Abstract
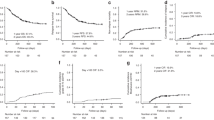
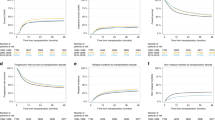
In haploidentical hematopoietic cell transplantation (Haplo-HCT), in vivo or ex vivo T-cell depletion (TCD) can prevent graft-versus-host disease (GVHD) but increase risk of infection and relapse. We hypothesized that TCRαβ-depleted allograft together with upfront infusion with CD45RA-depleted memory T cells (αβTCD + TMDLI) may result in favourable GVHD-free and relapse-free survival (GRFS). Between January 2017 and July 2023, 145 adult patients with various haematological malignancies received αβTCD + TMDLI. All except 2 patients had robust engraftment at a median of 12 days for neutrophil and 11 days for platelet. The cumulative incidence (CI) of CMV, EBV, HHV6 or ADV infection was only 43% (n = 63) at day+120. CI of grade II–IV and III–IV acute GVHD at 180 days was 31% and 8% respectively. Chronic GVHD was seen in only 5 patients with a 2-year CI of 4%. CI of non-relapse mortality and relapse at 2 years were 17% and 22% respectively. At a median follow up of 28 months, 3-year overall (OS), event-free (EFS), and GRFS were 67%, 62%, and 59%, respectively. This was significantly improved over a propensity score-matched contemporary cohort (n = 53) who received PTCy as GVHD prophylaxis. This first multi-center study demonstrated the potential benefits of the αβTCD + TMDLI approach for Haplo-HCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available upon request from the authors at their discretion.
References
Versluis J, Labopin M, Ruggeri A, Socie G, Wu D, Volin L, et al. Alternative donors for allogeneic hematopoietic stem cell transplantation in poor-risk AML in CR1. Blood Adv. 2017;1:477–85.
Hadjis AD, Nunes NS, Khan SM, Fletcher RE, Pohl AdeP, Venzon DJ, et al. Post-transplantation cyclophosphamide uniquely restrains alloreactive CD4+ T-Cell proliferation and differentiation after murine MHC-haploidentical hematopoietic cell transplantation. Front Immunol. 2022;13:796349.
Handgretinger R, Arendt A-M, Maier C-P, Lang P. Ex vivo and in vivo T-cell depletion in allogeneic transplantation: towards less or non-cytotoxic conditioning regimens. Expert Rev Clin Immunol. 2022;18:1285–96.
Champlin RE, Passweg JR, Zhang MJ, Rowlings PA, Pelz CJ, Atkinson KA, et al. T-cell depletion of bone marrow transplants for leukemia from donors other than HLA-identical siblings: advantage of T-cell antibodies with narrow specificities. Blood. 2000;95:3996–4003.
Antin JH, Bierer BE, Smith BR, Ferrara J, Guinan EC, Sieff C, et al. Selective depletion of bone marrow T lymphocytes with anti-CD5 monoclonal antibodies: effective prophylaxis for graft-versus-host disease in patients with hematologic malignancies. Blood. 1991;78:2139–49.
Soiffer RJ, Murray C, Mauch P, Anderson KC, Freedman AS, Rabinowe SN, et al. Prevention of graft-versus-host disease by selective depletion of CD6-positive T lymphocytes from donor bone marrow. J Clin Oncol. 1992;10:1191–200.
Nimer SD, Giorgi J, Gajewski JL, Ku N, Schiller GJ, Lee K, et al. Selective depletion of CD8+ cells for prevention of graft-versus-host disease after bone marrow transplantation. A randomized controlled trial. Transplantation. 1994;57:82–7.
Pulsipher MA, Ahn KW, Bunin NJ, Lalefar N, Anderson E, Flower A, et al. KIR-favorable TCR-αβ/CD19-depleted haploidentical HCT in children with ALL/AML/MDS: primary analysis of the PTCTC ONC1401 trial. Blood. 2022;140:2556–72.
Bethge WA, Eyrich M, Mielke S, Meisel R, Niederwieser D, Schlegel PG, et al. Results of a multicenter phase I/II trial of TCRαβ and CD19-depleted haploidentical hematopoietic stem cell transplantation for adult and pediatric patients. Bone Marrow Transpl. 2022;57:423–30.
Zheng H, Matte-Martone C, Li H, Anderson BE, Venketesan S, Sheng Tan H, et al. Effector memory CD4+ T cells mediate graft-versus-leukemia without inducing graft-versus-host disease. Blood. 2008;111:2476–84.
Chen BJ, Cui X, Sempowski GD, Liu C, Chao NJ. Transfer of allogeneic CD62L– memory T cells without graft-versus-host disease. Blood. 2004;103:1534–41.
Chen BJ, Deoliveira D, Cui X, Le NT, Son J, Whitesides JF, et al. Inability of memory T cells to induce graft-versus-host disease is a result of an abortive alloresponse. Blood. 2007;109:3115–23.
Huang W, Chao NJ. Memory T cells: a helpful guard for allogeneic hematopoietic stem cell transplantation without causing graft-versus-host disease. Hematol Oncol Stem Cell Ther. 2017;10:211–9.
Naik S, Li Y, Talleur AC, Selukar S, Ashcraft E, Cheng C, et al. Memory T-cell enriched haploidentical transplantation with NK cell addback results in promising long-term outcomes: a phase II trial. J Hematol Oncol. 2024;17:50.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424.
Ugozzoli L, Yam P, Petz LD, Ferrara GB, Champlin RE, Forman SJ, et al. Amplification by the polymerase chain reaction of hypervariable regions of the human genome for evaluation of chimerism after bone marrow transplantation. Blood. 1991;77:1607–15.
Van Deerlin VM, Leonard DG. Bone marrow engraftment analysis after allogeneic bone marrow transplantation. Clin Lab Med. 2000;20:197–225.
Tham CS, Linn YC, Koh LP. Desensitisation treatment for HLA-donor specific antibodies in ex-vivo T cell depleted haploidentical allogeneic haematopoietic stem cell transplant – a multi-centre retrospective study in Singapore. Bone Marrow Transpl. 2024;59:140.
Ciurea SO, Al Malki MM, Kongtim P, Zou J, Aung FM, Rondon G, et al. Treatment of allosensitized patients receiving allogeneic transplantation. Blood Adv. 2021;5:4031–43.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295:2097–2100.
Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A, Ballanti S, et al. Full Haplotype-mismatched hematopoietic stem-cell transplantation: a phase II study in patients with acute leukemia at high risk of relapse. J Clin Oncol. 2005;23:3447–54.
Leung W. Use of NK cell activity in cure by transplant. Br J Haematol. 2011;155:14–29.
Koh LP, Poon M, Quek J. Haploidentical haematopoietic cell transplantation of ex vivo TCRab-depleted grafts with CD45RA-depleted memory T cell add-back reduces chronic graft-versus-host disease and results in favourable GvHD-Relapse free survival: 5-year follow-up of 107 patients treated in a multicenter study in Singapore. Blood. 2022;140:4707–8.
Bleakley M, Sehgal A, Seropian S, Biernacki MA, Krakow EF, Dahlberg A, et al. Naive T-cell depletion to prevent chronic graft-versus-host disease. J Clin Oncol. 2022;40:1174–85.
Maeda Y, Reddy P, Lowler KP, Liu C, Bishop DK, Ferrara JLM. Critical role of host gammadelta T cells in experimental acute graft-versus-host disease. Blood. 2005;106:749–55.
Cantoni N, Hirsch HH, Khanna N, Gerull S, Buser A, Bucher C, et al. Evidence for a bidirectional relationship between cytomegalovirus replication and acute graft-versus-host disease. Biol Blood Marrow Transpl. 2010;16:1309–14.
Legoff J, Resche-Rigon M, Bouquet J, Robin M, Naccache SN, Mercier-Delarue S, et al. The eukaryotic gut virome in hematopoietic stem cell transplantation: new clues in enteric graft-versus-host disease. Nat Med. 2017;23:1080–5.
Triplett BM, Shook DR, Eldridge P, Li Y, Kang G, Dallas M, et al. Rapid memory T-cell reconstitution recapitulating CD45RA-depleted haploidentical transplant graft content in patients with hematologic malignancies. Bone Marrow Transpl. 2015;50:968–77.
Castagna L, Valli V, Timofeeva I, Capizzuto R, Bramanti S, Mariotti J, et al. Feasibility and efficacy of CD45RA+ depleted donor lymphocytes infusion after haploidentical transplantation with post-transplantation cyclophosphamide in patients with hematological malignancies. Transplant Cell Ther. 2021;27:478.e1–478.e5.
Bashey A, Zhang M-J, McCurdy SR, St. Martin A, Argall T, Anasetti C, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-Cell–replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2017;35:3002–9.
Fuchs EJ, O’Donnell PV, Eapen M, Logan B, Antin JH, Dawson P, et al. Double unrelated umbilical cord blood vs HLA-haploidentical bone marrow transplantation: the BMT CTN 1101 trial. Blood. 2021;137:420–8.
Mehta RS, Saliba RM, Ghanem S, Alousi AM, Rondon G, Anderlini P, et al. Haploidentical versus matched unrelated versus matched sibling donor hematopoietic cell transplantation with post-transplantation cyclophosphamide. Transplant Cell Ther. 2022;28:395.e1–11.
Ruggeri A, Labopin M, Bacigalupo A, Gülbas Z, Koc Y, Blaise D, et al. Bone marrow versus mobilized peripheral blood stem cells in haploidentical transplants using posttransplantation cyclophosphamide. Cancer. 2018;124:1428–37.
Granata A, Fürst S, Bramanti S, Legrand F, Sarina B, Harbi S, et al. Peripheral blood stem cell for haploidentical transplantation with post-transplant high dose cyclophosphamide: detailed analysis of 181 consecutive patients. Bone Marrow Transpl. 2019;54:1730–7.
Mariotti J, Devillier R, Bramanti S, Giordano L, Sarina B, Furst S, et al. Peripheral blood stem cells versus bone marrow for T cell–replete haploidentical transplantation with post-transplant cyclophosphamide in Hodgkin Lymphoma. Biol Blood Marrow Transpl. 2019;25:1810–7.
Gooptu M, Romee R, St. Martin A, Arora M, Al Malki M, Antin JH, et al. HLA-haploidentical vs matched unrelated donor transplants with posttransplant cyclophosphamide-based prophylaxis. Blood. 2021;138:273–82.
McCurdy SR, Kanakry JA, Showel MM, Tsai H-L, Bolaños-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125:3024–31.
Esquirol A, Pascual MJ, kwon M, Pérez A, Parody R, Ferra C, et al. Severe infections and infection-related mortality in a large series of haploidentical hematopoietic stem cell transplantation with post-transplant cyclophosphamide. Bone Marrow Transpl. 2021;56:2432–44.
Goldsmith SR, Slade M, DiPersio JF, Westervelt P, Lawrence SJ, Uy GL, et al. Cytomegalovirus viremia, disease, and impact on relapse in T-cell replete peripheral blood haploidentical hematopoietic cell transplantation with post-transplant cyclophosphamide. Haematologica. 2016;101:e465–8.
Ramlal R, Sasaki K, Cerrada SL, Srour SA, Chen J, Rondon RG, et al. Viral reactivation in haploidentical transplants using post-transplantation cyclophosphamide – a single institution experience. Biol Blood Marrow Transpl. 2016;22:S375–6.
Goldsmith SR, Abid MB, Auletta JJ, Bashey A, Beitinjaneh A, Castillo P, et al. Posttransplant cyclophosphamide is associated with increased cytomegalovirus infection: a CIBMTR analysis. Blood. 2021;137:3291–305.
Triplett BM, Muller B, Kang G, Li Y, Cross SJ, Moen J, et al. Selective T-cell depletion targeting CD45RA reduces viremia and enhances early T-cell recovery compared with CD3-targeted T-cell depletion. Transpl. Infect. Dis. 2018; 20, https://doi.org/10.1111/tid.12823.
Gasior Kabat M, Li Y, Galán V, Mozo Y, Sisinni L, Bueno-Sánchez D, et al. Safety and efficacy of high-dose memory CD45RO+ donor lymphocyte infusion in pediatric recipients after hematopoietic stem cell transplantation. Cytotherapy. 2024;26:1458–64.
van Beek JJP, Puccio S, Di Vito C, De Paoli F, Zaghi E, Calvi M, et al. Selected memory T cells infused post-haploidentical hematopoietic stem cell transplantation persist and hyperexpand. Blood Adv. 2023;7:3458–68.
Merli P, Algeri M, Galaverna F, Bertaina V, Lucarelli B, Boccieri E, et al. TCRαβ/CD19 cell–depleted HLA-haploidentical transplantation to treat pediatric acute leukemia: updated final analysis. Blood. 2024;143:279–89.
Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biology Blood Marrow Transpl. 2014;20:1573–9.
Sanz J, Boluda JCH, Martín C, González M, Ferrá C, Serrano D, et al. Single-unit umbilical cord blood transplantation from unrelated donors in patients with hematological malignancy using busulfan, thiotepa, fludarabine and ATG as myeloablative conditioning regimen. Bone Marrow Transpl. 2012;47:1287–93.
Rezvani K, Grube M, Brenchley JM, Sconocchia G, Fujiwara H, Price DA, et al. Functional leukemia-associated antigen-specific memory CD8+ T cells exist in healthy individuals and in patients with chronic myelogenous leukemia before and after stem cell transplantation. Blood. 2003;102:2892–900.
Maziarz RT, Devine S, Garrison LP, Agodoa I, Badaracco J, Gitlin M, et al. Estimating the lifetime medical cost burden of an allogeneic hematopoietic cell transplantation patient. Transpl Cell Ther. 2023;29:637.e1–637.e9.
Leen AM, Christin A, Myers GD, Liu H, Cruz CR, Hanley PJ, et al. Cytotoxic T lymphocyte therapy with donor T cells prevents and treats adenovirus and Epstein-Barr virus infections after haploidentical and matched unrelated stem cell transplantation. Blood. 2009;114:4283–92.
Kinoshita H, Cooke KR, Grant M, Stanojevic M, Cruz CR, Keller M, et al. Outcome of donor-derived TAA-T cell therapy in patients with high-risk or relapsed acute leukemia post allogeneic BMT. Blood Adv. 2022;6:2520–34.
Craddock C, Friedberg JW. Immunotherapy for hematologic malignancies. J Clin Oncol. 2021;39:343–5.
Acknowledgements
The authors acknowledge the continuous effort of the entire team involved in our transplant program, including junior medical staff, other medical disciplines, transplant coordinators, nurses, laboratory colleagues, pharmacists, and social workers for the excellent support rendered to our patients. Most importantly, we are grateful to all our patients and their families for their courage, trust, and cooperation.
Author information
Authors and Affiliations
Contributions
LPK, YCL, and WL conceived and designed the study; LPK, YCL, YBL, VL, ZYL, MP, JQ, HT, CPD, BV, AH, FL, WH, LKT, JRMC, JL, IW, KWY, BH, WSL, LN, TTT, YL, TGS, GG, and KKH provided study material or patients; LPK, YCL, YJK, and WL collected and assembled the data; LPK, YCL, and WL analyzed and interpreted the data; LPK, YCL, and WL wrote the manuscript; and all authors provided final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the National University Hospital (NHG DSRB 2010/00431) and Singapore General Hospital (Singhealth CRIB 2015-2419). All methods were conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koh, LP., Linn, Y.C., Boo, Y.L. et al. Upfront memory T cell add-back with haploidentical TCRαβ-depleted graft in adults with haematological malignancies: a nationwide, multicentre, single-arm, prospective study. Bone Marrow Transplant 61, 26–35 (2026). https://doi.org/10.1038/s41409-025-02728-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02728-6