Abstract
Background/objectives
Alcohol is commonly consumed around mealtimes. This study hypothesized that the association between alcohol and hypertension was influenced by overall diet quality. This study aims to test the hypothesis that overall diet quality influenced associations between alcohol and risk of hypertension across different ethnicities.
Subjects/methods
Using nationally representative data from National Health and Nutrition Examination Survey(NHANES 03–12), China Health Nutrition Survey (CHNS), and an independent population-based study, 43,914 adults were included. Subgroup analysis included 6984 adults from CHNS with a 14-year follow-up. Light alcohol consumption was defined as <7standard drinks/week, moderate as 7–21 drinks/week, and heavy as >21 drinks/week. Alternative healthy eating index and diet balance index were calculated as indicators of diet quality.
Results
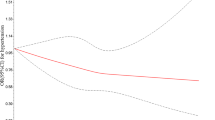
There were 3968 hypertensives in Caucasians (N = 11,325), 1976 in Africans (N = 5010), 1907 in Hispanics (N = 7274) and 5267 (N = 20,305) in Chinese. In context of high diet quality, light alcohol consumption was significantly associated with decreased risk of hypertension in Caucasians, and the risk of hypertension was not significantly increased with increasing in alcohol consumption in Caucasians, Chinese, and Hispanics (all Pfor trend > 0.05). On the contrary, in context of low diet quality, the risk of hypertension was significantly increased with increasing in alcohol consumption in Caucasians (Pfor trend = 0.005), Chinese (Pfor trend = 0.001) and Hispanics (Pfor trend = 0.022). Associations between alcohol consumption and risk of hypertension significantly varied by diet-quality scores in Caucasians, Hispanics, and Chinese (all Pfor interaction < 0.01) showing gradually changing from nonsignificant increasing trend to linear association.
Conclusions
This study firstly demonstrated that overall diet quality influenced associations between alcohol and risk of hypertension across different ethnicities, emphasizing that when examining health effects of alcohol on blood pressure, diet quality should be considered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
NHANES could be download at http://www.cdc.gov/nchs/nhanes/. CHNS could be download at http://www.cpc.unc.edu/projects/china. For HDNNCDS, researchers should contact the principal investigator if they wish to explore the possibility of collaborative work.
References
Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:51930.
Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671.
Di CA, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–45.
Howard AA, Arnsten JH, Gourevitch MN. Effect of alcohol consumption on diabetes mellitus: a systematic review. Ann Intern Med. 2004;140:211–9.
Chikritzhs T, Stockwell T, Naimi T, Andreasson S, Dangardt F, Liang W. Has the leaning tower of presumed health benefits from ‘moderate’ alcohol use finally collapsed. Addiction. 2015;110:726–7.
Yeomans MR, Caton S, Hetherington MM. Alcohol and food intake. Curr Opin Clin Nutr Metab Care. 2003;6:639–44.
Kesse E, Clavel–Chapelon F, Slimani N, van Liere M. Do eating habits differ according to alcohol consumption? Results of a study of the French cohort of the European Prospective Investigation into Cancer and Nutrition (E3N-EPIC). Am J Clin Nutr. 2001;74:322–7.
Corrao G, Lepore AR, Torchio P, Galatola G, Aricò S, Di OF. Interaction between dietary pattern and alcohol intake on the risk of liver cirrhosis. The Provincial Group for the Study of Chronic Liver Disease. Rev Epidemiol Sante Publique. 1995;43:7–17.
de Vries JH, Hollman PC, van Amersfoort I, Olthof MR, Katan MB. Red wine is a poor source of bioavailable flavonols in men. J Nutr. 2001;131:745–8.
Bloch MJ. Worldwide prevalence of hypertension exceeds 1.3 billion. J Am Soc Hypertens. 2016;10:753–4.
Han T, Gao J, Wang L, Li C, Qi L, Sun C, et al. The association of energy and macronutrient intake at dinner versus breakfast with disease-specific and all-cause mortality among people with diabetes: the U.S. National Health and Nutrition Examination Survey, 2003–2014. Diabetes Care. 2020;43:1442–8.
Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China Health and Nutrition Survey–monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;39:1435–40.
Na L, Wu X, Feng R, Li J, Han T, Lin L, et al. The Harbin Cohort Study on diet, nutrition and chronic non-communicable diseases: study design and baseline characteristics. PLoS ONE. 2015;10:e0122598.
Xu X, Hall J, Byles J, Shi Z. Assessing dietary quality of older Chinese people using the Chinese Diet Balance Index (DBI). PLoS ONE. 2015;10:e0121618.
Stade BC, Bailey C, Dzendoletas D, Sgro M, Dowswell T, Bennett D. Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning a pregnancy. Cochrane Database Syst Rev. 2009;2:CD004228.
Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N, et al. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Can Med Assoc J. 2005;172:S1–21.
John Godel MD, Canadian Pediatric Society. Fetal alcohol syndrome. Pediatr Child Health. 2002;7:161–74.
Scientific report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: Department of Agriculture; 2015.
Wang Y, Seitz HK, Wang XD. Moderate alcohol consumption aggravates high-fat diet induced steatohepatitis in rats. Alcohol Clin Exp Res. 2010;34:567–73.
Gäbele E, Dostert K, Dorn C, Patsenker E, Stickel F, Hellerbrand C. A new model of interactive effects of alcohol and high-fat diet on hepatic fibrosis. Alcohol Clin Exp Res. 2011;35:1361–7.
Chen Q, Turban S, Miller ER, Appel LJ. The effects of dietary patterns on plasma renin activity: results from the Dietary Approaches to Stop Hypertension trial. J Hum Hypertens. 2012;26:664–9.
Lin PH, Allen JD, Li YJ, Yu M, Lien LF, Svetkey LP. Blood pressure-lowering mechanisms of the DASH dietary pattern. J Nutr Metab. 2012;2012:472396.
Borgi L, Muraki I, Satija A, Willett WC, Rimm EB, Forman JP. Fruit and vegetable consumption and the incidence of hypertension in three prospective cohort studies. Hypertension. 2016;67:288–93.
Heinonen I, Rinne P, Ruohonen ST, Ruohonen S, Ahotupa M, Savontaus E. The effects of equal caloric high fat and western diet on metabolic syndrome, oxidative stress and vascular endothelial function in mice. Acta Physiol. 2014;211:515–27.
Meyer J, Döring A, Herder C, Roden M, Koenig W, Thorand B. Dietary patterns, subclinical inflammation, incident coronary heart disease and mortality in middle-aged men from the MONICA/KORA Augsburg cohort study. Eur J Clin Nutr. 2011;65:800–7.
Lopez-Garcia E, Schulze MB, Fung TT, Meigs JB, Rifai N, Manson JE, et al. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr. 2004;80:1029–35.
Zapolski TC, Pedersen SL, McCarthy DM, Smith GT. Less drinking, yet more problems: understanding African American drinking and related problems. Psychol Bull. 2014;140:188–233.
Lindhorst J, Alexander N, Blignaut J, Rayner B. Differences in hypertension between blacks and whites: an overview. Cardiovasc J Afr. 2007;18:241–7.
Acknowledgements
This research was supported funds from National Natural Science Foundation (81803227 to TH), National Key R&D Program of China (2017YFC1307401 to CS), and used data from National Health and Nutrition Examination Survey (NHANES), China Health and Nutrition Survey (CHNS) and the Harbin Cohort Study on Diet, Nutrition and Chronic Noncommunicable Disease (HDNNCDS). We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011. We are indebted to the participants of NHANES and HDNNCDS for their cooperation and participation.
Funding
This research was supported funds from National Natural Science Foundation (81803227 to TH), National Key R&D Program of China (2017YFC1307401 to CS).
Author information
Authors and Affiliations
Contributions
YL and TH planned the work. TH and CS conducted and reported the work. WJ and XM were involved in the data collection. MW, XW, and XC were involved in analysis of data. PW, WH, and YW wrote the paper. All the authors were responsible for revising the paper and approved the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jiang, W., Meng, X., Hou, W. et al. Impact of overall diet quality on association between alcohol consumption and risk of hypertension: evidence from two national surveys with multiple ethnics. Eur J Clin Nutr 75, 112–122 (2021). https://doi.org/10.1038/s41430-020-00708-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-020-00708-1