Abstract
Background
Percutaneous thermal ablation is a curative-intent locoregional therapy (LRT) for selected patients with unresectable colorectal liver metastasis (CLM). Several factors have been identified that contribute to local tumour control after ablation. However, factors contributing to disease progression outside the ablation zone after ablation are poorly understood.
Methods
In this retrospective study, using next-generation sequencing, we identified genetic biomarkers associated with different patterns of progression following thermal ablation of CLM.
Results
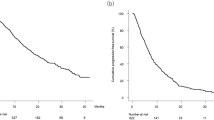
A total of 191 ablation naïve patients between January 2011 and March 2020 were included in the analysis, and 101 had genomic profiling available. Alterations in the TGFβ pathway were associated with increased risk of development of new intrahepatic tumours (hazard ratio [HR], 2.75, 95% confidence interval [95% CI] 1.39–5.45, P = 0.004); and alterations in the Wnt pathway were associated with increased probability of receiving salvage LRT for any intrahepatic progression (HR, 5.8, 95% CI 1.94–19.5, P = 0.003).
Conclusions
Our findings indicate that genomic alterations in cancer-related signalling pathways can predict different progression patterns and the likelihood of receiving salvage LRT following percutaneous thermal ablation of CLM.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available because of human subjects' privacy concerns and institutional policies. Anonymized data are available from the corresponding author upon reasonable request.
Code availability
The complete R code for the statistical analysis is available in the supplementary materials.
References
Valderrama-Trevino AI, Barrera-Mera B, Ceballos-Villalva JC, Montalvo-Jave EE. Hepatic metastasis from colorectal cancer. Euroasian J Hepatogastroenterol. 2017;7:166–75.
Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283–301.
Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ. Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer. 2014;14:810.
Lin YM, Paolucci I, Brock KK, Odisio BC. Image-guided ablation for colorectal liver metastasis: principles, current evidence, and the path forward. Cancers. 2021;13:3926.
Kron P, Linecker M, Jones RP, Toogood GJ, Clavien PA, Lodge JPA. Ablation or resection for colorectal liver metastases? A systematic review of the literature. Front Oncol. 2019;9:1052.
Gillams A, Goldberg N, Ahmed M, Bale R, Breen D, Callstrom M, et al. Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, The Interventional Oncology Sans Frontieres meeting 2013. Eur Radiol. 2015;25:3438–54.
Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Jiang BB, Yan K, Zhang ZY, Yang W, Wu W, Yin SS, et al. The value of KRAS gene status in predicting local tumor progression of colorectal liver metastases following radiofrequency ablation. Int J Hyperthermia. 2019;36:211–9.
Calandri M, Yamashita S, Gazzera C, Fonio P, Veltri A, Bustreo S, et al. Ablation of colorectal liver metastasis: interaction of ablation margins and RAS mutation profiling on local tumour progression-free survival. Eur Radiol. 2018;28:2727–34.
Odisio BC, Yamashita S, Huang SY, Harmoush S, Kopetz SE, Ahrar K, et al. Local tumour progression after percutaneous ablation of colorectal liver metastases according to RAS mutation status. Br J Surg. 2017;104:760–8.
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24.
Singh RR, Patel KP, Routbort MJ, Reddy NG, Barkoh BA, Handal B, et al. Clinical validation of a next-generation sequencing screen for mutational hotspots in 46 cancer-related genes. J Mol Diagn. 2013;15:607–22.
Rajagopalan H, Bardelli A, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE. Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature. 2002;418:934.
Sanchez-Vega F, Mina M, Armenia J, Chatila WK, Luna A, La KC, et al. Oncogenic signaling pathways in the cancer genome atlas. Cell. 2018;173:321–37. e310
Odisio BC, Yamashita S, Huang SY, Kopetz SE, Ahrar K, Mizuno T, et al. Impact of prior hepatectomy history on local tumor progression after percutaneous ablation of colorectal liver metastases. J Vasc Interv Radiol. 2018;29:395–403. e391
Anderson BM, Lin YM, Lin EY, Cazoulat G, Gupta S, Kyle Jones A, et al. A novel use of biomechanical model-based deformable image registration (DIR) for assessing colorectal liver metastases ablation outcomes. Med Phys. 2021;48:6226–36.
Anderson BM, Lin EY, Cardenas CE, Gress DA, Erwin WD, Odisio BC, et al. Automated contouring of contrast and noncontrast computed tomography liver images with fully convolutional networks. Adv Radiat Oncol. 2021;6:100464.
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria−a 10-year update. J Vasc Interv Radiol. 2014;25:1691–705. e1694
Puijk RS, Ahmed M, Adam A, Arai Y, Arellano R, de Baere T, et al. Consensus guidelines for the definition of time-to-event end points in image-guided tumor ablation: results of the SIO and DATECAN initiative. Radiology. 2021;301:533–40.
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019.
Alboukadel Kassambara. ggpubr: ’ggplot2’ Based Publication Ready Plots. R package version 0.4.0. 2020. https://CRAN.R-project.org/package=ggpubr.
Wickham H. ggplot2: elegant graphics for data analysis. 2nd edn. New York: Springer-Verlag; 2016.
Wickham H, Averick M, Bryan J, Chang W, McGowan L, Françoi R, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4:1686.
Andreou A, Knitter S, Schmelzle M, Kradolfer D, Maurer MH, Auer TA, et al. Recurrence at surgical margin following hepatectomy for colorectal liver metastases is not associated with R1 resection and does not impact survival. Surgery. 2021;169:1061–8.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing hepatectomy in colorectal liver metastasis improves salvageability and survival. Ann Surg. 2016;263:146–52.
Kawaguchi Y, Kopetz S, Kwong L, Xiao L, Morris JS, Tran Cao HS, et al. Genomic sequencing and insight into clinical heterogeneity and prognostic pathway genes in patients with metastatic colorectal cancer. J Am Coll Surg. 2021;233:272–84. e213
Shady W, Petre EN, Gonen M, Erinjeri JP, Brown KT, Covey AM, et al. Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes—a 10-year experience at a single center. Radiology. 2016;278:601–11.
Solbiati L, Ahmed M, Cova L, Ierace T, Brioschi M, Goldberg SN. Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology. 2012;265:958–68.
Ruiter SJS, Tinguely P, Paolucci I, Engstrand J, Candinas D, Weber S, et al. 3D quantitative ablation margins for prediction of ablation site recurrence after stereotactic image-guided microwave ablation of colorectal liver metastases: a multicenter study. Front Oncol. 2021;11.
Shady W, Petre EN, Do KG, Gonen M, Yarmohammadi H, Brown KT, et al. Percutaneous microwave versus radiofrequency ablation of colorectal liver metastases: ablation with clear margins (A0) provides the best local tumor control. J Vasc Interv Radiol. 2018;29:268–75. e261
Laimer G, Schullian P, Jaschke N, Putzer D, Eberle G, Alzaga A, et al. Minimal ablative margin (MAM) assessment with image fusion: an independent predictor for local tumor progression in hepatocellular carcinoma after stereotactic radiofrequency ablation. Eur Radiol. 2020;30:2463–72.
Puijk RS, Ahmed M, Adam A, Arai Y, Arellano R, de Baere T, et al. Consensus guidelines for the definition of time-to-event end points in image-guided tumor ablation: results of the SIO and DATECAN initiative. Radiology. 2021;203715; https://doi.org/10.1148/radiol.2021203715.
Acknowledgements
We thank Stephanie Deming, Research Medical Library, MD Anderson Cancer Center, for editing the manuscript.
Funding
IP is funded by a PostDoc Mobility Fellowship from the Swiss National Science Foundation under project number P2BEP3_195444. Research reported in this publication was supported in part by the National Cancer Institute of the National Institutes of Health under award numbers R01CA235564 and P30CA016672 and by the Image Guided Cancer Therapy Research Program at The University of Texas MD Anderson Cancer Center.
Author information
Authors and Affiliations
Contributions
IP, BCO and JNV: study design; IP, YML and BCO: writing and editing; IP, YML, BCO, YK and HM: data collection and data review; IP: statistical analysis; IP, YML, YK, HM, AKJ, MC, SK, TN, KKB and BCO: critical review and editing; BCO: supervision of the project. All authors have read and agreed to this version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This retrospective study was approved by The University of Texas MD Anderson Cancer Center Institutional Review Board (Nr: 2021-0340) and conducted in accordance with the Declaration of Helsinki. The requirement for written informed consent was waived.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Paolucci, I., Lin, YM., Kawaguchi, Y. et al. Targeted exome-based predictors of patterns of progression of colorectal liver metastasis after percutaneous thermal ablation. Br J Cancer 128, 130–136 (2023). https://doi.org/10.1038/s41416-022-02030-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-022-02030-y