Abstract
Background Multiple determinants influence dentists' health and wellbeing. In light of recent concerns, the aim of this research was to explore contemporary influences on dentists' health and wellbeing in England, drawing on their lived experience.
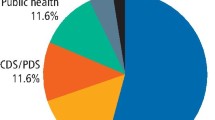
Methods Semi-structured interviews were conducted with a purposive sample of dentists working in England, taking into account age, gender, career stage, work sector, geographical area, position and route of entry to registration. A topic guide, informed by the literature, was used to guide the discourse. Dentists were approached via gatekeepers, supported by snowball sampling. Interviews were recorded and transcribed for analysis. Framework analysis was used, taking an interpretative phenomenological approach to develop theory.
Results Twenty dentists, from a range of backgrounds, participated in this research. While health and wellbeing was reported to be more positive among dentists in their later career, those in their early career and/or with high NHS work commitments shared concerns about their physical, psychological and emotional health. Influences ranged from macro-level issues relating to professional regulation and health systems, through meso-level, notably their workplace and job specification, to micro-level issues relating to their professional careers, relationships and personal life. Dentists highlighted ethical concerns and feeling driven to deliver, together with being demoralised by a survival culture, all leading to perceived lack of control and reduced professional fulfilment. In contrast, being able to deliver quality care, innovate and effect change, as well as being valued for their delivery, were perceived to positively contribute to general health and wellbeing.
Conclusion Dentists have a vital role in providing care for patients, so there are serious public health implications if urgent action is not taken to improve and sustain their health and wellbeing. This study confirms that dentists are affected by multiple contemporary influences, and although greater support is needed for individuals, organisational, system and policy changes may be required to fully address the challenges they face.
Key points
-
Highlights the wide range of contemporary influences on dentists' health and wellbeing, from macro- through meso- to micro-level.
-
Raises concerns that dentists, particularly those with high NHS primary care work commitments, are perceiving lack of control in their professional lives.
-
Dentists who were able to use their expertise to the full, in roles where they were able to deliver quality care and felt valued for their delivery, expressed greater confidence in their health and wellbeing.
-
Discusses the implications of retaining the dental workforce in light of the COVID-19 pandemic and its impact on our profession.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Colonio-Salazar F B, Sipiyaruk K, White S, Gallagher J E. Key determinants of health and wellbeing of dentists within the UK: a rapid review of over two decades of research. Br Dent J 2019; 227: 127-136.
Hancocks S. Well, being a dentist. Br Dent J 2019; 227: 69.
O'Selmo E, Collin V, Whitehead P. Dental associates' perceptions of their working environment: a qualitative study. Br Dent J 2019; 226: 955-962.
Collin V, Toon M, O'Selmo E, Reynolds L, Whitehead P. A survey of stress, burnout and well-being in UK dentists. Br Dent J 2019; 226: 40-49.
Toon M, Collin V, Whitehead P, Reynolds L. An analysis of stress and burnout in UK general dental practitioners: subdimensions and causes. Br Dent J 2019; 226: 125-130.
NHS Digital. Dental Working Hours: 2014/15 and 2015/16 Motivation Analysis, Experimental Statistics. London: NHS Digital, 2016.
NHS Digital. Dental Working Hours: 2016/17 and 2017/18 Working Patterns, Motivation and Morale [PAS]. London: NHS Digital, 2018.
NHS Digital. Dentists' Working Patterns, Motivation and Morale - 2018/19 and 2019/20. London: NHS Digital, 2020.
British Dental Association. The Psychosocial Working Conditions and Work-related stress among Community Dentists in the UK: Results from the 2014 Dentists' Wellbeing and Working Conditions surveys. London: BDA, 2015.
Larbie J, Kemp M, Whitehead P. The Mental Health and Well-being of UK Dentists: being of UK Dentists: A Qualitative Study. London: BDA, 2017.
NHS Digital. Dental Working Hours - Working Patterns, Motivation and Morale 2016/2017 and 2017/2018. London: NHS Digital, 2018.
British Dental Association. Half of NHS young dentists heading for the exit. 2017. Available online at https://bda.org/news-centre/press-releases/half-of-nhsyoung-dentists-heading-for-the-exit (accessed October 2020).
British Dental Association. 75% of NHS dental practices now struggling to fill vacancies. 2019. Available online at https://bda.org/news-centre/press-releases/Pages/75-per-cent-of-NHS-dental-practices-now-struggling-to-fill-vacancies.aspx (accessed October 2020).
British Dental Association. Is Government serious about the survival of NHS dentistry? 2019. Available at https://bda.org/news-centre/blog/is-government-serious-about-the-survival-of-nhs-dentistry (accessed May 2021).
Surman G, Goldacre M J, Lambert T W. UK-trained junior doctors' intentions to work in UK medicine: questionnaire surveys, three years after graduation. J R Soc Med 2017; 110: 493-500.
Moberly T. Health and wellbeing is the most common reason for doctors to take a break from training. BMJ 2018; DOI: 10.1136/bmj.k3097.
British Dental Association. Student Manifesto 2018-2020. 2018. Available at https://bda.org/news-centre/blog/Documents/BDA-Student-Manifesto-2018.pdf (accessed May 2021).
Watt R G, Steele J G, Treasure E T, White D A, Pitts N B, Murray J J. Adult Dental Health Survey 2009: implications of findings for clinical practice and oral health policy. Br Dent J 2013; 214: 71-75.
White D A, Tsakos G, Pitts N B et al. Adult Dental Health Survey 2009: common oral health conditions and their impact on the population. Br Dent J 2012; 213: 567-572.
The Health and Social Care Information Centre. Adult Dental Health Survey 2009 - Summary report and thematic series [NS]. London: HSCIC, 2011.
Steele J. Review of NHS Dental Services in England: an independent review. London: Department of Health, 2009.
General Dental Council. Registration report - March 2019. London: GDC, 2019.
Health Education England. Advancing Dental Care (ADC) Education & Training Review. 2018. Available online at https://www.hee.nhs.uk/our-work/advancing-dental-care (accessed October 2020).
Palinkas L A, Horwitz S M, Green C A, Wisdom J P, Duan N, Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health 2015; 42: 533-544.
Ritchie J, Lewis J, Nicholls C M, Ormston R. Qualitative research practice: A guide for social science students and researchers. London: Sage, 2013.
NHS Digital. NHS Dental Statistics England 2015/16. London: NHS Digital, 2016.
Kemp M, Edwards H. The Financial Circumstances of Final Year Dental Undergraduates in the UK. London: BDA, 2014.
D'Amour D, Oandasan I. Interprofessionality as the field of interprofessional practice and interprofessional education: An emerging concept. J Interprof Care 2005; 19 Suppl 1: 8-20.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health C 2007; 19: 349-357.
Flowers P, Larkin M, Smith J. Interpretative phenomenological analysis: Theory, method and research. London: Sage Publications Ltd, 2009.
Gilmour J, Stewardson D A. Morale of vocational dental practitioners in the United Kingdom. Br Dent J 2008; 204: E18.
Bretherton R, Chapman H R, Chipchase S. A study to explore specific stressors and coping strategies in primary dental care practice. Br Dent J 2016; 220: 471-478.
Humphris G M, Cooper C L. New stressors for GDPs in the past ten years: a qualitative study. Br Dent J 1998; 185: 404-406.
O'Selmo E, Collin V, Whitehead P. Dental associates' perceptions of their working environment: a qualitative study. Br Dent J 2019; 226: 955-962.
Myers H, Myers L. 'It's difficult being a dentist': Stress and health in the general dental practitioner. Br Dent J 2004; 197: 89-93; discussion 83; quiz 100.
Chapman H R, Chipchase S Y, Bretherton R. Understanding emotionally relevant situations in primary dental practice. 3. Emerging narratives. Br Dent J 2015; 219: 491-496.
Hill K B, Burke F J T, Brown J et al. Dental practitioners and ill health retirement: a qualitative investigation into the causes and effects. Br Dent J 2010; 209: E8.
Newton J T, Gibbons D E. Levels of career satisfaction among dental healthcare professionals: comparison of dental therapists, dental hygienists and dental practitioners. Community Dent Health 2001; 18: 172-176.
Gorter R C, Freeman R. Burnout and engagement in relation with job demands and resources among dental staff in Northern Ireland. Community Dent Oral Epidemiol 2011; 39: 87-95.
Gilmour J, Stewardson D A, Shugars D A, Burke F J T. An assessment of career satisfaction among a group of general dental practitioners in Staffordshire. Br Dent J 2005; 198: 701-704.
Kay E J, Lowe J C. A survey of stress levels, self-perceived health and health-related behaviours of UK dental practitioners in 2005. Br Dent J 2008; 204: E19.
Jones L M, Cotter R, Birch K M. A review of occupationally-linked suicide for dentists. N Z Dent J 2016; 112: 39-46.
Rogers C, Malone K M. Stress in Irish dentists: developing effective coping strategies. J Ir Dent Assoc 2009; 55: 304-307.
Gorter R C, Albrecht G, Hoogstraten J, Eijkman M A. Professional burnout among Dutch dentists. Community Dent Oral Epidemiol 1999; 27: 109-116.
Ab-Murat N, Mason L, Kadir R A, Yusoff N. Self-perceived mental well-being among Malaysian dentists. Int J Occup Saf Ergon 2018; 24: 233-239.
Meyerson J, Gelkopf M, Eli I, Uziel N. Burnout and professional quality of life among Israeli dentists: the role of sensory processing sensitivity. Int Dent J 2020; 70: 29-37.
Clough B A, Ireland M J, Leane S, March S. Stressors and protective factors among regional and metropolitan Australian medical doctors: A mixed methods investigation. J Clin Psychol 2020; 76: 1362-1389.
Robertson H D, Elliott A M, Burton C et al. Resilience of primary healthcare professionals: a systematic review. Br J Gen Pract 2016; DOI: 10.3399/bjgp16X685261.
Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T. H. Chan School of Public Health and Harvard Global Health Institute. A Crisis in Health Care: a call to action on Physician Burnout. Boston: Harvard Global Health Institute, 2019.
Rimmer A. Covid-19: Doctors may quit without proper post-pandemic support, defence body warns. BMJ 2020; DOI: 10.1136/bmj.m2476.
National Academy of Medicine. Action Collaborative on Clinician Well-Being and Resilience. 2017. Available online at https://nam.edu/initiatives/clinician-resilience-and-well-being/ (accessed May 2021).
Brigham T, Barden C, Dopp A L et al. Factors Affecting Clinician Well-Being and Resilience - Conceptual Model. Washinton DC: National Academy of Medicine, 2018.
Oldfield E. Plymouth's NHS dentists crisis - experts demand action. Plymouth Herald (Plymouth) 2020 January 14.
Gallagher J E. The Future Oral and Dental Workforce for England: Liberating human resources to serve the population across the life-course. 2019. Available at https://www.hee.nhs.uk/sites/default/files/documents/FDWF%20Report%20-%207th%20March%202019.pdf (accessed May 2021).
World Health Organisation. Coronavirus disease (COVID-19) pandemic. 2020. Available online at https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed May 2021).
Armstrong M. Coronavirus: Bringing dentistry back from the brink. 2020. Available at https://bda.org/news-centre/blog/Pages/Coronavirus-Bringing-dentistry-back-from-the-brink.aspx (accessed September 2020).
Wilson R F, Coward P Y, Capewell J, Laidler T L, Rigby A C, Shaw T J. Perceived sources of occupational stress in general dental practitioners. Br Dent J 1998; 184: 499-502.
British Dental Association. Salaried Primary Dental Care Service Morale Survey. London: BDA, 2011.
Edwards H, Kemp M. Morale and Motivation of Dentists in the Salaried Primary Dental Care Service. London: BDA, 2012.
Boyles J D, Ahmed B. Does student debt affect dental students' and dentists' stress levels? Br Dent J 2017; 223: 601.
McGregor S. Neoliberalism and health care. Int J Consum Stud 2001; 25: 82-89.
NHS England. NHS England Long Term Plan. London: NHS England, 2019.
Francis T, Hoefel F. 'True Gen': Generation Z and its implications for companies. 2018. Available at https://www.mckinsey.com/industries/consumer-packaged-goods/our-insights/true-gen-generation-z-and-its-implications-for-companies# (accessed May 2021).
Armstrong M. The dental profession's mental health crisis: what needs to happen. 2020. Available at https://bda.org/news-centre/blog/Pages/The-dental-professions-mental-health-crisis.aspx (accessed September 2020).
World Health Organisation. Global strategy on human resources for health: Workforce 2030. 2016. Available online at http://www.who.int/hrh/resources/pub_globstrathrh-2030/en/ (accessed May 2021).
Acknowledgements
The authors would like to thank Public Health England for funding this project, key gatekeepers across the country for their support in the recruitment process and all the dentists who participated in this study. Our thanks also to Dr Jim Aukett, who provided advice on an early version of this manuscript, and Sukriti KC who helped during its revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
SW and JEG work for Public Health England and FCS currently works for the National Audit Office. The views expressed do not represent the views of the above organisations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Gallagher, J., Colonio-Salazar, F. & White, S. Supporting dentists' health and wellbeing - workforce assets under stress: a qualitative study in England. Br Dent J (2021). https://doi.org/10.1038/s41415-021-3130-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41415-021-3130-9
This article is cited by
-
What, when and who determines foundation dentists' views about a future career in NHS general dental practice: a post-pandemic qualitative study by peers
British Dental Journal (2026)
-
Key determinants of health and wellbeing of dental nurses: a rapid review of over two decades of research
BDJ Open (2025)
-
Waiting in line for a check-up: evaluating access to NHS dental services in England
British Dental Journal (2025)
-
Me, we, they: identifying the key stressors affecting the dental team
British Dental Journal (2025)
-
Dental careers: findings of a national dental workforce survey
British Dental Journal (2025)