Abstract
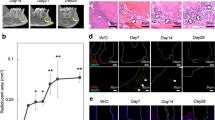
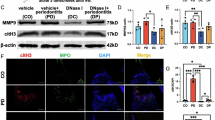
Periodontitis is a prevalent and progressive detrimental disease characterized by chronic inflammation, and the immunopathological mechanisms are not yet fully understood. Mesenchymal stem cells (MSCs) play crucial roles as immunoregulators and maintain tissue homeostasis and regeneration, but their in vivo function in immunopathology and periodontal tissue deterioration is still unclear. Here, we utilized multiple transgenic mouse models to specifically mark, ablate and modulate Gli1+ cells, a critical and representative subset of MSCs in the periodontium, to explore their specific role in periodontal immunopathology. We revealed that Gli1+ cells, upon challenge with an inflammatory microenvironment, significantly induce rapid trafficking and aberrant activation of neutrophils, thus exacerbating alveolar bone destruction. Mechanistically, extracellular vesicles (EVs) released by Gli1+ cells act as crucial immune regulators in periodontal tissue, mediating the recruitment and activation of neutrophils through increased neutrophil generation of reactive oxygen species and stimulation of nuclear factor kappa-B signaling. Furthermore, we discovered that CXC motif chemokine ligand 1 (CXCL1) is exposed on the surface of EVs derived from inflammation-challenged Gli1+ cells to prime aberrant neutrophils via the CXCL1-CXC motif chemokine receptor 2 (CXCR2) axis. Importantly, specific inhibition of EV release from Gli1+ cells or pharmacological therapy with GANT61 ameliorates periodontal inflammation and alveolar bone loss. Collectively, our findings identify previously unrecognized roles of Gli1+ cells in orchestrating infiltration and promoting aberrant activation of neutrophils under inflammation, which provides pathological insights and potential therapeutic targets for periodontitis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Chen MX, Zhong YJ, Dong QQ, Wong HM, Wen YF. Global, regional, and national burden of severe periodontitis, 1990–2019: An analysis of the Global Burden of Disease Study 2019. J Clin Periodontol 2021;48:1165–88.
Seymour GJ, Ford PJ, Cullinan MP, Leishman S, Yamazaki K. Relationship between periodontal infections and systemic disease. Clin Microbiol Infect 2007;4:3–10.
Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease: Inflammatory and immune pathways in periodontal disease. Periodontol. 2000;64:57–80.
Tsukasaki M, Komatsu N, Nagashima K, Nitta T, Pluemsakunthai W, Shukunami C, et al. Host defense against oral microbiota by bone-damaging T cells. Nat Commun 2018;9:701.
Araujo-Pires AC, Vieira AE, Francisconi CF, Biguetti CC, Glowacki A, Yoshizawa S, et al. IL-4/CCL22/CCR4 axis controls regulatory T-cell migration that suppresses inflammatory bone loss in murine experimental periodontitis. J Bone Miner Res 2015;30:412–22.
Mahanonda R, Champaiboon C, Subbalekha K, Sa-Ard-Iam N, Rattanathammatada W, Thawanaphong S, et al. Human memory B cells in healthy gingiva, gingivitis, and periodontitis. J Immunol 2016;197:715–25.
Xiao L, Zhou Y, Zhu L, Yang S, Huang R, Shi W, et al. SPHK1-S1PR1-RANKL Axis regulates the interactions between macrophages and BMSCs in inflammatory bone loss. J Bone Miner Res 2018;33:1090–104.
Kim TS, Silva LM, Theofilou VI, Greenwell-Wild T, Li L, Williams DW, et al. Neutrophil extracellular traps and extracellular histones potentiate IL-17 inflammation in periodontitis. J Exp Med 2023;220:e20221751.
Zhang D, Lin W, Jiang S, Deng P, Liu L, Wang Q, et al. Lepr‐Expressing PDLSCs Contribute to Periodontal Homeostasis and Respond to Mechanical Force by Piezo1. Adv Sci 2023;10:2303291.
Chen S, Jing J, Yuan Y, Feng J, Han X, Wen Q, et al. Runx2+ Niche cells maintain incisor mesenchymal tissue homeostasis through IGF Signaling. Cell Rep. 2020;32:108007.
Men Y, Wang Y, Yi Y, Jing D, Luo W, Shen B, et al. Gli1+ Periodontium stem cells are regulated by osteocytes and occlusal force. Dev Cell 2020;54:639–.e6.
Liu J, Gao J, Liang Z, Gao C, Niu Q, Wu F, et al. Mesenchymal stem cells and their microenvironment. Stem Cell Res Ther 2022;13:429.
Zhou J, Shi Y. Mesenchymal stem/stromal cells (MSCs): origin, immune regulation, and clinical applications. Cell Mol Immunol 2023;20:555–7.
Peng J, Han L, Liu B, Song J, Wang Y, Wang K, et al. Gli1 marks a sentinel muscle stem cell population for muscle regeneration. Nat Commun 2023;14:6993.
Lehmann GL, Hanke-Gogokhia C, Hu Y, Bareja R, Salfati Z, Ginsberg M, et al. Single-cell profiling reveals an endothelium-mediated immunomodulatory pathway in the eye choroid. J Exp Med 2020;217:e20190730.
Zhao H, Feng J, Ho TV, Grimes W, Urata M, Chai Y. The suture provides a niche for mesenchymal stem cells of craniofacial bones. Nat Cell Biol 2015;17:386–96.
Zhao H, Feng J, Seidel K, Shi S, Klein O, Sharpe P, et al. Secretion of shh by a neurovascular bundle niche supports mesenchymal stem cell homeostasis in the adult mouse incisor. Cell Stem Cell 2014;14:160–73.
Degirmenci B, Valenta T, Dimitrieva S, Hausmann G, Basler K. GLI1-expressing mesenchymal cells form the essential Wnt-secreting niche for colon stem cells. Nature 2018;558:449–53.
Shalehin N, Seki Y, Takebe H, Fujii S, Mizoguchi T, Nakamura H, et al. Gli1 + -PDL Cells Contribute to alveolar bone homeostasis and regeneration. J Dent Res 2022;101:1537–43.
Liu AQ, Zhang LS, Chen J, Sui BD, Liu J, Zhai QM, et al. Mechanosensing by Gli1+ cells contributes to the orthodontic force-induced bone remodeling. Cell Prolif 2020;53:e12810.
Huang X, Sui B, Liu A, Guo H, Zheng C, Liu P, et al. Odontogenesis-empowered extracellular vesicles safeguard donor-recipient stem cell interplay to support tooth regeneration. Small 2024;20:e240026.
Deng Y, Li Q, Svoboda KKH, Opperman LA, Ruest LB, Liu X. Gli1 + Periodontal mesenchymal stem cells in periodontitis. J Dent Res 2024;103:279–88.
van Niel G, Carter DRF, Clayton A, Lambert DW, Raposo G, Vader P. Challenges and directions in studying cell‒cell communication by extracellular vesicles. Nat Rev Mol Cell Biol 2022;23:369–82.
Marchesan J, Girnary MS, Jing L, Miao MZ, Zhang S, Sun L, et al. An experimental murine model to study periodontitis. Nat Protoc 2018;13:2247–67.
Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 2013;13:159–75.
Kou M, Huang L, Yang J, Chiang Z, Chen S, Liu J, et al. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? Cell Death Dis 2022;13:580.
Ueda Y, Nakazawa D, Nishio S, Shiratori-Aso S, Kudo T, Miyoshi-Harashima A, et al. Transcription factor Nrf2 activation regulates NETosis, endothelial injury, and kidney disease in myeloperoxidase-positive antineutrophil cytoplasmic antibody-associated vasculitis. Kidney Int 2024;105:1291–305.
Crompton ME, Gaessler LF, Tawiah PO, Polzer L, Camfield SK, Jacobson GD, et al. Expression of RcrB confers resistance to hypochlorous acid in uropathogenic Escherichia coli. J Bacteriol 2023;205:e0006423.
Kwaku GN, Ward RA, Vyas JM, Harding HB. Host innate immune systems gather intel on invading microbes via pathogen-derived extracellular vesicles. Extracell Vesicle 2024;3:100043.
Ding Z, Greenberg ZF, Serafim MF, Ali S, Jamieson JC, Traktuev DO, et al. Understanding molecular characteristics of extracellular vesicles derived from different types of mesenchymal stem cells for therapeutic translation. Extracell Vesicle 2024;3:100034.
Liu L, Zheng C, Zhao N, Zhu T, Hu C, Zhang N, et al. Mesenchymal stem cell aggregation‐released extracellular vesicles induce CD31 + EMCN + Vessels in skin regeneration and improve diabetic wound healing. Adv Healthc Mater 2023;12:2300019.
Williams DW, Greenwell-Wild T, Brenchley L, Dutzan N, Overmiller A, Sawaya AP, et al. Human oral mucosa cell atlas reveals a stromal-neutrophil axis regulating tissue immunity. Cell 2021;184:4090–.e15.
Metzemaekers M, Gouwy M, Proost P. Neutrophil chemoattractant receptors in health and disease: double-edged swords. Cell Mol Immunol 2020;17:433–50.
Su D, Jiao Z, Li S, Yue L, Li C, Deng M, et al. Spatiotemporal single-cell transcriptomic profiling reveals inflammatory cell states in a mouse model of diffuse alveolar damage. Exploration 2023;3:20220171.
Chen Y, Wang H, Yang Q, Zhao W, Chen Y, Ni Q, et al. Single-cell RNA landscape of the osteoimmunology microenvironment in periodontitis. Theranostics 2022;12:1074–96.
Silva LM, Doyle AD, Greenwell-Wild T, Dutzan N, Tran CL, Abusleme L, et al. Fibrin is a critical regulator of neutrophil effector function at the oral mucosal barrier. Science 2021;374:eabl5450.
Jing Z, Feng X, Li X, Zhang X, Pan C. Vaspin facilitates the proliferation and osteogenic differentiation of periodontal ligament stem cells. J Periodontal Res 2024;59:812–20.
Yang J, Su J, Sun Z, Song Y, Zhang Y, Zhang Z, et al. Youthful small extracellular vesicles restore the function and reparative capacity of inflammatory-impaired periodontal ligament stem cells by delivering protein biglycan for bone regeneration. J Nanobiotechnol 2024;22:508.
He HP, Zhao MZ, Jiao WH, Liu ZQ, Zeng XH, Li QL, et al. Nocardamine mitigates cellular dysfunction induced by oxidative stress in periodontal ligament stem cells. Stem Cell Res Ther 2024;15:247.
Hajishengallis G, Chavakis T, Lambris JD. Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontol 2000 2020;84:14–34.
Cortés-Vieyra R, Rosales C, Uribe-Querol E. Neutrophil functions in periodontal homeostasis. J Immunol Res 2016;2016:1396106.
Av C, Ma S, Ca M, M G. The Role of NrF2 in the regulation of periodontal health and disease. J Dent Res 2017;96:975–83.
Liu A, Zhang L, Chen J, Sui B, Liu J, Zhai Q, et al. Mechanosensing by Gli1 + cells contributes to the orthodontic force‐induced bone remodeling. Cell Prolif 2020;53:e12810.
Deng Y, Li Q, Svoboda KKH, Opperman LA, Ruest LB, Liu X. Gli1+ Periodontal mesenchymal stem cells in periodontitis. J Dent Res 2024;103:279–88.
Shi Y, Wang Y, Li Q, Liu K, Hou J, Shao C, et al. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat Rev Nephrol 2018;14:493–507.
Li P, Ou Q, Shi S, Shao C. Immunomodulatory properties of mesenchymal stem cells/dental stem cells and their therapeutic applications. Cell Mol Immunol 2023;20:558–69.
Liu H, Zhang X, Zhang M, Zhang S, Li J, Zhang Y, et al. Mesenchymal stem cell derived exosomes repair uterine injury by targeting transforming growth factor-β signaling. ACS Nano 2024;18:3509–19.
Liu M, Hu S, Yan N, Popowski KD, Cheng K. Inhalable extracellular vesicle delivery of IL-12 mRNA to treat lung cancer and promote systemic immunity. Nat Nanotechnol 2024;19:565–75.
Dai H, Fan Q, Wang C. Recent applications of immunomodulatory biomaterials for disease immunotherapy. Exploration 2022;2:20210157.
Liu X, Hu L, Liu F. Mesenchymal stem cell-derived extracellular vesicles for cell-free therapy of ocular diseases. Extracell Vesicles Circ Nucl Acids 2022;3:102–17.
Zhang X, Che X, Zhang S, Wang R, Li M, Jin Y, et al. Mesenchymal stem cell-derived extracellular vesicles for human diseases. Extracell Vesicles Circ Nucl Acids 2024;5:64–82.
Ruan H, Li Y, Zheng D, Deng L, Chen G, Zhang X, et al. Engineered extracellular vesicles for ischemic stroke treatment. Innovation 2023;4:100394.
Yoon DS, Lee KM, Choi Y, Ko EA, Lee NH, Cho S, et al. TLR4 downregulation by the RNA-binding protein PUM1 alleviates cellular aging and osteoarthritis. Cell Death Differ 2022;29:1364–78.
Tang M, Wang G, Li J, Wang Y, Peng C, Chang X, et al. Flavonoid extract from propolis alleviates periodontitis by boosting periodontium regeneration and inflammation resolution by regulating TLR4/MyD88/NF-κB and RANK/NF-κB pathway. J Ethnopharmacol 2024;319:117324.
Liu BW, Cao JL, Wang Y, Zhao X, Zeng Q, Liu WP, et al. GANT61, an inhibitor of Gli1, inhibits the proliferation and migration of hepatocellular carcinoma cells. J Investig Med 2024;72:181–92.
Liu M, Wang X, Zhu J. PDLIM3 knockdown promotes ferroptosis in endometriosis progression by inducing Gli1 degradation and blocking Hedgehog signaling pathway. J Assist Reprod Genet 2024;41:2117–28.
Chen N, Sui BD, Hu CH, Cao J, Zheng CX, Hou R, et al. microRNA-21 Contributes to Orthodontic Tooth Movement. J Dent Res 2016;95:1425–33.
Hu CH, Sui BD, Du FY, Shuai Y, Zheng CX, Zhao P, et al. miR-21 deficiency inhibits osteoclast function and prevents bone loss in mice. Sci Rep. 2017;7:43191.
Sun S, Ma S, Cai Y, Wang S, Ren J, Yang Y, et al. A single-cell transcriptomic atlas of exercise-induced anti-inflammatory and geroprotective effects across the body. Innovation 2023;4:100380.
Zheng C, Sui B, Zhang X, Hu J, Chen J, Liu J, et al. Apoptotic vesicles restore liver macrophage homeostasis to counteract type 2 diabetes. J Extracell Vesicles 2021;10:e12109.
Acknowledgements
This work was supported by grants from the National Key Research and Development Program of China (2022YFA1104400), the National Natural Science Foundation of China (82401201, 82370949, 82371020, 82100969, and 82100992), the Young Science and Technology Rising Star Project of Shaanxi Province (2024ZC-KJXX-122), the China Postdoctoral Science Foundation (BX20230485), the “Rapid Response” Research Projects (2023KXKT017 and 2023KXKT090), and the Shaanxi Provincial Health Research and Innovation Platform Construction Plan (2024PT-04).
Author information
Authors and Affiliations
Contributions
X.Y.C., C.X.Z. and H.G. contributed equally to the experiments, data collection and analysis, and manuscript drafting. S.Y.F., X.Y.H., and J.C. contributed to the experimental performance and data collection. J.X.L., Y.R.G., A.Q.L., J.N.L. and X.H.Z. contributed to data acquisition and analysis. C.M., H.W., F.F., P.P. and H.K.X. contributed to the data analysis and interpretation. B.D.S., K.X. and Y.J. contributed to the project conception, experimental design and supervision. All the authors have read and approved the current version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cai, XY., Zheng, CX., Guo, H. et al. Inflammation-triggered Gli1+ stem cells engage with extracellular vesicles to prime aberrant neutrophils to exacerbate periodontal immunopathology. Cell Mol Immunol 22, 371–389 (2025). https://doi.org/10.1038/s41423-025-01271-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41423-025-01271-0
Keywords
This article is cited by
-
The research progress on periodontitis by the National Natural Science Foundation of China
International Journal of Oral Science (2025)