Abstract
Aim To explore the attitudes of general dental practitioners (GDPs) towards testing for diabetes in periodontitis patients amid recommendations from professional organisations that dentists and oral health professionals are well-positioned to support the diagnosis of diabetes in primary dental care.
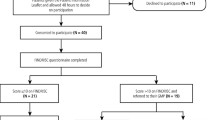
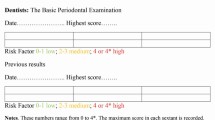
Method GDPs were selected based on purposeful sampling. The number of GDPs recruited was dependent on thematic saturation. Semi-structured telephone interviews were conducted with all recruited GDPs. Interviews were audio recorded and transcribed verbatim. Thematic analysis was utilised to generate initial codes and subsequent themes.
Results Fifteen GDPs participated in this qualitative study. Three main interrelated themes emerged: 1) there is an inadequate infrastructure within the current NHS; 2) the difference in the definition and threshold of the social and professional roles and identities of GDPs; and 3) there is a low self-efficacy to testing due to a perceived lack of knowledge.
Conclusions This qualitative study has identified the barriers to and enablers for testing for diabetes in patients with periodontitis attending general dental practices in England. The findings have the potential to influence interventions and policies going forward to improve the co-management of diabetes and periodontitis within primary healthcare.
Key points
-
NHS-practising GDPs perceived the current infrastructure of the health service to be their biggest barrier to implementation of such testing.
-
All GDPs, whether NHS or private, had varied perspectives on their social and professional role and identity in relation to such testing.
-
Self-efficacy in the realm of testing was generally low due to a lack of perceived knowledge, training and competence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Frencken J E, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis - a comprehensive review. J Clin Periodontol 2017; DOI: 10.1111/jcpe.12677.
Tonetti M S, Chapple I L C, Working Group 3 of Seventh European Workshop on Periodontology. Biological approaches to the development of novel periodontal therapies - consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 2011; DOI: 10.1111/j.1600-051X.2010.01675.x.
Dommisch H, Kuzmanova D, Jönsson D, Grant M, Chapple I. Effect of micronutrient malnutrition on periodontal disease and periodontal therapy. Periodontol 2000 2018; 78: 129-153.
Chapple L, Chapple I. Risk assessment in periodontal disease. Dent Update 2018; 45: 920-926.
Royal College of Surgeons. Position Statement: Oral Health and General Health. 2019. Available at https://www.rcseng.ac.uk/dental-faculties/fds/faculty/government-relations-and-consultation/fds-reports/ (accessed May 2022).
Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type1 and Type2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012; 29: 855-862.
Graziani F, Gennai S, Solini A, Petrini M. A systematic review and meta-analysis of epidemiologic observational evidence on the effect of periodontitis on diabetes An update of the EFP-AAP review. J Clin Periodontol 2018; 45: 167-187.
Kocher T, König J, Borgnakke W S, Pink C, Meisel P. Periodontal complications of hyperglycaemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontol 2000 2018; 78: 59-97.
Preshaw P M, Bissett S M. Periodontitis and diabetes. Br Dent J 2019; 227: 577-584.
National Institute for Health and Care Excellence. Type 2 diabetes: prevention in people at high risk Public health guideline [PH38]. 2017. Available at https://www.nice.org.uk/guidance/ph38 (accessed May 2022).
Sanz M, Herrera D, Kebschull M et al. Treatment of Stage I-III Periodontitis - The EFP S3 level clinical practice guideline. J Clin Periodontol 2020; DOI: 10.1111/jcpe.13290.
Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: A worked example from a synthesis on parental perceptions of vaccination communication. BMC Med Res Methodol 2019; DOI: 10.1186/s12874-019-0665-4.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2008; 3: 77-101.
Atkins L, Francis J, Islam R et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci 2017; DOI: 10.1186/s13012-017-0605-9.
Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004; 82: 581-629.
Goh G, Ower P, Eaton K. The prevalence of potentially undiagnosed type II diabetes in patients with chronic periodontitis attending a general dental practice in London - a feasibility study. Br Dent J 2021; 231: 180-186.
Bélanger E, Rodríguez C. More than the sum of its parts? A qualitative research synthesis on multi-disciplinary primary care teams. J Interprof Care 2008; 22: 587-597.
Exworthy M, Morcillo V. Primary care doctors' understandings of and strategies to tackle health inequalities: a qualitative study. Prim Heal Care Res Dev 2019; DOI: 10.1017/S146342361800052X.
Bissett S M, Stone K M, Rapley T, Preshaw P M. An exploratory qualitative interview study about collaboration between medicine and dentistry in relation to diabetes management. BMJ Open 2013; DOI: 10.1136/bmjopen-2012-002192.
Yonel Z, Yahyouche A, Jalal Z, James A, Dietrich T, Chapple I L C. Patient acceptability of targeted risk-based detection of non-communicable diseases in a dental and pharmacy setting. BMC Public Health 2020; DOI: 10.1186/s12889-020-09649-7.
Sansom A, Terry R, Fletcher E et al. Why do GPs leave direct patient care and what might help to retain them? A qualitative study of GPs in South West England. BMJ Open 2018; DOI: 10.1136/bmjopen-2017-019849.
Michie S, van Stralen M M, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci 2011; DOI: 10.1186/1748-5908-6-42.
Department of Health. NHS dental services in England: an independent review led by Professor Jimmy Steele. 2009. Available at http://www.sigwales.org/wp-content/uploads/dh_101180.pdf (accessed May 2022).
Pumerantz A S, Bissett S M, Dong F et al. Standardized screening for periodontitis as an integral part of multidisciplinary management of adults with type 2 diabetes: an observational cross-sectional study of cohorts in the USA and UK. BMJ Open Diabetes Res Care 2017; DOI: 10.1136/bmjdrc-2017-000413.
UK Government. The NHS Constitution for England. 2021. Available at https://www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england (accessed October 2021).
O'Connor P M, Harper C A, Brunton C L, Clews S J, Haymes S A, Keeffe J E. Shared care for chronic eye diseases: perspectives of ophthalmologists, optometrists and patients. Med J Aust 2012; 196: 646-650.
Alderwick H, Dixon J. The NHS long term plan. BMJ 2019; DOI: 10.1136/bmj.l84.
NHS England. Commissioning Standard: Dental Care for People with Diabetes. 2019. Available at https://www.england.nhs.uk/publication/commissioning-standard-dental-care-for-people-with-diabetes/ (accessed October 2021).
Greenhalgh T, Wherton J, Papoutsi C et al. Beyond Adoption: A New Framework for Theorizing and Evaluating Nonadoption, Abandonment, and Challenges to the Scale-Up, Spread, and Sustainability of Health And Care Technologies. J Med Internet Res 2017; DOI: 10.2196/jmir.8775.
Francis J J, O'Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci 2012; DOI: 10.1186/1748-5908-7-35.
General Medical Council. Good practice in prescribing and managing medicines and devices. 2021. Available at https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-practice-in-prescribing-and-managing-medicines-and-devices (accessed May 2022).
Stange K C. The problem of fragmentation and the need for integrative solutions. Ann Fam Med 2009; 7: 100-103.
Health Education England. Advancing Dental Care: Education and Training Review: Final Report. 2018. Available at https://www.hee.nhs.uk/sites/default/files/documents/advancing_dental_care_final.pdf (accessed May 2022).
Author information
Authors and Affiliations
Contributions
Varkha Rattu designed the study, collected the data, analysed the data, wrote the first draft of the manuscript and edited subsequent draft manuscripts until the final version was agreed. Dominic Hurst advised on the design of the study, contributed to data analysis, edited the manuscript and agreed its final version.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Rattu, V., Hurst, D. Why don't general dental practitioners test for diabetes in periodontitis patients? How infrastructure, role identity and self-efficacy can prevent effective shared care. Br Dent J 232, 798–803 (2022). https://doi.org/10.1038/s41415-022-4294-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41415-022-4294-7