Abstract
Background/objectives
Disruptions in redox balance lead to oxidative stress, a promoter of morbidity in critical illness. This study aimed to: (1) characterize the plasma and alveolar thiol/disulfide redox pools, (2) examine their associations with alveolar macrophage phagocytosis, and (3) determine the effect of high dose vitamin D3 on plasma thiol/disulfide redox.
Subjects/methods
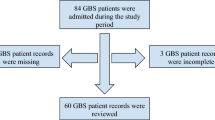
Subjects were 30 critically ill, ventilated adults in a double-blind randomized trial of high-dose (250 000 or 500 000 IU) vitamin D3 or placebo. Baseline bronchoalveolar lavage fluid (BALF) samples were analyzed for determination of alveolar phagocytosis index (PI) and for concentrations of glutathione (GSH), glutathione disulfide (GSSG), cysteine (Cys), cystine (CySS), and their respective redox potentials (EhGSSG and EhCySS). Plasma redox outcomes were assessed at baseline and days 7 and 14.
Results
Baseline plasma Cys was inversely associated with alveolar PI (ρ = −0.69, P = 0.003), and EhCySS was positively associated with PI (ρ = 0.61, P = 0.01). Over time, among all subjects there was an increase in plasma GSH levels and a decrease in EhGSSG (P < 0.01 for both), with no difference by treatment group. Vitamin D3 decreased oxidized plasma GSSG to a more normal state (P for group x time = 0.009).
Conclusions
Oxidative stress indicators were positively associated with alveolar macrophage phagocytic function in acutely ill ventilated adults. High-dose vitamin D3 decreased plasma GSSG concentrations, which suggests that vitamin D can possibly improve the oxidative stress environment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Gunaydin B, Sancak B, Candan S, Sariahmetoglu M, Ozcagli G, Tunctan B, et al. Temporal variation of oxidant stress in critically ill patients. Minerva Anestesiol. 2007;73(5):261–6.
Moriarty-Craige SE, Jones DP. Extracellular thiols and thiol/disulfide redox in metabolism. Annu Rev Nutr. 2004;24:481–509.
Grunwell JR, Gillespie SE, Ward JM, Fitzpatrick AM, Brown LA, Gauthier TW, et al. Comparison of glutathione, cysteine, and their redox potentials in the plasma of critically Ill and healthy children. Front Pediatr. 2015;3:46.
Bunnell E, Pacht ER. Oxidized glutathione is increased in the alveolar fluid of patients with the adult respiratory distress syndrome. Am Rev Respir Dis. 1993;148(5):1174–8.
Pacht ER, Timerman AP, Lykens MG, Merola AJ. Deficiency of alveolar fluid glutathione in patients with sepsis and the adult respiratory distress syndrome. Chest. 1991;100(5):1397–403.
Brune B, Dehne N, Grossmann N, Jung M, Namgaladze D, Schmid T, et al. Redox control of inflammation in macrophages. Antioxid Redox Signal. 2013;19(6):595–637.
Metukuri MR, Namas R, Gladstone C, Clermont T, Jefferson B, Barclay D, et al. Activation of latent transforming growth factor-beta1 by nitric oxide in macrophages: role of soluble guanylate cyclase and MAP kinases. Wound repair and regeneration: official publication of the Wound Healing Society [and] the European Tissue Repair. Society. 2009;17(4):578–88.
Heinloth A, Brune B, Fischer B, Galle J. Nitric oxide prevents oxidised LDL-induced p53 accumulation, cytochrome c translocation, and apoptosis in macrophages via guanylate cyclase stimulation. Atherosclerosis. 2002;162(1):93–101.
Duan J, Kodali VK, Gaffrey MJ, Guo J, Chu RK, Camp DG, et al. Quantitative profiling of protein S-glutathionylation reveals redox-dependent regulation of macrophage function during nanoparticle-induced oxidative stress. ACS Nano. 2016;10(1):524–38.
Liang Y, Yeligar SM, Brown LA. Chronic-alcohol-abuse-induced oxidative stress in the development of acute respiratory distress syndrome. Sci World J. 2012;2012:740308.
Liang Y, Harris FL, Brown LA. Alcohol induced mitochondrial oxidative stress and alveolar macrophage dysfunction. Bio Med Res Int. 2014;2014:371593.
Ke CY, Yang FL, Wu WT, Chung CH, Lee RP, Yang WT, et al. Vitamin D3 reduces tissue damage and oxidative stress caused by exhaustive exercise. Int J Med Sci. 2016;13(2):147–53.
Sales de Almeida JP, Liberatti LS, Nascimento Barros FE, Kallaur AP, Batisti Lozovoy MA, Scavuzzi BM, et al. Profile of oxidative stress markers is dependent on vitamin D levels in patients with chronic hepatitis C. Nutrition. 2016;32(3):362–7.
Kanikarla-Marie P, Jain SK. 1,25(OH)2D3 inhibits oxidative stress and monocyte adhesion by mediating the upregulation of GCLC and GSH in endothelial cells treated with acetoacetate (ketosis). J Steroid Biochem Mol Biol. 2016;159:94–101.
de Medeiros Cavalcante IG, Silva AS, Costa MJ, Persuhn DC, Issa CI, de Luna Freire TL, et al. Effect of vitamin D3 supplementation and influence of BsmI polymorphism of the VDR gene of the inflammatory profile and oxidative stress in elderly women with vitamin D insufficiency: Vitamin D3 megadose reduces inflammatory markers. Exp Gerontol. 2015;66:10–6.
Shab-Bidar S, Neyestani TR, Djazayery A. The interactive effect of improvement of vitamin D status and VDR FokI variants on oxidative stress in type 2 diabetic subjects: a randomized controlled trial. Eur J Clin Nutr. 2015;69(2):216–22.
Jeng L, Yamshchikov AV, Judd SE, Blumberg HM, Martin GS, Ziegler TR, et al. Alterations in vitamin D status and anti-microbial peptide levels in patients in the intensive care unit with sepsis. J Transl Med. 2009;7:28.
Mata-Granados JM, Vargas-Vasserot J, Ferreiro-Vera C, Luque de Castro MD, Pavon RG, Quesada Gomez JM. Evaluation of vitamin D endocrine system (VDES) status and response to treatment of patients in intensive care units (ICUs) using an on-line SPE-LC-MS/MS method. J Steroid Biochem Mol Biol. 2010;121(1-2):452–5.
Higgins DM, Wischmeyer PE, Queensland KM, Sillau SH, Sufit AJ, Heyland DK. Relationship of vitamin D deficiency to clinical outcomes in critically ill patients. J Parenter Enter Nutr. 2012;36(6):713–20.
Nair P, Lee P, Reynolds C, Nguyen ND, Myburgh J, Eisman JA, et al. Significant perturbation of vitamin D-parathyroid-calcium axis and adverse clinical outcomes in critically ill patients. Intensive Care Med. 2013;39(2):267–74.
Han JE, Jones JL, Tangpricha V, Brown MA, Brown LA, Hao L, et al. High dose vitamin D administration in ventilated intensive care unit patients: A pilot double blind randomized controlled trial. J Clin Transl Endocrinol. 2016;4:59–65.
Amrein K, Schnedl C, Holl A, Riedl R, Christopher KB, Pachler C, et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA. 2014;312(15):1520–30.
Alvarez JA, Chowdhury R, Jones DP, Martin GS, Brigham KL, Binongo JN, et al. Vitamin D status is independently associated with plasma glutathione and cysteine thiol/disulphide redox status in adults. Clin Endocrinol. 2014;81(3):458–66.
Alvarez JA, Grunwell JR, Gillespie SE, Tangpricha V, Hebbar KB, Vitamin D deficiency is associated with an oxidized plasma cysteine redox potential in critically Ill children. J Steroid Biochem Mol Biol. 2018;175:164–9.
Gauthier TW, Ping XD, Harris FL, Wong M, Elbahesh H, Brown LA. Fetal alcohol exposure impairs alveolar macrophage function via decreased glutathione availability. Pediatr Res. 2005;57(1):76–81.
Yeh MY, Burnham EL, Moss M, Brown LA. Chronic alcoholism alters systemic and pulmonary glutathione redox status. Am J Respir Crit Care Med. 2007;176(3):270–6.
Jones DP, Liang Y. Measuring the poise of thiol/disulfide couples in vivo. Free Radic Biol Med. 2009;47(10):1329–38.
Jain SK, Micinski D. Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem Biophys Res Commun. 2013;437(1):7–11.
Acknowledgements
We would like to acknowledge Mona Brown, Guatam Hebbar, Jennifer Jones, Frank Harris, and Janine Ward for their contribution to the study.
Funding
This project was supported, in part, by National Institutes of Health grants: NIH R21 HL110044 (GSM, TRZ, LAB, VT, JEH), K24 DK096574 (TRZ), UL1 TR000454 (JEH, GSM, TRZ, VT), K01 DK102851 (JAA), T32 HL076118 (BS), and T32 AA013528 (JEH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Han, J.E., Alvarez, J.A., Staitieh, B. et al. Oxidative stress in critically ill ventilated adults: effects of vitamin D3 and associations with alveolar macrophage function. Eur J Clin Nutr 72, 744–751 (2018). https://doi.org/10.1038/s41430-017-0047-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41430-017-0047-0