias or myelodysplastic syndrome using unrelated adult or umbilical cord blood donors in Brazil. Pediatr Transplant. 2020;24.
Anasetti C. What are the most important donor and recipient factors affecting the outcome of related and unrelated allogeneic transplantation? Best Pr Res Clin Haematol. 2008;21:691–7.
Kato M, Kurata M, Kanda J, Kato K, Tomizawa D, Kudo K, et al. Impact of graft-versus-host disease on relapse and survival after allogeneic stem cell transplantation for pediatric leukemia. Bone Marrow Transpl. 2019;54:68–75.
Algeri M, Merli P, Locatelli F, Pagliara D The role of allogeneic hematopoietic stem cell transplantation in pediatric leukemia. J Clin Med. 2021;10.
Silla L, Fischer GB, Paz A, Daudt LE, Mitto I, Katz B, et al. Patient socioeconomic status as a prognostic factor for allo-SCT. Bone Marrow Transpl. 2009;43:571–7. https://doi.org/10.1038/bmt.2008.358. Epub 2008 Nov 3. PMID: 18978820
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. diagnosis and staging working group report. Biol Blood Marrow Transpl. 2005;11:945–56.
Rowlings PA, Przepiorka D, Klein JP, Gale RP, Passweg JR, Henslee-Downey PJ, et al. IBMTR Severity Index for grading acute graft-versus-host disease: Retrospective comparison with Glucksberg grade. Br J Haematol. 1997;97:855–64.
Van Dongen JJM, Van Der Velden VHJ, Brüggemann M, Orfao A. Minimal residual disease diagnostics in acute lymphoblastic leukemia: Need for sensitive, fast, and standardized technologies. Blood. 2015;125:3996–4009.
Peters C, Matthes-Martin S, Poetschger U, Schrappe M, Schrauder A, Von Stackelberg A, et al. Stem-cell transplantation in children with acute lymphoblastic leukemia: A prospective international multicenter trial comparing sibling donors with matched unrelated donors - The ALL-SCT-BFM-2003 trial. J Clin Oncol. 2015;33:1265–74.
Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64:83–103.
Chang JH, Poppe MM, Hua C, Marcus KJ, Esiashvili N Acute lymphoblastic leukemia. Pediatr Blood Cancer. 2021;68. Available from: https://doi.org/10.1002/pbc.28371. [Accessed 2023 Oct 16].
Symons HJ, Fuchs EJ. Hematopoietic SCT from partially HLA-mismatched (HLA-haploidentical) related donors. Bone Marrow Transpl. 2008;42:365–77.
Willasch AM, Peters C, Sedláček P, Dalle JH, Kitra-Roussou V, Yesilipek A, et al. Myeloablative conditioning for allo-HSCT in pediatric ALL: FTBI or chemotherapy? A multicenter EBMT-PDWP study. Bone Marrow Transpl. 2020;55:1540–51.
Luznik L, O’Donnell PV, Fuchs EJ. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin Oncol. 2012;39:683–93.
Massei MS, Capolsini I, Mastrodicasa E, Perruccio K, Arcioni F, Cerri C, et al. HLA-haploidentical hematopoietic stem cells transplantation with regulatory and conventional T-cell adoptive immunotherapy in pediatric patients with very high-risk acute leukemia. Bone Marrow Transpl. 2023;58:526–33.
Fuchs EJ. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow Transpl. 2015;50:S31–6.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6.
Im A, Rashidi A, Wang T, Hemmer M, MacMillan ML, Pidala J, et al. Risk Factors for Graft-versus-Host Disease in Haploidentical Hematopoietic Cell Transplantation Using Post-Transplant Cyclophosphamide. Biol Blood Marrow Transpl. 2020;26:1459–68.
Vase JM, Reed EC, Pippert GC, Anderson JR, Bierman PJ, Kessinger A, et al. Mesna Compared With Continuous Bladder Irrigation as Uroprotection During High-Dose Chemotherapy and Transplantation: A Randomized Trial. J Clin Oncol. 1993;11:985–9.
El-Zimaity M, Saliba R, Chan K, Shahjahan M, Carrasco A, Khorshid O, et al. Hemorrhagic cystitis after allogeneic hematopoietic stem cell transplantation: donor type matters. Haematologica. 2004;103:4674–80.
Simione AJ, Das Neves HRA, Da Silva CC, Sabaini PMDS, Geraldo BLSS, Otuyama LJ, et al. Current use and outcomes of hematopoietic stem cell transplantation: Brazilian summary slides - 2023. J Bone Marrow Transplant Cell Ther. 2023;4:200.
Acknowledgements
We are grateful to individuals who participated in the study. This research was supported by Fundo de Incentivo à Pesquisa do Hospital de Clínicas de Porto Alegre (FIPE-HCPA, grant number: 2021–0041).
Author information
Authors and Affiliations
Contributions
DM was responsible for writing, selecting, and reviewing articles, as well as editing the database, interpreting results, and formatting. GL, VARC, RBT, SL, AMR, PRDP, CCK, and POS contributed to the construction of the database. NK played a role in editing the database, reviewing the statistical analysis, interpreting results, and formatting. CR was in charge of submitting the work to the ethics committee. YM was involved in building and editing the database. MBW performed and reviewed the statistical analysis and organized the database. MBM, CB, and LED contributed to the study design, project supervision, and final review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was reviewed and approved by the Local Research Ethics Committee of the Hospital de Clínicas de Porto Alegre and other participating centers (CAAE: 42464621.5.1001.5327, #2021-0035). All methods were performed in accordance with relevant guidelines and regulations. Due to the retrospective nature of this study, the requirement for informed consent was waived by the Ethics Committees of the participating institutions.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morales, D., Loth, G., Colturato, V.A.R. et al. Outcomes of hematopoietic stem cell transplantation in pediatric acute lymphoblastic leukemia: a multicenter Brazilian cohort study. Bone Marrow Transplant 60, 1344–1350 (2025). https://doi.org/10.1038/s41409-025-02676-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02676-1