Abstract
Porphyromonas gingivalis, a Gram-negative anaerobic bacterium, is a key pathogen in chronic periodontitis. P. gingivalis has a type IX secretion system (T9SS) that secretes highly hydrolytic proteinases called gingipains for obtaining peptides as an energy source. Although most T9SS-related proteins have been identified, no specific inhibitor of T9SS has been reported. To screen T9SS inhibitors, we focused on and characterized a minimal liquid medium called mC medium that contains milk casein as the sole protein source. We found that P. gingivalis wild-type strain ATCC 33277 caused cloudiness of mC medium without growth. In mC medium, an alkylating agent, iodoacetamide (IAM) that is an inhibitor of gingipains, and a protonophore, carbonyl cyanide 3-chlorophenylhydrazone (CCCP) that dissipates the proton motive force required for T9SS-mediated secretion, clearly inhibited the increase in turbidity. Moreover, neither the gingipain-null mutant nor the T9SS-deficient mutant caused mC medium cloudiness, suggesting that mC medium cloudiness is dependent on gingipain activity and T9SS. These results indicated that mC medium can be used to assess P. gingivalis gingipain activity and its functional T9SS. Using an assay system with mC medium, we discovered that OM-173αA and OM-173βA in the Ōmura Natural Compound Library and nanaomycin A were probable T9SS inhibitors. The compounds need to be further investigated as tools for analyzing T9SS and as potential therapeutic agents for periodontal disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Supplementary information is available at Journal of Antibiotics website.
References
How KY, Song KP, Chan KG. Porphyromonas gingivalis: an overview of periodontopathic pathogen below the gum line. Front Microbiol. 2016;7:53.
Goulas T, Mizgalska D, Garcia-Ferrer I, Kantyka T, Guevara T, Szmigielski B, et al. Structure and mechanism of a bacterial host-protein citrullinating virulence factor, Porphyromonas gingivalis peptidylarginine deiminase. Sci Rep. 2015;5:11969.
Jia S, Li X, Du Q. Host insulin resistance caused by Porphyromonas gingivalis-review of recent progresses. Front Cell Infect Microbiol. 2023;13:1209381.
Li Y, Guo R, Oduro PK, Sun T, Chen H, Yi Y, et al. The relationship between Porphyromonas gingivalis and rheumatoid arthritis: a meta-analysis. Front Cell Infect Microbiol. 2022;12:956417.
Liu Y, Wu Z, Nakanishi Y, Ni J, Hayashi Y, Takayama F, et al. Infection of microglia with Porphyromonas gingivalis promotes cell migration and an inflammatory response through the gingipain-mediated activation of protease-activated receptor-2 in mice. Sci Rep. 2017;7:11759.
Miyauchi M, Ao M, Furusho H, Chea C, Nagasaki A, Sakamoto S, et al. Galectin-3 plays an important role in preterm birth caused by dental infection of Porphyromonas gingivalis. Sci Rep. 2018;8:2867.
Ryder MI. Porphyromonas gingivalis and Alzheimer disease: recent findings and potential therapies. J Periodontol. 2020;91:S45–S49.
Potempa J, Travis J. Porphyromonas gingivalis proteinases in periodontitis, a review. Acta Biochim Pol. 1996;43:455–65.
Sato K, Sakai E, Veith PD, Shoji M, Kikuchi Y, Yukitake H, et al. Identification of a new membrane-associated protein that influences transport/maturation of gingipains and adhesins of Porphyromonas gingivalis. J Biol Chem. 2005;280:8668–77.
Sato K, Naito M, Yukitake H, Hirakawa H, Shoji M, McBride MJ, et al. A protein secretion system linked to bacteroidete gliding motility and pathogenesis. Proc Natl Acad Sci USA. 2010;107:276–81.
Seers CA, Slakeski N, Veith PD, Nikolof T, Chen YY, Dashper SG, et al. The RgpB C-terminal domain has a role in attachment of RgpB to the outer membrane and belongs to a novel C-terminal-domain family found in Porphyromonas gingivalis. J Bacteriol. 2006;188:6376–86.
Veith PD, Glew MD, Gorasia DG, Cascales E, Reynolds EC. The type IX secretion system and its role in bacterial function and pathogenesis. J Dent Res. 2022;101:374–83.
Hennell James R, Deme JC, Hunter A, Berks BC, Lea SM. Structures of the Type IX Secretion/Gliding Motility Motor from across the Phylum Bacteroidetes. mBio. 2022;13:e0026722.
Kita D, Shibata S, Kikuchi Y, Kokubu E, Nakayama K, Saito A, et al. Involvement of the type IX secretion system in Capnocytophaga ochracea gliding motility and biofilm formation. Appl Environ Microbiol. 2016;82:1756–66.
Kondo Y, Sato K, Nagano K, Nishiguchi M, Hoshino T, Fujiwara T, et al. Involvement of PorK, a component of the type IX secretion system, in Prevotella melaninogenica pathogenicity. Microbiol Immunol. 2018;62:554–66.
Naito M, Shoji M, Sato K, Nakayama K. Insertional inactivation and gene complementation of Prevotella intermedia type IX secretion system reveals its indispensable roles in black pigmentation, hemagglutination, protease activity of interpain A, and biofilm formation. J Bacteriol. 2022;204:e0020322.
Narita Y, Sato K, Yukitake H, Shoji M, Nakane D, Nagano K, et al. Lack of a surface layer in Tannerella forsythia mutants deficient in the type IX secretion system. Microbiology. 2014;160:2295–303.
Li Y, Watanabe E, Kawashima Y, Plichta DR, Wang Z, Ujike M, et al. Identification of trypsin-degrading commensals in the large intestine. Nature. 2022;609:582–9.
Barbier P, Rochat T, Mohammed HH, Wiens GD, Bernardet JF, Halpern D, et al. The type IX secretion system is required for virulence of the fish pathogen Flavobacterium psychrophilum. Appl Environ Microbiol. 2020;86:e00799–20.
McBride MJ, Nakane D. Flavobacterium gliding motility and the type IX secretion system. Curr Opin Microbiol. 2015;28:72–7.
Hennell James R, Deme JC, Kjӕr A, Alcock F, Silale A, Lauber F, et al. Structure and mechanism of the proton-driven motor that powers type 9 secretion and gliding motility. Nat Microbiol. 2021;6:221–33.
Nakane D, Sato K, Wada H, McBride MJ, Nakayama K. Helical flow of surface protein required for bacterial gliding motility. Proc Natl Acad Sci USA. 2013;110:11145–50.
Vincent MS, Comas Hervada C, Sebban-Kreuzer C, Le Guenno H, Chabalier M, Kosta A, et al. Dynamic proton-dependent motors power type IX secretion and gliding motility in Flavobacterium. PLoS Biol. 2022;20:e3001443.
Sasaki Y, Shoji M, Sueyoshi T, Shibata S, Matsuo T, Yukitake H, et al. A conditional gene expression system in Porphyromonas gingivalis for study of the secretion mechanisms of lipoproteins and T9SS cargo proteins. Mol Oral Microbiol. 2023;38:321–33.
Shoji M, Sato K, Yukitake H, Kondo Y, Narita Y, Kadowaki T, et al. Por secretion system-dependent secretion and glycosylation of Porphyromonas gingivalis hemin-binding protein 35. PLoS ONE. 2011;6:e21372.
Saiki K, Urano-Tashiro Y, Takahashi Y. Reassessment of minimal media reveals differences in growth among Porphyromonas gingivalis standard strains. J Oral Biosci. 2020;62:315–21.
Omura S, Tanaka H, Koyama Y, Oiwa R, Katagiri M, Awaya J, et al. Nanaomycins A and B*, new antibiotics produced by a strain of Streptomyces. J Antibiot. 1974;27:363–5.
Shoji M, Shibata S, Naito M, Nakayama K. Transport and Polymerization of Porphyromonas gingivalis Type V Pili. Methods Mol Biol. 2021;2210:61–73.
Yukitake H, Shoji M, Sato K, Handa Y, Naito M, Imada K, et al. PorA, a conserved C-terminal domain-containing protein, impacts the PorXY-SigP signaling of the type IX secretion system. Sci Rep. 2020;10:21109.
Coultate T. Food: The chemistry of its components. 7th ed. London: Royal Society of Chemistry; 2023.
Abe N, Kadowaki T, Okamoto K, Nakayama K, Ohishi M, Yamamoto K. Biochemical and functional properties of lysine-specific cysteine proteinase (Lys-gingipain) as a virulence factor of Porphyromonas gingivalis in periodontal disease. J Biochem. 1998;123:305–12.
Song L, Perpich JD, Wu C, Doan T, Nowakowska Z, Potempa J, et al. A unique bacterial secretion machinery with multiple secretion centers. Proc Natl Acad Sci USA. 2022;119:e2119907119.
Ōmura S. Microbial metabolites: 45 years of wandering, wondering and discovering. Tetrahedron. 2011;67:6420–59.
Ōmura S, Iwai Y, Hinotozawa K, Takahashi Y, Kato J, Nakagawa A, et al. Cervinomycin A1 and A2, new antibiotics active against anaerobes, produced by Streptomyces cervinus sp. nov. J Antibiot. 1982;35:645–52.
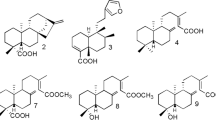
Iwai Y, Kimura K, Takahashi Y, Hinotozawa K, Shimizu H, Tanaka H, et al. OM-173, new nanaomycin-type antibiotics produced by a strain of Streptomyces. Taxonomy, production, isolation and biological properties. J Antibiot. 1983;36:1268–74.
Hayashi M, Unemoto T, Minami-Kakinuma S, Tanaka H, Ōmura S. The mode of action of nanaomycins D and A on a gram-negative marine bacterium Vibrio alginolyticus. J Antibiot. 1982;35:1078–85.
Marumo H, Kitaura K, Morimoto M, Tanaka H, Ōmura S. The mode of action of nanaomycin A in Gram-positive bacteria. J Antibiot. 1980;33:885–90.
Kuck D, Caulfield T, Lyko F, Medina-Franco JL. Nanaomycin A selectively inhibits DNMT3B and reactivates silenced tumor suppressor genes in human cancer cells. Mol Cancer Ther. 2010;9:3015–23.
Milner P, Batten JE, Curtis MA. Development of a simple chemically defined medium for Porphyromonas gingivalis: requirement for alpha-ketoglutarate. FEMS Microbiol Lett. 1996;140:125–30.
Oda H, Saiki K, Numabe Y, Konishi K. Effect of gamma-immunoglobulin on the asaccharolytic growth of Porphyromonas gingivalis. J Periodontal Res. 2007;42:438–42.
Saiki K, Urano-Tashiro Y, Konishi K, Takahashi Y. A screening system using minimal media identifies a flavin-competing inhibitor of Porphyromonas gingivalis growth. FEMS Microbiol Lett. 2019;366:fnz204.
Saiki K, Urano-Tashiro Y, Yamanaka Y, Takahashi Y. Calcium ions and vitamin B12 are growth factors for Porphyromonas gingivalis. J Oral Biosci. 2022;64:445–51.
Nicosia FD, Puglisi I, Pino A, Caggia C, Randazzo CL. Plant milk-clotting enzymes for cheesemaking. Foods. 2022;11:871.
Wang X, Zhao Q, He L, Shi Y, Fan J, Chen Y, et al. Milk-clotting properties on bovine caseins of a novel cysteine peptidase from germinated Moringa oleifera seeds. J Dairy Sci. 2022;105:3770–81.
Karlsson A, Arvidson S. Variation in extracellular protease production among clinical isolates of Staphylococcus aureus due to different levels of expression of the protease repressor sarA. Infect Immun. 2002;70:4239–46.
Ikeda T, Yoshimura F. A resistance-nodulation-cell division family xenobiotic efflux pump in an obligate anaerobe, Porphyromonas gingivalis. Antimicrob Agents Chemother. 2002;46:3257–60.
Olczak T, Simpson W, Liu X, Genco CA. Iron and heme utilization in Porphyromonas gingivalis. FEMS Microbiol Rev. 2005;29:119–44.
Meuric V, Rouillon A, Chandad F, Bonnaure-Mallet M. Putative Respiratory Chain of Porphyromonas gingivalis. Future Microbiol. 2010;5:717–34.
Wen A, Chen Y, Yuan S, Yu H, Guo Y, Cheng Y, et al. Elucidation of the binding behavior between tetracycline and bovine casein by multi-spectroscopic and molecular simulation methods. J Lumin. 2023;260:199879.
Acknowledgements
The enormous contribution of MS to this research, including the planning, execution, and paper preparation of this study, should be deeply emphasized. He had a great passion for science throughout his life. The authors thank H. Yukitake for discussions and continuous advice on experimental techniques and K. Nakayama for his support in preparing the revised manuscript. This work was supported by grants from Nagasaki University WISE Program Application Guidance for the Grant for Global Health Research Collaboration to MN, and the Platform Project for Supporting Drug Discovery and Life Science Research (Basis for Supporting Innovative Drug Discovery and Life Science Research (BINDS)) from the Japan Agency for Medical Research & Development (AMED) under Grant Numbers JP19am0101096 (Phase I) to MI. We would like to thank Editage (http://www.editage.com) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sasaki, Y., Matsuo, T., Watanabe, Y. et al. Identification of nanaomycin A and its analogs by a newly established screening method for functional inhibitors of the type IX secretion system in Porphyromonas gingivalis. J Antibiot 78, 90–105 (2025). https://doi.org/10.1038/s41429-024-00790-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41429-024-00790-8