Abstract
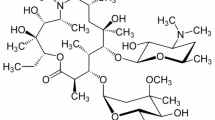
To overcome serious methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa infections, we synthesized TS2037, 5,4″-diepi-arbekacin, a novel aminoglycoside antibiotic, and evaluated its biological properties. TS2037 showed broad-range, as well as robust antibacterial activities against Gram-positive and Gram-negative bacteria. The MIC50 and MIC90 of TS2037 against clinical isolates of MRSA (n = 54) were both 0.25 µg/mL, and no resistant strain was observed. The MIC50 and MIC90 of TS2037 against clinical isolates of P. aeruginosa (n = 54) were 1 and 4 µg/mL, respectively. TS2037 and arbekacin, anti-MRSA aminoglycoside, were more stable against AAC(6′)-APH(2″), aminoglycoside-6′-N-acetyltransferase and 2″-O-phosphotransferase, produced by resistant S. aureus than gentamicin. Therapeutic efficacies of TS2037 in the mouse models of systemic infection with MRSA were superior to those of arbekacin, vancomycin, and linezolid. The efficacy of TS2037 against systemic infection caused by P. aeruginosa producing AAC(6′)-II was superior to those of arbekacin and amikacin. In the nephrotoxicity risk screening, the release of free N-acetyl-β-d-glucosaminidase from the kidney epithelial cell line after treatment with TS2037 at 2.5 and 5.0 μM were 2.0 and 2.1 (U/L), respectively, which were about two times higher than those of arbekacin. In conclusion, TS2037 exhibited the most potent antibacterial activity among aminoglycosides tested against both MRSA and P. aeruginosa in vitro and in vivo, although its nephrotoxicity risk remains to be improved.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tokajian S. New epidemiology of Staphylococcus aureus infections in the Middle East. Clin Microbiol Infect. 2014;20:624–8.
Chen CJ, Huang YC. New epidemiology of Staphylococcus aureus infection in Asia. Clin Microbiol Infect. 2014;20:605–23.
Sharma Y, Jain S, Singh H, Govil V. Staphylococcus aureus: Screening for nasal carriers in a community setting with special reference to MRSA. Science. 2014;2014:479048.
Coombs GW, Monecke S, Pearson JC, Tan HL, Chew YK, et al. Evolution and diversity of community-associated methicillin-resistant Staphylococcus aureus in a geographical region. BMC Microbiol. 2011;11:215.
Cocchi P, Taccetti G, Montagnani C, Campana S, Galli L, et al. Evidence of transmission of a Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus clone: a family affair. Clin Microbiol Infect. 2013;19:1158–62.
Shetty V, Trumbull K, Hegde A, Shenoy V, Prabhu R, et al. Prevalence of community-acquired methicillin-resistant Staphylococcus aureus nasal colonization among children. J Clin Diagn Res. 2014;8:DC12–5.
Lo WT, Lin WJ, Tseng MH, Lu JJ, Lee SY, et al. Nasal carriage of a single clone of community-acquired methicillin-resistant Staphylococcus aureus among kindergarten attendees in Northern Taiwan. BMC Infect Dis. 2007;7:51.
Ali Z, Mumtaz N, Naz SA, Jabeen N, Shafique M. Multi-drug resistant Pseudomonas aeruginosa: a threat of nosocomial infections in tertiary care hospitals. J Pak Med Assoc. 2015;65:12–6.
Rodrigues AC, Chang MR, Nóbrega GD, Rodrigues MS, Carvalho NC, et al. Metallo-β-lactamase and genetic diversity of Pseudomonas aeruginosa in intensive care units in Campo Grande, MS, Brazil. Braz J Infect Dis. 2011;15:195–9.
Karlowsky JA, Hoban DJ, Hackel MA, Lob SH, Sahm DF. Antimicrobial susceptibility of Gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Asia-Pacific countries: SMART 2013-2015. J Med Microbiol. 2017;66:61–9.
Mediavilla JR, Patrawalla A, Chen L, Chavda KD, Mathema B, et al. Colistin- and carbapenem-resistant Escherichia coli harboring mcr-1 and blaNDM-5, causing a complicated urinary tract infection in a patient from the United States. MBio. 2016;30:7.
Hiraiwa Y, Minowa N, Usui T, Akiyama Y, Maebashi K, et al. Effect of varying the 4”-position of arbekacin derivatives on antibacterial activity against MRSA and Pseudomonas aeruginosa. Bioorg Med Chem Lett. 2007;17:6369–72.
Masuda N, Sakagawa E, Ohya S, Gotoh N, Tsujimoto H, et al. Contribution of the MexX-MexY-oprM efflux system to intrinsic resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2000;44:2242–6.
Performance standards for antimicrobial susceptibility testing; Twenty-second informational supplement. Clinical and Laboratory Standards Institute. 2012;M100-S22.
Takahashi Y, Umemura E, Kobayashi Y, Murakami S, Nawa T et al. Discovery of 2-hydroxyarbekacin, a new aminoglycoside antibiotic with reduced nephrotoxicity. J Antibiot 2017;1–3. https://doi.org/10.1038/ja.2017.60.
Kondo S, Iinuma K, Yamamoto H. Syntheses of 1-N-(S)-4-amino-2-hydroxybutyryl)-kanamycin B and -3′, 4′-dideoxykanamycin B active against kanamycin-resistant bacteria. J Antibiot. 1973;26:412–5.
Hiraiwa Y, Usui T, Akiyama Y, Maebashi K, Minowa N. Synthesis and antibacterial activity of 5-deoxy-5-episubstituted arbekacin derivatives. Bioorg Med Chem Lett. 2007;17:3540–3.
Magnet S, Blanchard JS. Molecular insights into aminoglycoside action and resistance. Chem Rev. 2005;105:477–98.
Goto H, Iwasaki M. Susceptibilities of bacteria isolated from patients with lower respiratory infectious diseases to antibacterial agents. Jpn J Antibiot. 2015;68:85–104. (2010)
Matsumoto T. Arbekacin: another novel agent for treating infections due to methicillin-resistant Staphylococcus aureus and multidrug-resistant Gram-negative pathogens. Clin Pharmacol. 2014;6:139–48.
Holbrook SY, Garneau-Tsodikova S. Expanding aminoglycoside resistance enzyme regiospecificity by mutation and truncation. Biochemistry. 2016;55:5726–37.
Tabata M, Shimizu M, Araake M, Ogawa H. Relationship between arbekacin-susceptibility and aminoglycoside-resistant gene of methicillin-resistant Staphylococcus aureus (MRSA). Jpn J Antibiot. 2003;56:36–43.
Keith P. Aminoglycoside resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:479–87.
Cass RT, Brooks CD, Havrilla NA, Tack KJ, Borin MT, et al. Pharmacokinetics and safety of single and multiple doses of ACHN-490 injection administered intravenously in healthy subjects. Antimicrob Agents Chemother. 2011;55:5874–80.
Acknowledgements
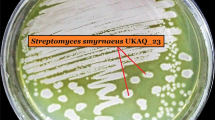
We thank Prof. Naomasa Gotoh, Kyoto Pharmaceutuical University, for kindly providing us with P. aeruginosa PAO1 and its ΔmexXY/oprM derivative strain. We also thank Ms. Erumi Murase for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirai, Y., Maebashi, K., Fushimi, H. et al. In vitro and in vivo antimicrobial activity of TS2037, a novel aminoglycoside antibiotic. J Antibiot 71, 363–371 (2018). https://doi.org/10.1038/s41429-017-0002-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41429-017-0002-2