Abstract
Background/objectives
It has been unknown if attenuated insulin sensitivity (Si) in non-alcoholic fatty liver disease (NAFLD) is a cause or a result. We examined the impact of attenuated Si on NAFLD evolution.
Subjects/methods
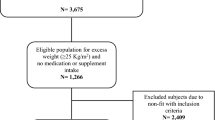
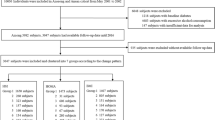
We observed 4856 NAFLD- and diabetes-free participants for a mean 2.9 years. Si was indexed by single point insulin sensitivity estimator (SPISE = [600 × HDL-c0.185]/[TG0.2 × BMI1.338]), correlating with 1/HOMA-IR in an independent cohort (n = 1537, Spearman rho = 0.519, P < 0.01). Fatty liver (FL) was diagnosed by ultrasonography and diabetes by fasting plasma glucose (FPG) ≥ 7 mmol/L and/or glycohemoglobin A1c ≥ 6.5%. Multinominal comparison was performed with incident FL (FLw/oDM, n = 486), diabetes (DMw/oFL, n = 171), and FL plus diabetes (FL/diabetes, n = 58) as targets; none of the above (n = 4,138) was the control. SPISE was taken as a predictor with adjustment for covariates. Trajectory of SPISE during the 5 years before development of each condition was also assessed.
Results
With SPISE tertile 3 (>10.06) as the reference, tertile 1 (<8.07) was related to incident FLw/oDM and FL/diabetes with OR (95% CI) 3.47 (2.60–4.63) and 1.78 (1.10–2.87), respectively, and tertile 2 (8.07–10.06) related to FLw/oDM with OR (95% CI) 1.38 (1.03–1.85). Low SPISE was not significantly related to incident diabetes. At −5 years, SPISE was 12% (P < 0.05) and 13% (P < 0.01) lower in those developed FLw/oDM and FL/diabetes, respectively, than the control. At year 0, SPISE in the two groups was 18% and 21% lower than the control, respectively (P < 0.01).
Conclusions
Attenuation of Si indexed by SPISE was a risk factor for NAFLD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Williams KH, Shackel NA, Gorrell MD, McLennan SV, Twigg SM. Diabetes and nonalcoholic fatty liver disease: a pathogenic duo. Endocr Rev. 2013;34:84–129.
Lallukka S, Yki-Järvinen H. Non-alcoholic fatty liver disease and risk of type 2 diabetes. Best Pract Res Clin Endocrinol Metab. 2016;30:385–95.
Katsiki N, Mikhailidis DP, Mantzoros CS. Non-alcoholic fatty liver disease and dyslipidemia: an update. Metabolism. 2016;65:1109–23.
Brouwers B, Schrauwen-Hinderling VB, Jelenik T, Gemmink A, Havekes B, Bruls Y, et al. Metabolic disturbances of non-alcoholic fatty liver resemble the alterations typical for type 2 diabetes. Similarity between NAFLD and DM. Clin Sci. 2017;131:1905–7.
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Paulmichl K, Hatunic M, Højlund K, Jotic A, Krebs M, Mitrakou A, et al. Beta-JUDO Investigators; RISC Investigators. Modification and validation of the triglyceride-to-HDL cholesterol ratio as a surrogate of insulin sensitivity in white juveniles and adults without diabetes mellitus: The Single Point Insulin Sensitivity Estimator (SPISE). Clin Chem. 2016;62:1211–9.
Marugame T, Yamamoto S, Yoshimi I, Sobue T, Inoue M, Tsugane S. Japan Public Health Center-based Prospective Study Group. Patterns of alcohol drinking and all-cause mortality: results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2007;165:1039–46.
Di Costanzo A, D’Erasmo L, Polimeni L, Baratta F, Coletta P, Di Martino M, et al. Non-alcoholic fatty liver disease and subclinical atherosclerosis: a comparison of metabolically- versus genetically-driven excess fat hepatic storage. Atherosclerosis. 2017;257:232–9.
Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708–15.
Martin-Rodriguez JL, Gonzalez-Cantero J, Gonzalez-Cantero A, Arrebola JP, Gonzalez-Calvin JL. Diagnostic accuracy of serum alanine aminotransferase as biomarker for nonalcoholic fatty liver disease and insulin resistance in healthy subjects, using 3T MR spectroscopy. Medicine. 2017;96:e6770.
American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2016;39(Suppl.1):S13–22.
Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, et al. APRICOT Clinical Investigators. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–25.
Sumida Y, Yoneda M, Hyogo H, Itoh Y, Ono M, Fujii H, et al. Japan Study Group of Nonalcoholic Fatty Liver Disease (JSG-NAFLD). Validation of the FIB4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol. 2012;12:2.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;6:1487–95.
Sakuma T, Yamashita K, Miyakoshi T, Shimodaira M, Yokota N, Sato Y, et al. Postchallenge Hyperglycemia in subjects with low body weight: implication for small glucose volume. Am J Physiol Endocrinol Metab. 2017;313:E748–56.
Aizawa T, Yamada M, Katakura M, Funase Y, Yamashita K, Yamauchi K. Hyperbolic correlation between insulin sensitivity and insulin secretion fades away in lean subjects with superb glucose regulation. Endocr J. 2012;59:127–36.
Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67:862–73.
Sagesaka H, Sato Y, Someya Y, Tamura Y, Shimodaira M, Miyakoshi, et al. Type 2 Diabetes: When Does It Start?. J Endocr Soc. 2018;2:476–84.
Seghieri M, Tricò D, Natali A. The impact of triglycerides on glucose tolerance: Lipotoxicity revisited. Diabetes Metab. 2017;43:314–22.
Katakura M, Komatsu M, Sato Y, Hashizume K, Aizawa T. Primacy of beta-cell dysfunction in the development of hyperglycemia: a study in the Japanese general population. Metabolism. 2004;53:949–53.
Morimoto A, Tatsumi Y, Deura K, Mizuno S, Ohno Y, Miyamatsu N, et al. Impact of impaired insulin secretion and insulin resistance on the incidence of type 2 diabetes mellitus in a Japanese population: the Saku study. Diabetologia. 2013;56:1671–9.
Tonks KT, Ng Y, Miller S, Coster AC, Samocha-Bonet D, Iseli TJ, Xu A, et al. Impaired Akt phosphorylation in insulin-resistant human muscle is accompanied by selective and heterogeneous downstream defects. Diabetologia. 2013;56:875–85.
Acknowledgements
The authors thank Yoshiko Shishido for the expertise in liver ultrasonography examinations.
Author contributions
T.M., M.S., S.U., K.K. and T.A. conceived and designed the study; T.M., H.S., Y.S., K.H., H.K., K.Y. and T.A. generated, collected, assembled, analysed and/or interpreted data. T.M., K.Y., K.K. and T.A. drafted and revised the manuscript and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Miyakoshi, T., Sagesaka, H., Sato, Y. et al. Reappraisal of attenuated insulin sensitivity in the evolution of non-alcoholic fatty liver disease. Eur J Clin Nutr 73, 770–775 (2019). https://doi.org/10.1038/s41430-018-0246-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41430-018-0246-3
This article is cited by
-
The single-point insulin sensitivity estimator (SPISE) index is a strong predictor of abnormal glucose metabolism in overweight/obese children: a long-term follow-up study
Journal of Endocrinological Investigation (2022)