Abstract
Introduction Dentists prescribe a significant proportion of all antibiotics, while antimicrobial stewardship aims to minimise antibiotic-prescribing to reduce the risk of developing antibiotic-resistance and adverse drug reactions.
Aims To evaluate NHS antibiotic-prescribing practices of dentists in England between 2010-2017.
Methods NHS Digital 2010-2017 data for England were analysed to quantify dental and general primary-care oral antibiotic prescribing.
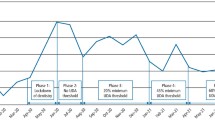
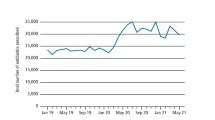
Results Dental prescribing accounted for 10.8% of all oral antibiotic prescribing, 18.4% of amoxicillin and 57.0% of metronidazole prescribing in primary care. Amoxicillin accounted for 64.8% of all oral antibiotic prescribing by dentists, followed by metronidazole (28.0%), erythromycin (4.4%), phenoxymethylpenicillin (0.9%), clindamycin (0.6%), co-amoxiclav (0.5%), cephalosporins (0.4%) and tetracyclines (0.3%). Prescriptions by dentists declined during the study period for all antibiotics except for co-amoxiclav. This increase is of concern given the need to restrict co-amoxiclav use to infections where there is no alternative. Dental prescribing of clindamycin, which accounted for 43.9% of primary care prescribing in 2010, accounted for only 14.6% in 2017. Overall oral antibiotic prescribing by dentists fell 24.4% as compared to 14.8% in all of primary care.
Conclusions These data suggest dentists have reduced antibiotic prescribing, possibly more than in other areas of primary-care. Nonetheless, opportunities remain for further reduction.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
National Institute for Health and Care Excellence (NICE). Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use 2015. Nice Guideline 15 [NG]. Available online at https://www.nice.org.uk/guidance/NG15/chapter/1-Recommendations#recommendationsforprescribers (accessed 12 November 2019).
Baddour L M, Dayer M J, Thornhill M H. Fluoroquinolone use and associated adverse drug events in England. J Infect 2019; 78: 249-259.
Longman L P, Martin M V. The use of antibiotics in the prevention of post-operative infection: a re-appraisal. Br Dent J 1991; 170: 257-262.
Martin M V, Longman L P, Hill J B, Hardy P. Acute dentoalveolar infections: an investigation of the duration of antibiotic therapy. Br Dent J 1997; 183: 135-137.
Public Health England. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR). London: Public Health England, 2018.
Teoh L, Stewart K, Marino R J, McCullough M J. Part 1. Current prescribing trends of antibiotics by dentists in Australia from 2013 to 2016. Aust Dent J 2018; DOI: 10.1111/adj.12622.
Marra F, George D, Chong M, Sutherland S, Patrick D M. Antibiotic prescribing by dentists has increased: Why? J Am Dent Assoc 2016; 147: 320-327.
Durkin M J, Hsueh K, Sallah Y H et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc 2017; 148: 878-886.
Dayer M J, Jones S, Prendergast B, Baddour L M, Lockhart P B, Thornhill M H. Incidence of infective endocarditis in England, 2000-2013: a secular trend, interrupted time-series analysis. Lancet 2015; 385: 1219-1228.
Thornhill M H, Dayer M J, Forde J M et al. Impact of the NICE guideline recommending cessation of antibiotic prophylaxis for prevention of infective endocarditis: before and after study. BMJ 2011; 342: d2392.
SDCEP. Antibiotic prophylaxis against infective endocarditis 2018. (Updated 23rd August 2018.) Available online at http://www.sdcep.org.uk/published-guidance/antibiotic-prophylaxis/ (accessed 12 November 2019).
Baddour L M, Dayer M J, Thornhill M H. Adverse drug reactions due to oral antibiotics in the community setting - England. Infectious Diseases 2019; 51: 866-869.
Thornhill M H, Dayer M J, Durkin M J, Lockhart P B, Baddour L M. Risk of adverse reactions to oral antibiotics prescribed by dentists. J Dent Res 2019; 98: 1081-1087.
Bartlett J G, Chang T W, Gurwith M, Gorbach S L, Onderdonk A B. Antibiotic-associated pseudomembranous colitis due to toxin-producing clostridia. N Engl J Med 1978; 298: 531-534.
Lusk R H, Fekety F R Jr., Silva J Jr. et al. Gastrointestinal side effects of clindamycin and ampicillin therapy. The Journal of infectious diseases. 1977; 135 Suppl: S111-119.
Thornhill M H, Dayer M J, Prendergast B, Baddour L M, Jones S, Lockhart P B. Incidence and nature of adverse reactions to antibiotics used as endocarditis prophylaxis. J Antimicrob Chemother 2015; 70: 2382-2388.
Brown K A, Khanafer N, Daneman N, Fisman D N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother 2013; 57: 2326-2332.
Beacher N, Sweeney M P, Bagg J. Dentists, antibiotics and Clostridium difficile-associated disease. Br Dent J 2015; 219: 275-279.
Eick S, Pfister W, Straube E. Antimicrobial susceptibility of anaerobic and capnophilic bacteria isolated from odontogenic abscesses and rapidly progressive periodontitis. Int J Antimicrob Agents 1999; 12: 41-46.
Handal T, Olsen I. Antimicrobial resistance with focus on oral beta-lactamases. Eur J Oral Sci 2000; 108: 163-174.
Handal T, Olsen I, Walker C B, Caugant D A. Beta-lactamase production and antimicrobial susceptibility of subgingival bacteria from refractory periodontitis. Oral Microbiol Immunol 2004; 19: 303-308.
Baumgartner J C, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. J Endod 2003; 29: 44-47.
Lewis M A, Carmichael F, MacFarlane T W, Milligan S G. A randomised trial of co-amoxiclav (Augmentin) versus penicillin V in the treatment of acute dentoalveolar abscess. Br Dent J 1993; 175: 169-174.
Ellison S J. The role of phenoxymethylpenicillin, amoxicillin, metronidazole and clindamycin in the management of acute dentoalveolar abscessesa review. Br Dent J 2009; 206: 357-362.
Lewis M A, MacFarlane T W, McGowan D A. Quantitative bacteriology of acute dento-alveolar abscesses. J Med Microbiol 1986; 21: 101-104.
Lewis M A, MacFarlane T W, McGowan D A. A microbiological and clinical review of the acute dentoalveolar abscess. Br J Oral Maxillofac Surg 1990; 28: 359-366.
Stefanopoulos P K, Kolokotronis A E. The clinical significance of anaerobic bacteria in acute orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98: 398-408.
Lewis M A, MacFarlane T W, McGowan D A, MacDonald D G. Assessment of the pathogenicity of bacterial species isolated from acute dentoalveolar abscesses. J Med Microbiol 1988; 27: 109-116.
Hood F J. The place of metronidazole in the treatment of acute oro-facial infection. J Antimicrob Chemother 1978; 4 Suppl C: 71-73.
Kuriyama T, Williams D W, Yanagisawa M et al. Antimicrobial susceptibility of 800 anaerobic isolates from patients with dentoalveolar infection to 13 oral antibiotics. Oral Microbiol Immunol 2007; 22: 285-288.
Lewis M A, MacFarlane T W, McGowan D A. Antibiotic susceptibilities of bacteria isolated from acute dentoalveolar abscesses. J Antimicrob Chemother 1989; 23: 69-77.
Sandor G K, Low D E, Judd P L, Davidson R J. Antimicrobial treatment options in the management of odontogenic infections. J Can Dent Assoc 1998; 64: 508-514.
Barker G R, Qualtrough A J. An investigation into antibiotic prescribing at a dental teaching hospital. Br Dent J 1987; 162: 303-306.
Olson A K, Edington E M, Kulid J C, Weller R N. Update on antibiotics for the endodontic practice. Compendium 1990; 11: 328-332.
Palmer N O, Martin M V, Pealing R, Ireland R S. An analysis of antibiotic prescriptions from general dental practitioners in England. J Antimicrob Chemother 2000; 46: 1033-1035.
Al-Haroni M, Skaug N. Incidence of antibiotic prescribing in dental practice in Norway and its contribution to national consumption. J Antimicrob Chemother 2007; 59: 1161-1166.
Fadare J O, Oshikoya K A, Obimakinde O S et al. Patterns of drugs prescribed for dental outpatients in Nigeria: findings and implications. Acta Odontol Scand 2017; 75: 496-506.
Dar-Odeh N S, Abu-Hammad O A, Khraisat A S, El Maaytah M A, Shehabi A. An analysis of therapeutic, adult antibiotic prescriptions issued by dental practitioners in Jordan. Chemotherapy 2008; 54: 17-22.
Konde S, Jairam L S, Peethambar P, Noojady S R, Kumar N C. Antibiotic overusage and resistance: A cross-sectional survey among paediatric dentists. J Indian Soc Paedod Prev Dent 2016; 34: 145-151.
Tanwir F, Marrone G, Tariq A, Lundborg C S. Diagnosis and prescribing pattern of antibiotics and painkillers among dentists. Oral Health Prev Dent 2015; 13: 75-83.
Ford P J, Saladine C, Zhang K, Hollingworth S A. Prescribing patterns of dental practitioners in Australia from 2001 to 2012. Antimicrobials. Aust Dent J 2017; 62: 52-57.
Schentag J J, Ballow C H. Tissue-directed pharmacokinetics. Am J Med 1991; 91: 5S-11S.
Williams J D, Sefton A M. Comparison of macrolide antibiotics. J Antimicrob Chemother 1993; 31 Suppl C: 11-26.
Malizia T, Tejada M R, Ghelardi E et al. Periodontal tissue disposition of azithromycin. J Periodontol 1997; 68: 1206-1209.
Cope A L, Francis N A, Wood F, Chestnutt I G. Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dent Oral Epidemiol 2016; 44: 145-153.
British Medical Association & Royal Pharmaceutical Society. BNF - The British National Formulary: BMJ Group and Pharmaceutical Press, 2019.
Scottish Dental Clinical Effectiveness Programme. Drug Prescribing for Dentistry 2016. Available online at http://www.sdcep.org.uk/published-guidance/drug-prescribing/ (accessed 12 November 2019).
Faculty of General Dental Practice. Antimicrobial prescribing for GDPs. London: Royal College of Surgeons of England Faculty of General Dental Practice, 2016.
Cope A L, Chestnutt I G. Inappropriate prescribing of antibiotics in primary dental care: reasons and resolutions. Prim Dent J 2014; 3: 33-37.
Cope A L, Wood F, Francis N A, Chestnutt I G. General dental practitioners' perceptions of antimicrobial use and resistance: a qualitative interview study. Br Dent J 2014; 217: E9.
Thompson W, Tonkin-Crine S, Pavitt S H et al. Factors associated with antibiotic prescribing for adults with acute conditions: an umbrella review across primary care and a systematic review focusing on primary dental care. J Antimicrob Chemother 2019; 74: 2139-2152.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thornhill, M., Dayer, M., Durkin, M. et al. Oral antibiotic prescribing by NHS dentists in England 2010-2017. Br Dent J 227, 1044–1050 (2019). https://doi.org/10.1038/s41415-019-1002-3
Published:
Issue date:
DOI: https://doi.org/10.1038/s41415-019-1002-3
This article is cited by
-
The butterfly effect: collateral damage and impacts of antimicrobial strategies on the oral microbiome
npj Antimicrobials and Resistance (2025)
-
From prescription to protection: combating antimicrobial resistance in dental practice
Evidence-Based Dentistry (2024)
-
AAA: a rock and a hard place
British Dental Journal (2021)
-
Can antibiotic prescribing recover its downward trajectory during 2021?
BDJ In Practice (2021)
-
Biofilm viability checker: An open-source tool for automated biofilm viability analysis from confocal microscopy images
npj Biofilms and Microbiomes (2021)