Abstract
Introduction Minimally invasive dentistry has been promoted as the contemporary approach to the operative management of dental caries. Operative intervention should be undertaken on cavitated lesions which are actively progressing. However, there may be large variability in the restorative intervention thresholds and care plans of general dental practitioners (GDPs).
Aims To investigate restorative threshold and treatment decisions for occlusal and proximal carious lesions in a cohort of GDPs in London. To investigate potential differences based on number of years since graduation and attendance on a caries management course.
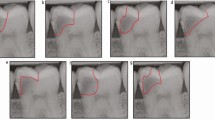
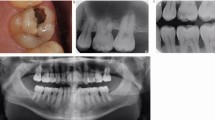
Materials and methods A previously used, validated caries questionnaire was distributed to foundation dentists, general practice dentists and practising educational supervisors in NHS London dental practices.
Results Two hundred and seventeen GDPs participated in the study. For occlusal lesions, nine (9.1%) newly-qualified dentists selected to intervene surgically on lesions confined to enamel, compared to 24 (29.8%) dentists who have been qualified for more than five years (p <0.05). In addition, a greater number of dentists who had attended a training course were more likely to do a minimally invasive preparation for a proximal lesion (38.2%), compared to 19.8% of those who had not (p <0.05). The majority of all participants (74.2%) chose to restore a proximal lesion using resin composite. Despite this material choice, 58.5% of those graduating within five years opted to prepare a traditional Black's class II cavity.
Conclusion A practitioner's restorative intervention threshold and their choice of treatment appears to be negatively affected by the number of years post-qualification, and positively influenced by attending a caries management course.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Banerjee A. 'MI'opia or 20/20 vision? Br Dent J 2013; 214: 101-105. DOI: 10.1038/sj.bdj.2013.105.
Domejean S, Banerjee A, Featherstone J D B. Caries risk/ susceptibility assessment: its value in minimum intervention oral health care. Br Dent J 2017; 223: 191-197. DOI: 10.1038/sj.bdj.2017.665.
Banerjee A. Minimal intervention dentistry: part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J 2013; 214: 107-111. DOI: 10.1038/sj.bdj.2013.106.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing carious lesions: Consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58-67. DOI: 10.1177/0022034516639271.
Banerjee A. 'Minimum intervention' - MI inspiring future oral healthcare? Br Dent J 2017; 223: 133-135. DOI: 10.1038/sj.bdj.2017.644.
Banerjee A, Frencken J E, Schwendicke F, Innes N P T. Contemporary operative caries management: consensus recommendations on minimal caries removal. Br Dent J 2017; 223: 215-222. DOI: 10/1038/sj.bdj.2017.672.
Banerjee A. Selective removal of carious dentine. In Scwendicke F, ed. Management of deep carious lesions. Switzerland: Springer International Publishing AG; 2018. pp. 55-70. DOI: 10/1007/9783319613703_5.
Black G. A work on operative dentistry: The technical procedures in filling teeth. Chicago: MedicoDental Publishing Company; 1908.
Domejean-Orliaguet S, Banerjee A, Gaucher C, Miletic I, Basson M RE. Minimum intervention treatment plan: a practical implementation in general dental practice. J Minim Interv Den. 2009; 2: 103-123.
Banerjee A, Domejean S. The contemporary approach to tooth preservation: minimum intervention caries management in general practice. Prim Dent J 2013; 2: 30-37.
Bader J D, Shugars D A. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol 1997; 25: 97-103.
Kay E J, Locker D. Variations in restorative treatment decisions: an international comparison. Community Dent Oral Epidemiol 1996; 24: 376-379. DOI: 10.1111/j.1600-0528.1996.tb00882.x.
Espelid I, Tveit A B, Mejàre I, Sundberg H, Hallonsten A L. Restorative treatment decisions on occlusal caries in Scandinavia. Acta Odontol Scand 2001; 59: 21-27. DOI: 10.1080/000163501300035724.
Tveit A B, Espelid I, Skodje F. Restorative treatment decisions on approximal caries in Norway. Int Dent J 1999; 49: 165-172. DOI: 10.1002/j.1875-1595X.1999.tb00902.x.
Domejean-Orilaguet S, Tubert-Jeannin S, Riordan P J, Espelid I, Tveit A. French dentists' restorative treatment decisions. Oral Health Prev Dent 2004; 2: 125-131.
Rechmann P, Doméjean S, Rechmann B M T, Kinsel R, Featherstone J D B. Approximal and occlusal carious lesions. Restorative treatment decisions by California dentists. J Am Dent Assoc 2016; 147: 328-338. DOI: 10.1016/j.adaj.2015.10.006.
Khalaf M E, Alomari Q D, Ngo H, Doméjean S. Restorative treatment thresholds: Factors influencing the treatment thresholds and modalities of general dentists in Kuwait. Med Princ Pract 2014; 23: 357-362. DOI: 10.1159/000363184.
Domejean S, Leger S, Maltrait M, Espelid E, Tveit A B, Tubert-Jeannin S. Changes in Occlusal Caries Lesion Management in France from 2002 to 2012: A Persistent Gap between Evidence and Clinical Practice. Caries Res 2015; 49: 408-416.
Curtis B, Warren E, Pollicino C, Evans R W, Schwarz E, Sbarini A. The Monitor Practice Programme: is non-invasive management of dental caries in private practice cost-effective? Aust Dent J 2011; 56: 48-55. DOI: 10.1111/]j.1834-7819.2010.01286.x.
Schwendicke F, Paris S, Stolpe M. Cost-effectiveness of caries excavations in different risk groups - a micro-simulation study. BMC Oral Health 2014; 14: 153.
Mount G J. Minimal intervention dentistry: cavity classification & preparation. J Minimal Interv Dent 2009; 2: 150-162.
Innes N, Schwendicke F, Frencken J. An agreed terminology for carious tissue removal. Monogr Oral Sci 2018; 27: 155-161. DOI: 10.1159/000487842.
United Nations. What is the Minamata Convention on mercury?. 2018. Available online at http://ask.un.org/faq/192079 (accessed 13 March 2019).
Kay E J, Nuttall N M. Relationship between dentists'treatment attitudes and restorative decisions made on the basis of simulated bitewing radiographs. Community Dent Oral Epidemiol 1994; 22: 71-74. DOI: 10.1111/j.1600-0528.1994.tb01575.x.
Acknowledgements
The authors thank Dr Sophie Domejean for providing the questionnaire used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chana, P., Orlans, M., O’Toole, S. et al. Restorative intervention thresholds and treatment decisions of general dental practitioners in London. Br Dent J 227, 727–732 (2019). https://doi.org/10.1038/s41415-019-0849-7
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41415-019-0849-7
This article is cited by
-
The long-term oral health consequences of an amalgam phase-out
British Dental Journal (2025)
-
Minimum intervention oral care: staging and grading dental carious lesions in clinical practice
British Dental Journal (2024)
-
Bridging the gap: harnessing clinical evidence for smarter primary care dentistry
British Dental Journal (2024)
-
General dental practice and improved oral health: is there a win-win for both the professional establishment and government?
British Dental Journal (2020)
-
Minimum intervention oral healthcare delivery - is there consensus?
British Dental Journal (2020)