Abstract
This study focuses on the activity of previously reported imine and β-lactam derivatives against methicillin-resistant Staphylococcus aureus (MRSA) isolates. The presence of mecA and blaZ genes in the isolates was determined, and the minimum inhibitory concentration (MIC) values were determined based on the antibacterial activity against these isolates. Active compounds were selected and their ability to act against resistant isolates in vitro was determined. Concurrently, biochemical (nitrocefin) and molecular (qRT-PCR) tests were used to investigate the ability of the compounds to induce resistance genes in MRSA isolates. The cytotoxicity of the compounds on human dermal fibroblasts (HDF) was investigated. The MIC values of compounds (10) and (12) against MSSA and MRSA isolates were 7.81 and 15.62 μg ml−1, respectively. The most active compounds were identified as (10) and (12), and it was observed that the isolates did not develop resistance to these compounds in vitro. These compounds were found to inhibit β-lactamase, reduce the expression of resistance genes, and exhibit reduced HDF cell toxicity in a dose-dependent manner. According to the findings of the study, it can be concluded that these compounds show promise as hits with an interesting mechanism of action for further chemical modifications to develop new MRSA inhibitors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article.
References
Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277–83.
Ciftci A, Aksoy A. Acquired Resistance Mechanisms Against Antibiotics. Turkiye Klinikleri J Vet Sci Pharmacol Toxicol-Spec Top. 2015;1:1–10.
Copeland RA. Conformational adaptation in drug-target interactions and residence time. Future Med Chem. 2011;3:1491–501.
Cloete R, Oppon E, Murungi E, Schubert W-D, Christoffels A. Resistance related metabolic pathways for drug target identification in Mycobacterium tuberculosis. BMC Bioinform. 2016;17:75–75. https://doi.org/10.1186/s12859-016-0898-8.
Santajit S, Indrawattana N. Mechanisms of antimicrobial resistance in ESKAPE pathogens. Biomed Res Int. 2016;2016:1–8. https://doi.org/10.1155/2016/2475067.
May KL, Grabowicz M. The bacterial outer membrane is an evolving antibiotic barrier. Proc Natl Acad Sci. 2018;115:8852.
Sun J, Deng Z, Yan A. Bacterial multidrug efflux pumps: Mechanisms, physiology and pharmacological exploitations. Biochem Biophys Res Commun. 2014;453:254–67.
Reygaert WC. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiol. 2018;4:482–501. https://doi.org/10.3934/microbiol.2018.3.482.
Worthington RJ, Melander C. Overcoming resistance to β-lactam antibiotics. J Org Chem. 2013;78:4207–13.
Garneau-Tsodikova S, Labby KJ. Mechanisms of resistance to aminoglycoside antibiotics: overview and perspectives. Medchemcomm. 2016;7:11–27.
Uzun B, Güngör S, Pektaş B, Aksoy Gökmen A, Yula E, Koçal F, et al. Macrolide-lincosamide-streptogramin B (MLSB) resistance phenotypes in clinical Staphylococcus isolates and investigation of telithromycin activity. Mikrobiyol Bul. 2014;48:469–76.
Yushchuk O, Binda E, Marinelli F. Glycopeptide antibiotic resistance genes: distribution and function in the producer actinomycetes. Front Microbiol. 2020;11:1173–1173.
Grossman TH. Tetracycline antibiotics and resistance. Cold Spring Harb Perspect Med. 2016;6:a025387–a. https://doi.org/10.1101/cshperspect.a025387.
Khawcharoenporn T, Vasoo S, Ward E, Singh K. High rates of quinolone resistance among urinary tract infections in the ED. Am J Emerg Med. 2012;30:68–74.
Goldstein BP. Resistance to rifampicin: a review. J Antibiot (Tokyo). 2014;67:625–30.
Schmitz F-J, Fluit AC. Chapter 131 - Mechanisms of antibacterial resistance. In: Cohen J, Opal SM, Powderly WG, editors. Infectious diseases (Third Edition). London: Mosby; 2010. p. 1308-22.
Turner NA, Sharma-Kuinkel BK, Maskarinec SA, Eichenberger EM, Shah PP, Carugati M, et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol. 2019;17:203–18. https://doi.org/10.1038/s41579-018-0147-4.
Andrade MM, Luiz WB, da Silva Oliveira Souza R, Amorim JH. The History of Methicillin-Resistant Staphylococcus aureus in Brazil. Can J Infect Dis Med Microbiol. 2020;2020:1–18. https://doi.org/10.1155/2020/1721936.
Brahma U, Sharma P, Murthy S, Sharma S, Chakraborty S, Appalaraju SN, et al. Decreased expression of femXAB genes and fnbp mediated biofilm pathways in OS-MRSA clinical isolates. Sci Rep. 2019;9:16028 https://doi.org/10.1038/s41598-019-52557-z.
Shalaby M-AW, Dokla EME, Serya RAT, Abouzid KAM. Penicillin binding protein 2a: An overview and a medicinal chemistry perspective. Eur J Med Chem. 2020;199:112312.
Kuehl R, Morata L, Meylan S, Mensa J, Soriano A. When antibiotics fail: a clinical and microbiological perspective on antibiotic tolerance and persistence of Staphylococcus aureus. J Antimicrob Chemother. 2020;75:1071–86. https://doi.org/10.1093/jac/dkz559.
Guignard B, Vouillamoz J, Giddey M, Moreillon PA. A positive interaction between inhibitors of protein synthesis and cefepime in the fight against methicillin-resistant Staphylococcus aureus. Eur J Clin Microbiol Infect Dis. 2013;32:899–907.
Zapun A, Contreras-Martel C, Vernet T. Penicillin-binding proteins and β-lactam resistance. FEMS Microbiol Rev. 2008;32:361–85.
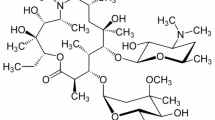
Yildirim M, Ozgeris B, Gormez A. Substituted phenethylamine-based 8-lactam derivatives: Antimicrobial, anticancer, and 8-lactamase inhibitory properties. Bioorg Chem. 2022;129:106212.
Ulucay O, Gormez A, Ozic C. Identification, characterization and hydrolase producing performance of thermophilic bacteria: geothermal hot springs in the Eastern and Southeastern Anatolia Regions of Turkey. Antonie van Leeuwenhoek. 2022;115:253–70. https://doi.org/10.1007/s10482-021-01678-5.
Chung PY, Chung LY, Navaratnam P. Transcriptional profiles of the response of methicillin-resistant staphylococcus aureus to pentacyclic triterpenoids. Plos One. 2013;8:e56687 https://doi.org/10.1371/journal.pone.0056687.
Liu XF, Pai PJ, Zhang WP, Hu YW, Dong XJ, Qian PY, et al. Proteomic response of methicillin-resistant S. aureus to a synergistic antibacterial drug combination: a novel erythromycin derivative and oxacillin. Sci Rep. 2016;6 https://doi.org/10.1038/srep19841.
Gormez A, Bozari S, Yanmis D, Gulluce M, Sahin F, Agar G. Chemical composition and antibacterial activity of essential oils of two species of lamiaceae against phytopathogenic bacteria. Pol J Microbiol. 2015;64:121–7.
Ruzin A, Petersen PJ, Jones CH. Resistance development profiling of piperacillin in combination with the novel beta-lactamase inhibitor BLI-489. J Antimicrob Chemother. 2010;65:252–7. https://doi.org/10.1093/jac/dkp435.
Haste NM, Hughes CC, Tran DN, Fenical W, Jensen PR, Nizet V, Hensler ME. Pharmacological properties of the marine natural product marinopyrrole A against methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2011;55:3305–12. https://doi.org/10.1128/AAC.01211-10.
Atshan SS, Shamsudin MN, Lung LT, Ling KH, Sekawi Z, Pei CP, Ghaznavi-Rad E. Improved method for the isolation of RNA from bacteria refractory to disruption, including S. aureus producing biofilm. Gene. 2012;494:219–24. https://doi.org/10.1016/j.gene.2011.12.010.
Narrandes S, Xu W. Gene expression detection assay for cancer clinical use. J Cancer. 2018;9:2249–65.
Ghavami A, Labbé G, Brem J, Goodfellow VJ, Marrone L, Tanner CA, King DT, Lam M, Strynadka NCJ, Pillai DR, Siemann S, Spencer J, Schofield CJ, Dmitrienko GI. Assay for drug discovery: Synthesis and testing of nitrocefin analogues for use as β-lactamase substrates. Anal Biochem. 2015;486:75–77. https://doi.org/10.1016/j.ab.2015.06.032.
Barlak N, Sanlı F, Capik O, Tuysuz E, Aydın Karataş E, Turkez H, Karatas OF. Metformin treatment sensitizes human laryngeal cancer cell line hep-2 to 5-fluorouracil. Clin Cancer Drugs. 2020;7:16–24. https://doi.org/10.2174/2212697X06666190906165309.
Kaci FN, Ruzgar D, Gormez A, Efe D. The evaluation of cytotoxic and antibacterial activity of the ethanol extract of Punica granatum L. Peels. J Inst Sci Technol. 2021;11:2319–27. https://dergipark.org.tr/en/pub/jist/issue/64410/875449.
Takayama Y, Tanaka T, Oikawa K, Fukano N, Goto M, Takahashi T. Prevalence of blaZ gene and performance of phenotypic tests to detect penicillinase in Staphylococcus aureus Isolates from Japan. Ann Lab Med. 2018;38:155–9.
Dulger D, Ekici S, Albuz O, Pakdemirli A. Investigation of Nasal Staphylococcus aureus carriage in hospital employees and rapid detection of PVL and mecA genes by RT-PCR. Etlik Vet Mikrobiyol Derg 2022;31:47–51.
Iravani Mohammad Abadi M, Moniri R, Khorshidi A, Piroozmand A, Mousavi SGA, Dastehgoli K, et al. Molecular characteristics of nasal carriage methicillin-resistant coagulase negative staphylococci in school students. Jundishapur J Microbiol. 2015;8:e18591–e. https://doi.org/10.5812/jjm.18591v2. 2015
Ray MD, Boundy S, Archer GL. Transfer of the methicillin resistance genomic island among staphylococci by conjugation. Mol Microbiol. 2016;100:675–85.
Mobasherizadeh S, Shojaei H, Azadi D, Havaei SA, Rostami S. Molecular characterization and genotyping of methicillin-resistant Staphylococcus aureus in nasal carriage of healthy Iranian children. J Med Microbiol. 2019;68:374–8. https://doi.org/10.1099/jmm.0.000924.
Ibrahim OMA, Bilal NE, Osman OF, Magzoub MA. Assessment of methicillin resistant Staphylococcus aureus detection methods: analytical comparative study. Pan Afr Med J. 2017;27:281 https://doi.org/10.11604/pamj.2017.27.281.9016.
Bagcigil AF, Taponen S, Koort J, Bengtsson B, Myllyniemi AL, Pyorala S. Genetic basis of penicillin resistance of S. aureus isolated in bovine mastitis. Acta Vet Scand. 2012;54. https://doi.org/10.1186/1751-0147-54-69.
Kriegeskorte A, Ballhausen B, Idelevich E, Köck R, Friedrich A, Karch H, et al. Human MRSA isolates with novel genetic homolog, Germany. Emerg Infect Dis. 2012;18:1016–8. https://doi.org/10.3201/eid1806.110910.
Laica SP, Andrade CF, Orellana PP, Ramos RR. Resistance to beta-lactams in Staphylococcus aureus isolated from cell phone screens of dentistry students based on an antibiogram and detection of blaZ and mecA genes. Genet Mol Res. 2021;20:gmr18931 https://doi.org/10.4238/gmr18931.
Shi L, Mao WJ, Yang Y, Zhu HL. Synthesis, characterization, and biological activity of a Schiff-base Zn(II) complex. J Coord Chem. 2009;62:3471–7.
Schroeder M, Horne SM, Prüß BM. Efficacy of β-phenylethylamine as a novel anti-microbial and application as a liquid catheter flush. J Med Microbiol. 2018;67:1778–88.
Gładkowski W, Siepka M, Janeczko T, Kostrzewa-Susłow E, Popłoński J, Mazur M, Żarowska B, Łaba W, Maciejewska G, Wawrzeńczyk C. Synthesis and antimicrobial activity of methoxy- substituted γ-Oxa-ε-lactones derived from flavanones. Molecules. 2019;24:4151 https://doi.org/10.3390/molecules24224151.
Gopalakrishnan M, Thanusu J, Kanagarajan V. Design, synthesis, spectral analysis and in vitro microbiological evaluation of 2-phenyl-3-(4,6-diarylpyrimidin-2-yl)thiazolidin-4-ones. J Enzym Inhibition Medicinal Chem. 2009;24:1088–94.
Limban C, Chifiriuc MC, Caproiu MT, Dumitrascu F, Ferbinteanu M, Pintilie L, et al. New substituted benzoylthiourea derivatives: from design to antimicrobial applications. Molecules. 2020;25:1478.
Ozgeris B. Synthesis of substituted phenethylamine-based thioureas and their antimicrobial and antioxidant properties. Russ J Org Chem. 2021;57:422–9. https://doi.org/10.1134/S1070428021030143.
Lahiri SD, Alm RA. Potential of Staphylococcus aureus isolates carrying different PBP2a alleles to develop resistance to ceftaroline. J Antimicrob Chemother. 2016;71:34–40. https://doi.org/10.1093/jac/dkv329.
Man NYT, Knight DR, Stewart SG, McKinley AJ, Riley TV, Hammer KA. Spectrum of antibacterial activity and mode of action of a novel tris-stilbene bacteriostatic compound. Sci Rep. 2018;8:6912 https://doi.org/10.1038/s41598-018-25080-w.
Soliman MK, Abozahra R, Gaafar AY, Younes AM, Affr NA. Determination of mecA expression and other resistance mechanisms in methicillin-resistant Staphylococcus aureus isolated from Oreochromis niloticus (Nile tilapia). Afr J Microbiol Res. 2016;10:481–5. https://doi.org/10.5897/AJMR2015.7859.
Gillard K, Miller HB, Blackledge MS. Tricyclic amine antidepressants suppress β-lactam resistance in methicillin-resistant Staphylococcus aureus (MRSA) by repressing mRNA levels of key resistance genes. Chem Biol Drug Des. 2018;92:1822–9.
Liu X, Ma L, Chen F, Liu J, Yang H, Lu Z. Synergistic antibacterial mechanism of Bi2Te3 nanoparticles combined with the ineffective β-lactam antibiotic cefotaxime against methicillin-resistant Staphylococcus aureus. J Inorg Biochem. 2019;196:110687 https://doi.org/10.1016/j.jinorgbio.2019.04.001.
Barreto EF, Webb AJ, Pais GM, Rule AD, Jannetto PJ, Scheetz MH. Setting the beta-lactam therapeutic range for critically ill patients: is there a floor or even a ceiling? Crit Care Explorations. 2021;3:e0446–e. https://doi.org/10.1097/CCE.0000000000000446.
Desai NC, Vaghani HV, Patel BY, Karkar TJ. Synthesis and antimicrobial activity of fluorine containing pyrazole-clubbed dihydropyrimidinones. Indian J Pharm Sci. 2018;80:242–52.
Özgeriş FB, Özgeriş B. Synthesis, characterization, and biological evaluations of substituted phenethylamine-based urea as anticancer and antioxidant agents. Monatsh Chem. 2021;152:1241–50. https://doi.org/10.1007/s00706-021-02830-7.
Acknowledgements
This study was supported by Erzurum Technical University (Master’s Thesis Project, 2021/004) and is based on the MSc thesis of Merve Yıldırım. We would like to thank Erzurum Technical University and YUTAM (High Technology and Research Center) for their financial support and research conditions.
Author information
Authors and Affiliations
Contributions
MY performed the analyses and wrote the first draft of the manuscript. AG and BO supervised the study and interpreted the results. All authors contributed to the revision of the manuscript and have read and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yildirim, M., Ozgeris, B. & Gormez, A. The effect of novel β-lactam derivatives synthesized from substituted phenethylamines on resistance genes of MRSA isolates. J Antibiot 77, 802–811 (2024). https://doi.org/10.1038/s41429-024-00769-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41429-024-00769-5