Abstracts
Background
Identifying molecular alterations specific to advanced lung adenocarcinomas could provide insights into tumour progression and dissemination mechanisms.
Method
We analysed tumour samples, either from locoregional lesions or distant metastases, from patients with advanced lung adenocarcinoma from the SAFIR02-Lung trial by targeted sequencing of 45 cancer genes and comparative genomic hybridisation array and compared them to early tumours samples from The Cancer Genome Atlas.
Results
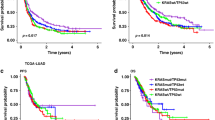
Differences in copy-number alterations frequencies suggest the involvement in tumour progression of LAMB3, TNN/KIAA0040/TNR, KRAS, DAB2, MYC, EPHA3 and VIPR2, and in metastatic dissemination of AREG, ZNF503, PAX8, MMP13, JAM3, and MTURN. Conversely, no meaningful difference was found in pathogenic single-nucleotide variant frequencies, reinforcing the notion that they are early events in tumorigenesis. CDKN2A homozygous deletion was linked to poor clinical outcome in patients with early tumours (overall survival hazard ratio 2.17, 95% CI: 1.43–3.28, corrected p-value = 0.01). Furthermore, we found that KRAS mutant allele specific imbalance, i.e. focal amplification of the mutant allele, is more prevalent in locoregional or distant samples of metastatic patients than in early lesions (8.4%, 13% and 2.8% respectively). This observation was replicated in three public cohorts. Tumours with KRAS mutant allele specific imbalance show specific patterns of co-occurrence and mutual exclusion with alterations in key cancer genes like CDKN2A, TP53, STK11 and NKX2-1, often in a tumour type dependent manner.
Conclusion
Advanced LUAD tumours exhibit higher copy-number alteration burden, with distinct alterations associated with tumour progression and metastasis. CDKN2A homozygous deletions predict poor prognosis in early disease, while KRAS mutant allele-specific imbalance is enriched in advanced tumours.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Chromosomal microarray raw data are available on the Sequence Read Archive under the accession number SUB15395068.
References
Cancer Genome Atlas Research Network, Campbell JD, Alexandrov A, Kim J, Wala J, Berger AH, et al. Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. Nat Genet. 2016;48:607–16.
The Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–50.
Skoulidis F, Heymach JV. Co-occurring genomic alterations in non-small-cell lung cancer biology and therapy. Nat Rev Cancer. 2019;19:495–509.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Non-Small Cell Lung Cancer [Internet]. 2022. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
Bertucci F, Ng CKY, Patsouris A, Droin N, Piscuoglio S, Carbuccia N, et al. Genomic characterization of metastatic breast cancers. Nature. 2019;569:560–4.
Nguyen B, Fong C, Luthra A, Smith SA, DiNatale RG, Nandakumar S, et al. Genomic characterization of metastatic patterns from prospective clinical sequencing of 25,000 patients. Cell. 2022185:563–575.e11.
International Agency for Research on Cancer. Cancer Incidence, Mortality and Prevalence Worldwide [Internet]. Available from: https://gco.iarc.fr
Barlesi F, Tomasini P, Karimi M, Michiels S, Raimbourg J, Daniel C, et al. Comprehensive genome profiling in patients with metastatic non–small cell lung cancer: the precision medicine phase II randomized SAFIR02-lung trial. Clin Cancer Res. 2022;28:OF1–9.
The Cancer Genome Atlas, National Health Institute. https://portal.gdc.cancer.gov/projects/TCGA-LUAD. Genomic Data Common, TCGA-LUAD project.
Jee J, Lebow ES, Yeh R, Das JP, Namakydoust A, Paik PK, et al. Overall survival with circulating tumor DNA-guided therapy in advanced non-small-cell lung cancer. Nat Med. 2022;28:2353–63.
The AACR Project GENIE Consortium, The AACR Project GENIE Consortium, André F, Arnedos M, Baras AS, Baselga J, et al. AACR Project GENIE: Powering Precision Medicine through an International Consortium. Cancer Discovery. 2017;7:818–31.
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–4.
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:pl1.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. Reporting recommendations for tumor marker prognostic studies (REMARK). JNCI J Natl Cancer Inst. 2005;97:1180–4.
The International Adjuvant Lung Cancer Trial Collaborative Group. Cisplatin-based adjuvant chemotherapy in patients with completely resected non–small-cell lung cancer. N Engl J Med. 2004;350:351–60.
Shepherd FA, Domerg C, Hainaut P, Jänne PA, Pignon JP, Graziano S, et al. Pooled analysis of the prognostic and predictive effects of KRAS mutation status and KRAS mutation subtype in early-stage resected non–small-cell lung cancer in four trials of adjuvant chemotherapy. JCO. 2013;31:2173–81.
on behalf of the LACE-Bio Consortium, Rotolo F, Zhu CQ, Brambilla E, Graziano SL, Olaussen K, et al. Genome-wide copy number analyses of samples from LACE-Bio project identify novel prognostic and predictive markers in early stage non-small cell lung cancer. Transl Lung Cancer Res. 2018;7:416–27.
McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GRS, Thormann A, et al. The ensembl variant effect predictor. Genome Biol. 2016;17:122.
oncokb-annotator [Internet]. Available from: https://github.com/oncokb/oncokb-annotator#readme
Sondka Z, Dhir NB, Carvalho-Silva D, Jupe S, Madhumita, McLaren K, et al. COSMIC: a curated database of somatic variants and clinical data for cancer. Nucleic Acids Res. 2024;52:D1210–7.
Chang MT, Bhattarai TS, Schram AM, Bielski CM, Donoghue MTA, Jonsson P, et al. Accelerating discovery of functional mutant alleles in cancer. Cancer Discov. 2018;8:174–83.
Chakravarty D, Gao J, Phillips S, Kundra R, Zhang H, Wang J, et al. OncoKB: a precision oncology knowledge base. JCO Precision Oncol. 2017:1–16.
Li MM, Datto M, Duncavage EJ, Kulkarni S, Lindeman NI, Roy S, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer. J Mol Diagnostics. 2017;19:4–23.
R Core Team. R: A language and environment for statistical computing [Internet]. Vienna, Austria; 2020. Available from: https://www.R-project.org/
Watkins TBK, Lim EL, Petkovic M, Elizalde S, Birkbak NJ, Wilson GA, et al. Pervasive chromosomal instability and karyotype order in tumour evolution. Nature. 2020;587:126–32.
Hamidi H, Ivaska J. Every step of the way: integrins in cancer progression and metastasis. Nat Rev Cancer. 2018;18:533–48.
Du L, Zhao Z, Ma X, Hsiao TH, Chen Y, Young E, et al. miR-93-directed downregulation of DAB2 defines a novel oncogenic pathway in lung cancer. Oncogene. 2014;33:4307–15.
Shahi P, Wang CY, Lawson DA, Slorach EM, Lu A, Yu Y, et al. ZNF503/Zpo2 drives aggressive breast cancer progression by down-regulation of GATA3 expression. Proc Natl Acad Sci USA. 2017;114:3169–74.
Patel SA, Hirosue S, Rodrigues P, Vojtasova E, Richardson EK, Ge J, et al. The renal lineage factor PAX8 controls oncogenic signalling in kidney cancer. Nature. 2022;606:999–1006.
Kessenbrock K, Wang CY, Werb Z. Matrix metalloproteinases in stem cell regulation and cancer. Matrix Biol. 2015;44–46:184–90.
Shih DJH, Nayyar N, Bihun I, Dagogo-Jack I, Gill CM, Aquilanti E, et al. Genomic characterization of human brain metastases identifies drivers of metastatic lung adenocarcinoma. Nat Genet. 2020;52:371–7.
Sun X, Lu B, Hu B, Xiao W, Li W, Huang Z. Novel function of the chromosome 7 open reading frame 41 gene to promote leukemic megakaryocyte differentiation by modulating TPA-induced signaling. Blood Cancer J. 2014;4:e198.
Yan FJ, Wang YJ, Wang SE, Hong HT. PKCα/ERK/C7ORF41 axis regulates epidermal keratinocyte differentiation through the IKKα nuclear translocation. Biochem J. 2021;478:839–54.
Liu L, Song X, Li X, Xue L, Ding S, Niu L, et al. A three-platelet mRNA set: MAX, MTURN and HLA-B as biomarker for lung cancer. J Cancer Res Clin Oncol. 2019;145:2713–23.
Busser B, Sancey L, Brambilla E, Coll JL, Hurbin A. The multiple roles of amphiregulin in human cancer. Biochim et Biophys Acta (BBA) Rev Cancer 2011;1816:119–31.
Williams CJM, Elliott F, Sapanara N, Aghaei F, Zhang L, Muranyi A, et al. Associations between AI-assisted tumor amphiregulin and epiregulin IHC and outcomes from anti-EGFR therapy in the routine management of metastatic colorectal cancer. Clin Cancer Res. 2023;29:4153–65.
Asano S, Yamasaka M, Ozasa K, Sakamoto K, Hayata-Takano A, Nakazawa T, et al. Vasoactive intestinal peptide–VIPR2 signaling regulates tumor cell migration. Front Oncol. 2022;12:852358.
Zhuang G, Song W, Amato K, Hwang Y, Lee K, Boothby M, et al. Effects of cancer-associated EPHA3 mutations on lung cancer. JNCI: J Natl Cancer Inst. 2012;104:1183–98.
Sosinsky A, Ambrose J, Cross W, Turnbull C, Henderson S, Jones L, et al. Insights for precision oncology from the integration of genomic and clinical data of 13,880 tumors from the 100,000 Genomes Cancer Programme. Nat Med. 2024;30:279–89.
Liu R, Rizzo S, Wang L, Chaudhary N, Maund S, Garmhausen MR, et al. Characterizing mutation-treatment effects using clinico-genomics data of 78,287 patients with 20 types of cancers. Nat Commun. 2024;15:10884.
Lou-Qian Z, Rong Y, Ming L, Xin Y, Feng J, Lin X The Prognostic Value of Epigenetic Silencing of p16 Gene in NSCLC Patients: A Systematic Review and Meta-Analysis. Pratap J, editor. PLoS ONE. 2013;8:e54970.
Yu CC, Qiu W, Juang CS, Mansukhani MM, Halmos B, Su GH. Mutant allele specific imbalance in oncogenes with copy number alterations: Occurrence, mechanisms, and potential clinical implications. Cancer Lett. 2017;384:86–93.
Burgess MR, Hwang E, Mroue R, Bielski CM, Wandler AM, Huang BJ, et al. KRAS allelic imbalance enhances fitness and modulates MAP kinase dependence in cancer. Cell. 2017;168:817–829.e15.
Kerr EM, Gaude E, Turrell FK, Frezza C, Martins CP. Mutant Kras copy number defines metabolic reprogramming and therapeutic susceptibilities. Nature. 2016;531:110–3.
Chan-Seng-Yue M, Kim JC, Wilson GW, Ng K, Figueroa EF, O’Kane GM, et al. Transcription phenotypes of pancreatic cancer are driven by genomic events during tumor evolution. Nat Genet. 2020;52:231–40.
Mueller S, Engleitner T, Maresch R, Zukowska M, Lange S, Kaltenbacher T, et al. Evolutionary routes and KRAS dosage define pancreatic cancer phenotypes. Nature. 2018;554:62–8.
Awad MM, Liu S, Rybkin II, Arbour KC, Dilly J, Zhu VW, et al. Acquired resistance to KRAS G12C inhibition in cancer. N Engl J Med. 2021;384:2382–93.
Skoulidis F, Byers LA, Diao L, Papadimitrakopoulou VA, Tong P, Izzo J, et al. Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer Discov. 2015;5:860–77.
Sasaki H, Hikosaka Y, Kawano O, Moriyama S, Yano M, Fujii Y. Evaluation of Kras gene mutation and copy number gain in non-small cell lung cancer. J Thorac Oncol. 2011;6:15–20.
Chiosea SI, Sherer CK, Jelic T, Dacic S. KRAS mutant allele-specific imbalance in lung adenocarcinoma. Mod Pathol. 2011;24:1571–7.
Author information
Authors and Affiliations
Contributions
Benjamin Besse, Maud Kamal, Fabrice Barlesi and Ivan Bièche conceived the study and participated in its design. Benjamin Besse, Ivan Bièche and Marta Jimenez acquired the financial support for the project. David Planchard, Marta Jimenez, Christophe Le Tourneau, Nicolas Girard, Benjamin Besse and Fabrice Barlesi provided patient samples and gathered and curated clinical data. Ludovic Lacroix, Valery Attignon, Isabelle Soubeyran, Pascal JézéquelIvan Bièche provided laboratory reagents and instrumentation. Sophie Vacher performed sequencing experiments. Abderaouf Hamza, Alicia Tran-Dien, Laurène Syx and Pierre Gestraud performed and Nicolas Servant performed the bioinformatic analysis. Maryam Karimi, Stefan Michiels, and Trenton Dailey-Chwalibóg performed statistical analyses. Abderaouf Hamza, Samia Melaabi, Quentin Peretti, Isabelle Soubeyran, Ludovic Lacroix and Valeri Attignon analysed the data, created the visualisations and wrote the original drafts. Ivan Bièche reviewed the original drafts. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
F Barlesi reports personal fees from AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer-Ingelheim, Eli Lilly Oncology, F Hoffmann-La Roche Ltd, Novartis, Merck, Mirati, MSD, Pierre Fabre, Pfizer, Seattle Genetics and Takeda; grants from Abbvie, ACEA, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer-Ingelheim, Eisai, Eli Lilly Oncology, F Hoffmann-La Roche Ltd., Genentech, Ipsen, Ignyta, Innate Pharma, Loxo, Novartis, Medimmune, Merck, MSD, Pierre Fabre, Pfizer, Sanofi-Aventis, and Takeda; and nonfinancial support from AstraZeneca, BMS, Merck, Pierre Fabre, and F Hoffmann-La Roche outside the submitted work. S. Michiels reports personal fees from Amaris, Roche, Sensorion, Biophytis, Servier, and Yuhan outside the submitted work. A Madroszyk reports personal fees and nonfinancial support from AstraZeneca and Roche, and nonfinancial support from Lilly outside the submitted work. I Soubeyran reports grants and nonfinancial support from AstraZeneca; grants from Takeda and ThermoFisher; and personal fees from GSK, Lilly, and Servier outside the submitted work. M. Jimenez reports grants and nonfinancial support from AstraZeneca and grants from Fondation ARC during the conduct of the study. B. Besse reports grants from 4D Pharma, AbbVie, Amgen, Aptitude Health, AstraZeneca, BeiGene, Blueprint Medicines, Boehringer Ingelheim, Celgene, Cergentis, Chugai pharmaceutical, Cristal Therapeutics, Daiichi-Sankyo, Eli Lilly, EISAI, Genzyme Corporation, GSK, Inivata, IPSEN, Janssen, Onxeo, OSE immunotherapeutics, Pfizer, Roche-Genentech, Sanofi, Takeda, Tolero Pharmaceuticals, and Turning Point Therapeutics during the conduct of the study. No disclosures were reported by the other authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hamza, A., Gestraud, P., Karimi, M. et al. Molecular analysis of lung adenocarcinomas from the SAFIR02-Lung cohort reveals new metastasis-associated copy-number alterations including frequent mutant-specific KRAS-allelic imbalance and identifies CDKN2A homozygous deletions as an independent biomarker of poor prognosis. Br J Cancer 133, 1554–1564 (2025). https://doi.org/10.1038/s41416-025-03183-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03183-2