Abstract
Background
The poor prognosis of resectable esophageal squamous cell carcinoma (ESCC) poses an unmet need to identify early predictive and prognostic genomic biomarkers to improve treatment outcome and risk stratification.
Methods
Mutational profiling was performed for 171 ESCC patients receiving curative neoadjuvant chemoradiation treatment (nCRT). The discovery cohort included 100 ESCC formalin-fixed paraffin-embedded (FFPE) tumor specimens; the validation FFPE cohort consisted of serial ctDNA samples from 71 patients.
Results
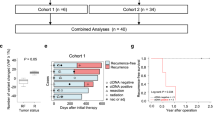
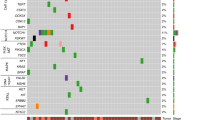
The discovery cohort identified hot-spot oncogenic NFE2L2 mutations exclusively localized at DLG and ETGE KEAP1-binding motifs in poor responders associated with incomplete pathological response (P = 0.004). Patients with NFE2L2 mutations in two independent FFPE cohorts had about 2-fold higher risk of death and recurrence. Serial ctDNA analysis further demonstrated oncogenic NFE2L2 mutations detected at post-nCRT were independent prognosticators for recurrence (HR = 5.90; P = 0.005) and survival (HR = 4.75; P = 0.013). Risk stratification based on pathological T and N stages, positive FFPE (HR = 4.50) and ctDNA NFE2L2 mutations (HR = 8.50) identified high-risk groups for recurrence (P = 0.001). Combined FFPE and ctDNA NFE2L2 mutation status predicted nCRT responses (P = 0.05) by ROC analysis.
Conclusions
Tracking oncogenic NFE2L2 mutations at pre-treatment and post-surgery or serial ctDNA monitoring during treatment are useful nCRT predictors and independent prognosticators of survival for locally advanced ESCC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data supporting the findings of this study are available from the corresponding author upon request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. https://doi.org/10.3322/caac.21492
Smyth EC, Lagergren J, Fitzgerald RC, Lordick F, Shah MA, Lagergren P, et al. Oesophageal cancer. Nat Rev Dis Primers. 2017;3:17048 https://doi.org/10.1038/nrdp.2017.48
Wang S, Zheng R, Arnold M, Abnet C, Zeng H, Zhang S, et al. Global and national trends in the age-specific sex ratio of esophageal cancer and gastric cancer by subtype. Int J Cancer. 2022;151:1447–61. https://doi.org/10.1002/ijc.34158
Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64:381–7. https://doi.org/10.1136/gutjnl-2014-308124
Shapiro J, Van Lanschot JJB, Hulshof M, Van Hagen P, Van Berge Henegouwen MI, Wijnhoven BPL, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16:1090–8. https://doi.org/10.1016/S1470-2045(15)00040-6
Yang H, Liu H, Chen Y, Zhu C, Fang W, Yu Z, et al. Neoadjuvant chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the esophagus (NEOCRTEC5010): A phase III multicenter, randomized, open-label clinical trial. J Clin Oncol. 2018;36:2796–803. https://doi.org/10.1200/JCO.2018.79.1483
Tong DK, Law S, Kwong DL, Chan KW, Lam AK, Wong KH. Histological regression of squamous esophageal carcinoma assessed by percentage of residual viable cells after neoadjuvant chemoradiation is an important prognostic factor. Ann Surg Oncol. 2010;17:2184–92. https://doi.org/10.1245/s10434-010-0995-2
Chirieac LR, Swisher SG, Ajani JA, Komaki RR, Correa AM, Morris JS, et al. Posttherapy pathologic stage predicts survival in patients with esophageal carcinoma receiving preoperative chemoradiation. Cancer. 2005;103:1347–55. https://doi.org/10.1002/cncr.20916
Meredith KL, Weber JM, Turaga KK, Siegel EM, Mcloughlin J, Hoffe S, et al. Pathologic response after neoadjuvant therapy is the major determinant of survival in patients with esophageal cancer. Ann Surg Oncol. 2010;17:1159–67. https://doi.org/10.1245/s10434-009-0862-1
Blum Murphy M, Xiao L, Patel VR, Maru DM, Correa AM, G Amlashi F, et al. Pathological complete response in patients with esophageal cancer after the trimodality approach: The association with baseline variables and survival-The University of Texas MD Anderson Cancer Center experience. Cancer. 2017;123:4106–13. https://doi.org/10.1002/cncr.30953
Gao YB, Chen ZL, Li JG, Hu XD, Shi XJ, Sun ZM, et al. Genetic landscape of esophageal squamous cell carcinoma. Nat Genet. 2014;46:1097–102. https://doi.org/10.1038/ng.3076
Lin DC, Hao JJ, Nagata Y, Xu L, Shang L, Meng X, et al. Genomic and molecular characterization of esophageal squamous cell carcinoma. Nat Genet. 2014;46:467–73. https://doi.org/10.1038/ng.2935
Song Y, Li L, Ou Y, Gao Z, Li E, Li X, et al. Identification of genomic alterations in oesophageal squamous cell cancer. Nature. 2014;509:91–5. https://doi.org/10.1038/nature13176
Sawada G, Niida A, Uchi R, Hirata H, Shimamura T, Suzuki Y, et al. Genomic Landscape of Esophageal Squamous Cell Carcinoma in a Japanese Population. Gastroenterology. 2016;150:1171–82. https://doi.org/10.1053/j.gastro.2016.01.035
Ko JM, Guo C, Liu C, Ning L, Dai W, Tao L, et al. Clonal relationship and alcohol consumption-associated mutational signature in synchronous hypopharyngeal tumours and oesophageal squamous cell carcinoma. Br J Cancer. 2022;127:2166–74. https://doi.org/10.1038/s41416-022-01995-0
Dai W, Ko JMY, Choi SSA, Yu Z, Ning L, Zheng H, et al. Whole-exome sequencing reveals critical genes underlying metastasis in oesophageal squamous cell carcinoma. J Pathol. 2017;242:500–10. https://doi.org/10.1002/path.4925
Merker JD, Oxnard GR, Compton C, Diehn M, Hurley P, Lazar AJ, et al. Circulating tumor DNA analysis in patients with cancer: American Society of Clinical Oncology and College of American Pathologists Joint Review. J Clin Oncol. 2018;36:1631–41. https://doi.org/10.1200/JCO.2017.76.8671
Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6:224ra24 https://doi.org/10.1126/scitranslmed.3007094
Ng, HY, Ko, JMY, Lam, KO, Kwong, DLW, Lo, AWI, Wong, IYH, et al. Circulating tumor DNA dynamics as prognostic markers in locally advanced and metastatic esophageal squamous cell carcinoma. JAMA Surg https://doi.org/10.1001/jamasurg.2023.4395 (2023).
Denicola GM, Karreth FA, Humpton TJ, Gopinathan A, Wei C, Frese K, et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature. 2011;475:106–9. https://doi.org/10.1038/nature10189
Canning P, Sorrell FJ, Bullock AN. Structural basis of Keap1 interactions with Nrf2. Free Radic Biol Med. 2015;88:101–7. https://doi.org/10.1016/j.freeradbiomed.2015.05.034
Kitano Y, Baba Y, Nakagawa S, Miyake K, Iwatsuki M, Ishimoto T, et al. Nrf2 promotes oesophageal cancer cell proliferation via metabolic reprogramming and detoxification of reactive oxygen species. J Pathol. 2018;244:346–57. https://doi.org/10.1002/path.5021
Rojo De La Vega M, Chapman E, Zhang DD. NRF2 and the Hallmarks of Cancer. Cancer Cell. 2018;34:21–43. https://doi.org/10.1016/j.ccell.2018.03.022
Lee SB, Sellers BN, Denicola GM. The regulation of NRF2 by nutrient-responsive signaling and its role in anabolic cancer metabolism. Antioxid Redox Signal. 2018;29:1774–91. https://doi.org/10.1089/ars.2017.7356
Cancer Genome Atlas Research, N. Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489:519–25. https://doi.org/10.1038/nature11404
Guan L, Nambiar DK, Cao H, Viswanathan V, Kwok S, Hui AB, et al. NFE2L2 mutations enhance radioresistance in head and neck cancer by modulating intratumoral myeloid cells. Cancer Res. 2023;83:861–74. https://doi.org/10.1158/0008-5472.CAN-22-1903
Jaramillo MC, Zhang DD. The emerging role of the Nrf2-Keap1 signaling pathway in cancer. Genes Dev. 2013;27:2179–91. https://doi.org/10.1101/gad.225680.113
Romero R, Sayin VI, Davidson SM, Bauer MR, Singh SX, Leboeuf SE, et al. Keap1 loss promotes Kras-driven lung cancer and results in dependence on glutaminolysis. Nat Med. 2017;23:1362–8. https://doi.org/10.1038/nm.4407
Binkley MS, Jeon YJ, Nesselbush M, Moding EJ, Nabet BY, Almanza D, et al. KEAP1/NFE2L2 Mutations Predict Lung Cancer Radiation Resistance That Can Be Targeted by Glutaminase Inhibition. Cancer Discov. 2020;10:1826–41. https://doi.org/10.1158/2159-8290.CD-20-0282
Kawasaki Y, Okumura H, Uchikado Y, Kita Y, Sasaki K, Owaki T, et al. Nrf2 is useful for predicting the effect of chemoradiation therapy on esophageal squamous cell carcinoma. Ann Surg Oncol. 2014;21:2347–52. https://doi.org/10.1245/s10434-014-3600-2
Zhang J, Jiao Q, Kong L, Yu J, Fang A, Li M, et al. Nrf2 and Keap1 abnormalities in esophageal squamous cell carcinoma and association with the effect of chemoradiotherapy. Thorac Cancer. 2018;9:726–35. https://doi.org/10.1111/1759-7714.12640
Kim YR, Oh JE, Kim MS, Kang MR, Park SW, Han JY, et al. Oncogenic NRF2 mutations in squamous cell carcinomas of oesophagus and skin. J Pathol. 2010;220:446–51. https://doi.org/10.1002/path.2653
So AP, Vilborg A, Bouhlal Y, Koehler RT, Grimes SM, Pouliot Y, et al. A robust targeted sequencing approach for low input and variable quality DNA from clinical samples. NPJ Genom Med. 2018;3:2 https://doi.org/10.1038/s41525-017-0041-4
Ko, JM, Vardhanabhuti, V, Ng, WT, Lam, KO, Ngan, RK, Kwong, DL et al. Clinical utility of serial analysis of circulating tumour cells for detection of minimal residual disease of metastatic nasopharyngeal carcinoma. Br J Cancer https://doi.org/10.1038/s41416-020-0871-1 (2020).
Zhang SS, Huang QY, Yang H, Xie X, Luo KJ, Wen J, et al. Correlation of p53 status with the response to chemotherapy-based treatment in esophageal cancer: a meta-analysis. Ann Surg Oncol. 2013;20:2419–27. https://doi.org/10.1245/s10434-012-2859-4
Kang N, Wang Y, Guo S, Ou Y, Wang G, Chen J, et al. Mutant TP53 G245C and R273H promote cellular malignancy in esophageal squamous cell carcinoma. BMC Cell Biol. 2018;19:16 https://doi.org/10.1186/s12860-018-0167-y
Li XC, Wang MY, Yang M, Dai HJ, Zhang BF, Wang W, et al. A mutational signature associated with alcohol consumption and prognostically significantly mutated driver genes in esophageal squamous cell carcinoma. Ann Oncol. 2018;29:938–44. https://doi.org/10.1093/annonc/mdy011
Shibata T, Kokubu A, Saito S, Narisawa-Saito M, Sasaki H, Aoyagi K, et al. NRF2 mutation confers malignant potential and resistance to chemoradiation therapy in advanced esophageal squamous cancer. Neoplasia. 2011;13:864–73. https://doi.org/10.1593/neo.11750
Shibata T, Ohta T, Tong KI, Kokubu A, Odogawa R, Tsuta K, et al. Cancer related mutations in NRF2 impair its recognition by Keap1-Cul3 E3 ligase and promote malignancy. Proc Natl Acad Sci USA. 2008;105:13568–73. https://doi.org/10.1073/pnas.0806268105
Feng L, Zhao K, Sun L, Yin X, Zhang J, Liu C, et al. SLC7A11 regulated by NRF2 modulates esophageal squamous cell carcinoma radiosensitivity by inhibiting ferroptosis. J Transl Med. 2021;19:367 https://doi.org/10.1186/s12967-021-03042-7
Azad TD, Chaudhuri AA, Fang P, Qiao Y, Esfahani MS, Chabon JJ, et al. Circulating tumor DNA analysis for detection of minimal residual disease after chemoradiotherapy for localized esophageal cancer. Gastroenterology. 2020;158:494–505 e6. https://doi.org/10.1053/j.gastro.2019.10.039
Eyck BM, Jansen MP, Noordman BJ, Atmodimedjo PN, Van Der Wilk BJ, Martens JW, et al. Detection of circulating tumour DNA after neoadjuvant chemoradiotherapy in patients with locally advanced oesophageal cancer. J Pathol. 2023;259:35–45. https://doi.org/10.1002/path.6016
Baird L, Yamamoto M. Immunoediting of KEAP1-NRF2 mutant tumours is required to circumvent NRF2-mediated immune surveillance. Redox Biol. 2023;67:102904 https://doi.org/10.1016/j.redox.2023.102904
Guan J, Lu C, Jin Q, Lu H, Chen X, Tian L, et al. MLH1 deficiency-triggered DNA hyperexcision by exonuclease 1 activates the cGAS-STING pathway. Cancer Cell. 2021;39:109–21 e5. https://doi.org/10.1016/j.ccell.2020.11.004
Oh MH, Sun IH, Zhao L, Leone RD, Sun IM, Xu W, et al. Targeting glutamine metabolism enhances tumor-specific immunity by modulating suppressive myeloid cells. J Clin Invest. 2020;130:3865–84. https://doi.org/10.1172/JCI131859
Wicker CA, Hunt BG, Krishnan S, Aziz K, Parajuli S, Palackdharry S, et al. Glutaminase inhibition with telaglenastat (CB-839) improves treatment response in combination with ionizing radiation in head and neck squamous cell carcinoma models. Cancer Lett. 2021;502:180–8. https://doi.org/10.1016/j.canlet.2020.12.038
Ren D, Villeneuve NF, Jiang T, Wu T, Lau A, Toppin HA, et al. Brusatol enhances the efficacy of chemotherapy by inhibiting the Nrf2-mediated defense mechanism. Proc Natl Acad Sci USA. 2011;108:1433–8. https://doi.org/10.1073/pnas.1014275108
Xiang Y, Ye W, Huang C, Yu D, Chen H, Deng T, et al. Brusatol enhances the chemotherapy efficacy of gemcitabine in pancreatic cancer via the Nrf2 signalling pathway. Oxid Med Cell Longev. 2018;2018:2360427 https://doi.org/10.1155/2018/2360427
Tian Z, Yang Y, Wu H, Chen Y, Jia H, Zhu L, et al. The Nrf2 inhibitor brusatol synergistically enhances the cytotoxic effect of lapatinib in HER2-positive cancers. Heliyon. 2022;8:e10410 https://doi.org/10.1016/j.heliyon.2022.e10410
Reinert T, Henriksen TV, Christensen E, Sharma S, Salari R, Sethi H, et al. Analysis of plasma cell-free DNA by ultradeep sequencing in patients with stages I to III colorectal cancer. JAMA Oncol. 2019;5:1124–31. https://doi.org/10.1001/jamaoncol.2019.0528
Tie J, Cohen JD, Wang Y, Christie M, Simons K, Lee M, et al. Circulating Tumor DNA analyses as markers of recurrence risk and benefit of adjuvant therapy for stage III colon cancer. JAMA Oncol. 2019;5:1710–7. https://doi.org/10.1001/jamaoncol.2019.3616
Acknowledgements
The study is funded by Hong Kong Research Grants Council Theme-Based Research Scheme grant number T12-701/17-R to MLL.
Author information
Authors and Affiliations
Contributions
Conceptualization: MLL, JMYK, KOL Methodology: JMYK, CG, HYN, WD Formal analysis: CG, AKKL, LT, AKYL Investigation: CG, AKKL, SCYL, LT, CWYW, AKYL Resources: AWIL, SL, IYHW, CLYW, FSYC, KKC, TTL, KOL, DLWK Data curation: AWIL, SL, IYHW, CLYW, FSYC, KKC, TTL, KOL, DLWK Writing – original draft: JMYK, CG Writing – review & editing: JMYK, MLL Visualization: JMYK, CG Supervision: MLL, JMYK Project administration: MLL, JMYK Funding acquisition: MLL, SL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ko, J.MY., Guo, C., Leung, A.KK. et al. Oncogenic NFE2L2 mutations in plasma ctDNA and tumors are predictors and prognosticators of chemoradiation therapy in resectable esophageal squamous cell carcinoma. Br J Cancer 133, 1046–1055 (2025). https://doi.org/10.1038/s41416-025-03113-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03113-2