Abstract
Background
Despite the increasing incidence in colorectal cancer (CRC) among the young population, the involvement of modifiable early-life exposures is understudied.
Methods
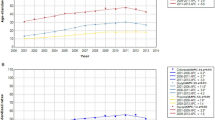
We prospectively investigated the association of lifestyle score, which measures adherence to the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) cancer prevention recommendations, in adolescence and adulthood with risk of CRC precursors in 34,509 women enrolled in the Nurses’ Health Study II. Participants reported adolescent diet in 1998 and subsequently underwent at least one lower gastrointestinal endoscopy between 1999 and 2015. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using multivariable logistic regression for clustered data.
Results
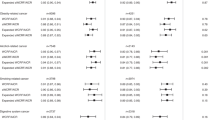
During follow-up (1998–2015), 3036 women had at least one adenoma, and 2660 had at least one serrated lesion. In multivariable analysis, per unit increase in adolescent WCRF/AICR lifestyle score was not associated with risk of total adenoma or serrated lesions, in contrast to adult WCRF/AICR lifestyle score (OR = 0.92, 95% CI: 0.87–0.97, Ptrend = 0.002 for total adenoma; and OR = 0.86, 95% CI: 0.81–0.92, Ptrend < 0.001 for total serrated lesions).
Conclusion
Adherence to the 2018 WCRF/AICR recommendations during adulthood but not during adolescence was associated with a lower risk of CRC precursors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Further information including the procedures to obtain and access data from the Nurses’ Health Study is described at https://www.nurseshealthstudy.org/researchers (e-mail: nhsaccess@channing.harvard.edu).
References
Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. 2021;71:209–49.
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–91.
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145–64.
Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109:djw322.
Siegel RL, Torre LA, Soerjomataram I, Hayes RB, Bray F, Weber TK, et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut. 2019;68:2179–85.
Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–73.
Cao Y, Rosner BA, Ma J, Tamimi RM, Chan AT, Fuchs CS, et al. Assessing individual risk for high-risk colorectal adenoma at first-time screening colonoscopy. Int J Cancer. 2015;137:1719–28.
He X, Wu K, Ogino S, Giovannucci EL, Chan AT, Song M. Association between risk factors for colorectal cancer and risk of serrated polyps and conventional adenomas. Gastroenterology. 2018;155:355–73.e18.
Hawkins N, Norrie M, Cheong K, Mokany E, Ku SL, Meagher A, et al. CpG island methylation in sporadic colorectal cancers and its relationship to microsatellite instability. Gastroenterology. 2002;122:1376–87.
Spring KJ, Zhao ZZ, Karamatic R, Walsh MD, Whitehall VLJ, Pike T, et al. High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006;131:1400–7.
Strum WB. Colorectal adenomas. N Engl J Med. 2016;374:1065–75.
Nimptsch K, Malik VS, Fung TT, Pischon T, Hu FB, Willett WC, et al. Dietary patterns during high school and risk of colorectal adenoma in a cohort of middle-aged women. Int J Cancer. 2014;134:2458–67.
Joh HK, Lee DH, Hur J, Nimptsch K, Chang Y, Joung H, et al. Simple sugar and sugar-sweetened beverage intake during adolescence and risk of colorectal cancer precursors. Gastroenterology. 2021;161:128–42 e20.
Rezende LFM, Lee DH, Keum N, Nimptsch K, Song M, Lee IM, et al. Physical activity during adolescence and risk of colorectal adenoma later in life: results from the Nurses’ Health Study II. Br J Cancer. 2019;121:86–94.
Zheng X, Hur J, Nguyen LH, Liu J, Song M, Wu K, et al. Comprehensive assessment of diet quality and risk of precursors of early-onset colorectal cancer. JNCI: J Natl Cancer Inst. 2021;113:543–52.
Hur J, Otegbeye E, Joh H-K, Nimptsch K, Ng K, Ogino S, et al. Sugar-sweetened beverage intake in adulthood and adolescence and risk of early-onset colorectal cancer among women. Gut. 2021;70:2330–6.
Yue Y, Hur J, Cao Y, Tabung FK, Wang M, Wu K, et al. Prospective evaluation of dietary and lifestyle pattern indices with risk of colorectal cancer in a cohort of younger women. Ann Oncol. 2021;32:778–86.
Giovannucci E. Molecular biologic and epidemiologic insights for preventability of colorectal cancer. JNCI: J Natl Cancer Inst. 2022;114:645–50.
Lahouel K, Younes L, Danilova L, Giardiello FM, Hruban RH, Groopman J, et al. Revisiting the tumorigenesis timeline with a data-driven generative model. Proc Natl Acad Sci USA. 2020;117:857–64.
Zhang Y, Chan AT, Meyerhardt JA, Giovannucci EL. Timing of aspirin use in colorectal cancer chemoprevention: a prospective cohort study. J Natl Cancer Inst. 2021;113:841–51.
Michels KB, Willett WC, Vaidya R, Zhang X, Giovannucci E. Yogurt consumption and colorectal cancer incidence and mortality in the Nurses’ Health Study and the Health Professionals Follow-Up Study. Am J Clin Nutr. 2020;112:1566–75.
Lee JE, Willett WC, Fuchs CS, Smith-Warner SA, Wu K, Ma J, et al. Folate intake and risk of colorectal cancer and adenoma: modification by time. Am J Clin Nutr. 2011;93:817–25.
Luebeck EG, Moolgavkar SH, Liu AY, Boynton A, Ulrich CM. Does folic acid supplementation prevent or promote colorectal cancer? Results from model-based predictions. Cancer Epidemiol Biomark Prev. 2008;17:1360–7.
Akimoto N, Ugai T, Zhong R, Hamada T, Fujiyoshi K, Giannakis M, et al. Rising incidence of early-onset colorectal cancer—a call to action. Nat Rev Clin Oncol. 2021;18:230–43.
World Cancer Research Fund/American Institute for Cancer Research Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report 2018. Available http://dietandcancerreport.org. Accessed 2 Nov 2021.
Shams-White MM, Brockton NT, Mitrou P, Romaguera D, Brown S, Bender A, et al. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) cancer prevention recommendations: a standardized scoring system. Nutrients. 2019;11:1572.
Petimar J, Smith-Warner SA, Rosner B, Chan AT, Giovannucci EL, Tabung FK. Adherence to the World Cancer Research Fund/American Institute for Cancer Research 2018 recommendations for cancer prevention and risk of colorectal cancer. Cancer Epidemiol Biomark Prev. 2019;28:1469–79.
Korn AR, Reedy J, Brockton NT, Kahle LL, Mitrou P, Shams-White MM. The 2018 World Cancer Research Fund/American Institute for Cancer Research score and cancer risk: a longitudinal analysis in the NIH-AARP diet and health study. Cancer Epidemiol Biomark Prev. 2022;31:1983–92.
Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, et al. Origin, methods, and evolution of the three Nurses’ Health Studies. Am J Public Health. 2016;106:1573–81.
Maruti SS, Feskanich D, Colditz GA, Frazier AL, Sampson LA, Michels KB, et al. Adult recall of adolescent diet: reproducibility and comparison with maternal reporting. Am J Epidemiol. 2005;161:89–97.
Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–9.
Al-Shaar L, Pernar CH, Chomistek AK, Rimm EB, Rood J, Stampfer MJ, et al. Reproducibility, validity, and relative validity of self-report methods for assessing physical activity in epidemiologic studies: findings from the women’s lifestyle validation study. Am J Epidemiol. 2022;191:696–710.
Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122:327–34.
He X, Hang D, Wu K, Nayor J, Drew DA, Giovannucci EL, et al. Long-term risk of colorectal cancer after removal of conventional adenomas and serrated polyps. Gastroenterology. 2020;158:852–61 e4.
Gupta S, Lieberman D, Anderson JC, Burke CA, Dominitz JA, Kaltenbach T, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US multi-society task force on colorectal cancer. Am J Gastroenterol. 2020;115:415–34.
Gill P, Wang LM, Bailey A, East JE, Leedham S, Chetty R. Reporting trends of right-sided hyperplastic and sessile serrated polyps in a large teaching hospital over a 4-year period (2009-2012). J Clin Pathol. 2013;66:655–8.
Andersen PK, Gill RD. Cox’s regression model for counting processes: a large sample study. Ann Stat. 1982;10:1100–20. 21
Wark PA, Wu K, Van T, Veer P, Fuchs CF, Giovannucci EL. Family history of colorectal cancer: a determinant of advanced adenoma stage or adenoma multiplicity? Int J Cancer. 2009;125:413–20.
Benjamin DJ, Berger JO, Johannesson M, Nosek BA, Wagenmakers EJ, Berk R, et al. Redefine statistical significance. Nat Hum Behav. 2018;2:6–10.
Nimptsch K, Bernstein AM, Giovannucci E, Fuchs CS, Willett WC, Wu K. Dietary intakes of red meat, poultry, and fish during high school and risk of colorectal adenomas in women. Am J Epidemiol. 2013;178:172–83.
Nimptsch K, Lee DH, Zhang X, Song M, Farvid MS, Rezende LFM, et al. Dairy intake during adolescence and risk of colorectal adenoma later in life. Br J Cancer. 2021;124:1160–8.
Nimptsch K, Wu K. Is timing important? The role of diet and lifestyle during early life on colorectal neoplasia. Curr Colorectal Cancer Rep. 2018;14:1–11.
Song R, Petimar J, Wang M, Tabung FK, Song M, Liu L, et al. Adherence to the World Cancer Research Fund/American Institute for cancer research cancer prevention recommendations and colorectal cancer survival. Cancer Epidemiol Biomark Prev. 2021;30:1816–25.
Ruder EH, Thiebaut AC, Thompson FE, Potischman N, Subar AF, Park Y, et al. Adolescent and mid-life diet: risk of colorectal cancer in the NIH-AARP diet and health study. Am J Clin Nutr. 2011;94:1607–19.
Baron JA, Beach M, Mandel JS, Van Stolk RU, Haile RW, Sandler RS, et al. Calcium supplements for the prevention of colorectal adenomas. N Engl J Med. 1999;340:101–7.
Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB. Key Findings on alcohol consumption and a variety of health outcomes from the Nurses’ Health Study. Am J Public Health. 2016;106:1586–91.
Esser MB, Clayton H, Demissie Z, Kanny D, Brewer RD. Current and binge drinking among high school students—United States, 1991–2015. MMWR Morb Mortal Wkly Rep. 2017;66:474–8.
Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. West J Med. 2000;173:378–83.
Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. youth, 2011–2014. NCHS Data Brief. 2017;1–8.
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Bertrand KA, Baer HJ, Orav EJ, Klifa C, Shepherd JA, Van Horn L, et al. Body fatness during childhood and adolescence and breast density in young women: a prospective analysis. Breast Cancer Res. 2015;17:95.
Maruti SS, Feskanich D, Rockett HR, Colditz GA, Sampson LA, Willett WC. Validation of adolescent diet recalled by adults. Epidemiology. 2006;17:226–9.
Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC. Premenopausal dietary fat in relation to pre- and post-menopausal breast cancer. Breast Cancer Res Treat. 2014;145:255–65.
Farvid MS, Cho E, Chen WY, Eliassen AH, Willett WC. Adolescent meat intake and breast cancer risk. Int J Cancer. 2015;136:1909–20.
Farvid MS, Chen WY, Michels KB, Cho E, Willett WC, Eliassen AH. Fruit and vegetable consumption in adolescence and early adulthood and risk of breast cancer: population based cohort study. BMJ. 2016;353:i2343.
American Cancer Society. Colorectal cancer facts & figures 2020–2022. Atlanta, GA: American Cancer Society; 2020.
Acknowledgements
The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Central registries may also be supported by state agencies, universities, and cancer centres. Participating central cancer registries include the following: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Maine, Maryland, Michigan, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Seattle SEER Registry, South Carolina, Tennessee, Texas, Utah, Virginia, West Virginia, Wyoming.
Funding
This work was supported by the National Institutes of Health (NHSII infrastructure grant of U01 CA176726 and R37 CA246175 to Yin Cao). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. JH was supported by a research grant from the Ottogi Ham Taiho Foundation.
Author information
Authors and Affiliations
Contributions
SZ, RS and PW had full access to all the data and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: EG, JH, YC and KW. Acquisition, analysis or interpretation of the data: SZ, JH and EG. Drafting of the manuscript: SZ, JH and EG. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: SZ.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the institutional review boards of the Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, and those of participating registries as required. Completion of the questionnaire was considered to imply informed consent.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, S., Hur, J., Song, R. et al. Adherence to the World Cancer Research Fund/American Institute for Cancer Research cancer prevention recommendations throughout the life course and risk of colorectal cancer precursors. Br J Cancer 128, 2243–2252 (2023). https://doi.org/10.1038/s41416-023-02255-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41416-023-02255-5
This article is cited by
-
Plasma metabolite profiles related to dietary patterns: exploring the association with colorectal tumor risk
European Journal of Nutrition (2025)
-
Association between being breastfed in infancy and adult colorectal cancer risk among Japanese men and women
Scientific Reports (2024)