Abstract
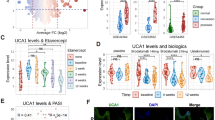
Psoriasis is a persistent inflammatory skin disease characterized by the adverse infiltration of inflammatory cells and epidermal hyperplasia. Self-RNA is the most abundant damage-associated molecular pattern (DAMP) in psoriasis tissues, which triggers and amplifies inflammatory responses through TLR7 pathway. However, the pathogenic effects of self-RNA on immune cell activation and chemotaxis during psoriasis and the underlying mechanisms remain largely unknown. Epigenetic modifications are widely acknowledged to link the environmental signals to gene expression in various immune cells, whose dysfunction tends to cause or worsen various inflammatory diseases. Through a comprehensive analysis of histone modifications in lesional skin from both psoriasis patients and mice, the significantly increased level of histone acetylation at H4 lysine 16 (H4K16ac) in macrophages was found, which was positively correlated with the accumulation of self-RNA in the dermis and psoriasis pathology. Further studies showed that lysine acetyltransferase 8 (KAT8) was responsible for self-RNA-driven H4K16ac modification and psoriasis-associated pathogenic chemokine expression in macrophages of lesional skin. Mechanistically, KAT8 was selectively recruited to the gene promoters of pathogenic chemokines including Cxcl2 and Ccl3 through interaction with AP-1 transcription complex. The auto-acetylation of KAT8 enhanced its acetyltransferase activity. KAT8-mediated H4K16ac modification at these chemokine promoters, coupling with increased chromatin accessibility, facilitated the production and secretion of pro-inflammatory chemokines CXCL2 and CCL3 for neutrophil chemotaxis, neutrophil extracellular traps (NETs) formation and aggravated inflammatory damage in psoriasis. KAT8 deficiency in macrophages or pharmacological inhibition restricted the secretion of macrophage-derived pro-inflammatory chemokines and ameliorated TLR7-dependent tissue inflammatory injury in experimental psoriasis and arthritis model. Taken together, our finding provides new insight into the role of epigenetic modification in self-RNA/TLR7 pathway-dependent immune cell activation and chemotaxis during psoriasis, which proposes the promising therapeutic strategy to control the inflammatory damage and psoriatic skin dysfunction by targeting KAT8 and KAT8-mediated H4K16ac modification in dermis macrophages.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Data supporting the present study are available from the corresponding author upon reasonable request. Original images of unprocessed immunoblot are available at Supplementary information.
References
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet. 2021;397:1301–15.
Cai Y, Shen X, Ding C, Qi C, Li K, Li X, et al. Pivotal role of dermal IL-17-producing γδ T cells in skin inflammation. Immunity. 2011;35:596–610.
Lowes MA, Bowcock AM, Krueger JG. Pathogenesis and therapy of psoriasis. Nature. 2007;445:866–73.
Lou F, Sun Y, Xu Z, Niu L, Wang Z, Deng S, et al. Excessive polyamine generation in keratinocytes promotes self-RNA sensing by dendritic cells in psoriasis. Immunity. 2020;53:204–16.e10.
Brunner PM, Koszik F, Reininger B, Kalb ML, Bauer W, Stingl G. Infliximab induces downregulation of the IL-12/IL-23 axis in 6-sulfo-LacNac (slan)+ dendritic cells and macrophages. J Allergy Clin Immunol. 2013;132:1184–93.e8.
Zhang L-J, Sen GL, Ward NL, Johnston A, Chun K, Chen Y, et al. Antimicrobial peptide LL37 and MAVS signaling drive interferon-β production by epidermal keratinocytes during skin injury. Immunity. 2016;45:119–30.
Ganguly D, Chamilos G, Lande R, Gregorio J, Meller S, Facchinetti V, et al. Self-RNA–antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. J Exp Med. 2009;206:12.
Tokuyama M, Mabuchi T. New treatment addressing the pathogenesis of psoriasis. International J Mol Sci. 2020;21:7488.
Romhányi D, Szabó K, Kemény L, Groma G. Histone and histone acetylation-related alterations of gene expression in uninvolved psoriatic skin and their effects on cell proliferation, differentiation, and immune responses. Int J Mol Sci. 2023;24:14551.
Yao Q, Epstein CB, Banskota S, Issner R, Kim Y, Bernstein BE, et al. Epigenetic alterations in keratinocyte carcinoma. J Invest Dermatol. 2021;141:1207–18.
Masalha M. H3K27Ac modification and gene expression in psoriasis. J Dermatol Sci. 2021;103:93–100.
Nascimento-Filho CHV, Silveira EJD, Goloni-Bertollo EM, De Souza LB, Squarize CH, Castilho RM. Skin wound healing triggers epigenetic modifications of histone H4. J Transl Med. 2020;18:138.
Greb JE, Goldminz AM, Elder JT, Lebwohl MG, Gladman DD, Wu JJ, et al. Psoriasis. Nat Rev Dis Prim. 2016;2:16082.
Valerio DG, Xu H, Eisold ME, Woolthuis CM, Pandita TK, Armstrong SA. Histone acetyltransferase activity of MOF is required for adult but not early fetal hematopoiesis in mice. Blood. 2017;129:48–59.
Mellert H, Sykes SM, Murphy ME, McMahon SB. The ARF/oncogene pathway activates p53 acetylation within the DNA binding domain. Cell Cycle (Georget, Tex). 2007;6:1304–6.
Füllgrabe J, Klionsky DJ, Joseph B. Histone post-translational modifications regulate autophagy flux and outcome. Autophagy. 2013;9:1621–3.
Wu Y. Disrupting the phase separation of KAT8–IRF1 diminishes PD-L1 expression and promotes antitumor immunity. Nature Cancer. 2023;4:382–400.
Huai W, Liu X, Wang C, Zhang Y, Chen X, Chen X, et al. KAT8 selectively inhibits antiviral immunity by acetylating IRF3. J Exp Med. 2019;216:772–85.
Herster F. Neutrophil extracellular trap-associated RNA and LL37 enable self-amplifying inflammation in psoriasis. Nat Commun. 2020;11:105.
Balsini P, Weinzettl P, Samardzic D, Zila N, Buchberger M, Freystätter C et al. Stiffness-dependent lysyl oxidase regulation through hypoxia-inducing factor 1 drives extracellular matrix modifications in psoriasis. J Invest Dermatol. 2024; 26:1653–69.
Suárez-Fariñas M, Li K, Fuentes-Duculan J, Hayden K, Brodmerkel C, Krueger JG. Expanding the psoriasis disease profile: interrogation of the skin and serum of patients with moderate-to-severe psoriasis. J Invest Dermatol. 2012;132:2552–64.
Peng L, Liu W, Cheng Y, Chen L, Shen Z. IL-17A/F double producing T cells, unstable tregs and quiescent TRMs in clinically healed lesions are potential cellular candidates for recurrence of psoriasis. Clin Immunol. 2024;266:110328.
Gessl I, Hana CA, Deimel T, Durechova M, Hucke M, Konzett V, et al. Tenderness and radiographic progression in rheumatoid arthritis and psoriatic arthritis. Ann Rheum Dis. 2023;82:344–50.
El Bably MM, Abdel Aziz DM, Adly NN, Ali MA, Khedr AS, El Leithy SA. Galectin-1 in Psoriatic arthritis, Psoriasis, Rheumatoid arthritis and its relation with disease activity and skin lesion. Egypt J Immunol. 2023;30:73–82.
Chamberlain ND, Kim S, Vila OM, Volin MV, Volkov S, Pope RM, et al. Ligation of TLR7 by rheumatoid arthritis synovial fluid single strand RNA induces transcription of TNFα in monocytes.Ann Rheum Dis. 2013;72:418–26.
Heil F, Hemmi H, Hochrein H, Ampenberger F, Kirschning C, Akira S, et al. Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science. 2004;303:1526–29.
Füllgrabe J, Lynch-Day MA, Heldring N, Li W, Struijk RB, Ma Q, et al. The histone H4 lysine 16 acetyltransferase hMOF regulates the outcome of autophagy. Nature. 2013;500:468–71.
Zhu Y, Wu Z, Yan W, Shao F, Ke B, Jiang X, et al. Allosteric inhibition of SHP2 uncovers aberrant TLR7 trafficking in aggravating psoriasis. EMBO Mol Med. 2022;14:e14455.
Yang Y, Csakai A, Jiang S, Smith C, Tanji H, Huang J, et al. Tetrasubstituted imidazoles as incognito Toll-like receptor 8 a(nta)gonists. Nat Commun. 2021;12:4351.
Klopp-Schulze L, Shaw JV, Dong JQ, Khandelwal A, Vazquez-Mateo C, Goteti K. Applying modeling and simulations for rational dose selection of novel toll-like receptor 7/8 inhibitor enpatoran for indications of high medical need. Clin Pharm Ther. 2022;112:297–306.
McKinnon JE, Santiaguel J, Murta de Oliveira C, Yu D, Khursheed M, Moreau F, et al. Enpatoran in COVID-19 pneumonia: safety and efficacy results from a phase II randomized trial. Clin Transl Sci. 2023;16:2640–53.
Port A, Shaw JV, Klopp-Schulze L, Bytyqi A, Vetter C, Hussey E, et al. Phase 1 study in healthy participants of the safety, pharmacokinetics, and pharmacodynamics of enpatoran (M5049), a dual antagonist of toll-like receptors 7 and 8. Pharmacol Res Perspect. 2021;9:e00842.
Zhang P, Su Y, Zhao M, Huang W, Lu Q. Abnormal histone modifications in PBMCs from patients with psoriasis vulgaris. Eur J Dermatol. 2011;21:552–7.
Samata M, Alexiadis A, Richard G, Georgiev P, Nuebler J, Kulkarni T, et al. Intergenerationally maintained histone h4 lysine 16 acetylation is instructive for future gene activation. Cell. 2020;182:127–44.
Pessoa Rodrigues C, Chatterjee A, Wiese M, Stehle T, Szymanski W, Shvedunova M, et al. Histone H4 lysine 16 acetylation controls central carbon metabolism and diet-induced obesity in mice. Nat Commun. 2021;12:6212.
Zhang X, Liu H, Zhou JQ, Krick S, Barnes JW, Thannickal VJ, et al. Modulation of H4K16Ac levels reduces pro-fibrotic gene expression and mitigates lung fibrosis in aged mice. Theranostics. 2022;12:530–41.
Chen F, Chen H, Jia Y, Lu H, Tan Q, Zhou X. miR-149-5p inhibition reduces alzheimer’s disease β-amyloid generation in 293/APPsw cells by upregulating H4K16ac via KAT8. Exp Ther Med. 2020;20:88.
Zippo A, Serafini R, Rocchigiani M, Pennacchini S, Krepelova A, Oliviero S. Histone crosstalk between H3S10ph and H4K16ac generates a histone code that mediates transcription elongation. Cell. 2009;138:1122–36.
Cai W-T, Guan P, Lin M-X, Fu B, Wu B. Sirt1 suppresses MCP-1 production during the intervertebral disc degeneration by inactivating AP-1 subunits c-fos/c-jun. Eur Rev Med Pharm Sci. 2020;24:5895–904.
Novoszel P, Holcmann M, Stulnig G, De Sa Fernandes C, Zyulina V, Borek I, et al. Psoriatic skin inflammation is promoted by c-Jun/AP-1-dependent CCL2 and IL-23 expression in dendritic cells. EMBO Mol Med. 2021;13:e12409.
Bhagchandani S, Johnson JA, Irvine DJ. Evolution of Toll-like receptor 7/8 agonist therapeutics and their delivery approaches: from antiviral formulations to vaccine adjuvants. Advanced Drug Deliv Rev. 2021;175:113803.
Kaisho T, Tanaka T. Turning NF-kappaB and IRFs on and off in DC. Trends Immunol. 2008;29:329–36.
Larsen SB, Cowley CJ, Sajjath SM, Barrows D, Yang Y, Carroll TS, et al. Establishment, maintenance, and recall of inflammatory memory. Cell Stem Cell. 2021;28:1758–74.
Sheikh BN, Guhathakurta S, Akhtar A. The non-specific lethal (NSL) complex at the crossroads of transcriptional control and cellular homeostasis. EMBO Rep. 2019;20:e47630.
Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20:1475.
Van Der Fits L, Mourits S, Voerman JSA, Kant M, Boon L, Laman JD, et al. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J Immunol. 2009;182:5836–45.
Zhang S, Zhang Y, Duan X, Wang B, Zhan Z. Targeting NPM1 epigenetically promotes postinfarction cardiac repair by reprogramming reparative macrophage metabolism. Circulation. 2024;149:1982–2001.
Zhang Y, Gao Y, Jiang Y, Ding Y, Chen H, Xiang Y, et al. Histone demethylase KDM5B licenses macrophage-mediated inflammatory responses by repressing Nfkbia transcription. Cell Death Differ. 2023;30:1279–92.
Zhou Q, Zhang Y, Wang B, Zhou W, Bi Y, Huai W, et al. KDM2B promotes IL-6 production and inflammatory responses through Brg1-mediated chromatin remodeling. Cell Mol Immunol. 2020;17:834–42.
Yong L, Yu Y, Li B, Ge H, Zhen Q, Mao Y, et al. Calcium/calmodulin-dependent protein kinase IV promotes imiquimod-induced psoriatic inflammation via macrophages and keratinocytes in mice. Nat Commun. 2022;13:4255.
Funding
This work was supported by the National Key Research & Development Program of China (2023YFC2307302, 2023YFC2307000), the Noncommunicable Chronic Diseases-National Science and Technology Major Project (2024ZD0529003), the National Natural Science Foundation of China (82271797, 82341065, 82371825 and 32400727), the program of Shanghai outstanding academic leader in public health subject (GWVI-11.2-XD29), the experimental animal program sponsored by the Science and Technology Commission of Shanghai Municipality (23141902300), the Natural Science Foundation of Shanghai (24ZR1481100), the Chenguang Program of Shanghai Education Development Foundation and Shanghai Municipal Education Commission (24CGA43), the Postadoctoral Fellowship Program for Innovative Talents and China Postdoctoral Science Foundation, and the Open Research Fund of Basic Medicine College of Naval Medical University (JCKFKT-ZD-002).
Author information
Authors and Affiliations
Contributions
YX, YJ, ZW, and XW performed experiments, analyzed data, and interpreted results. YX designed experiments and drafted the manuscript. LM, YD, BR, CZ, and XL performed experiments and collected data. MX provided the resources; XL, ZZ, and YZ conceived the study, designed experiments, analyzed data, revised the manuscript, and provided funding for this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All animal experiments were conducted in strict accordance with the Guidelines for the Care and Use of Laboratory Animals of Naval Medical University, China, and approved by the Animal Ethics Committee of Naval Medical University. Informed consents were obtained from all participants. Experiments using human samples were approved by the Ethics Committee of Skin Disease Hospital of Tongji University, and conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiang, Y., Jiang, Y., Wang, Z. et al. Targeting KAT8 alleviates self-RNA-driven skin inflammation by modulating histone H4 lysine 16 acetylation in psoriasis. Cell Death Differ (2025). https://doi.org/10.1038/s41418-025-01547-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41418-025-01547-y