Abstract
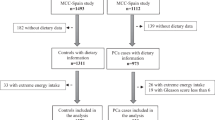
This updated meta-analysis sought to determine whether the pro-inflammatory potential of diet is a risk factor for breast cancer (BrCa) development, for the first time focusing on the effects of design heterogeneity. The search was performed using Scopus, PubMed, and Embase databases. Data were extracted from twenty-one eligible studies, including eleven cohorts (336,085 participants/20,033 incidence cases), and ten case-control studies (9,833 cases/12,752controls). The random-effect was used to calculate the relative risk (RR) using STATA 16 software. The highest dietary inflammatory index (DII) vs. the lowest category showed 16% increased risk of BrCa (95% CI: 1.06–1.26; I2 = 62.8%, P (I2) < 0.001). This was notable in post-menopausal status (RR = 1.13, 95% CI: 1.04–1.22), women with body mass index (BMI) ≥ 30 kg/m2 (RR = 1.35, 95% CI: 1.07–1.63), and study populations from developing countries (RR = 1.79, 95% CI: 1.12–2.47). Methodological covariates were subject to subgroup meta-analyses and showed stronger results among case-control studies (RR = 1.50, 95% CI: 1.20–1.80), studies considered age-matched controls (RR = 1.56, 95% CI: 1.19–1.93) and hospital-based controls (RR = 2.11, 95% CI: 1.58–2.64), and cohort studies identified by prolong follow-up durations (RR = 1.13, 95% CI: 1.03–1.22). This updated meta-analysis highlighted the pro-inflammatory diet as a risk factor for BrCa, especially among women in post-menopausal status, obese groups, and developing countries. Meta-analysis in methodological subgroups could improve results, less affected by heterogeneity, and suggested subclassification with important implications for future epidemiological designs and even clinical management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
McPherson K, Steel C, Dixon J. ABC of breast diseases: breast cancer—epidemiology, risk factors, and genetics. BMJ. 2000;321:624.
Tobias DK, Akinkuolie AO, Chandler PD, Lawler PR, Manson JE, Buring JE, et al. Markers of inflammation and incident breast cancer risk in the women’s health study. Am J Epidemiol. 2018;187:705–16.
Wang K, Karin M Tumor-elicited inflammation and colorectal cancer. Adv Cancer Res. 128: Elsevier; 2015. p. 173-96.
Macciò A, Madeddu C. Inflammation and ovarian cancer. Cytokine. 2012;58:133–47.
Aggarwal BB, Vijayalekshmi R, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15:425–30.
Multhoff G, Molls M, Radons J. Chronic inflammation in cancer development. Front Immunol. 2012;2:98.
Sollie S, Michaud DS, Sarker D, Karagiannis SN, Josephs DH, Hammar N, et al. Chronic inflammation markers are associated with risk of pancreatic cancer in the Swedish AMORIS cohort study. BMC Cancer. 2019;19:1–6.
van’t Klooster CC, Ridker PM, Hjortnaes J, van Der Graaf Y, Asselbergs FW, Westerink J, et al. The relation between systemic inflammation and incident cancer in patients with stable cardiovascular disease: a cohort study. Eur Heart J. 2019;40:3901–9.
Demb J, Wei EK, Izano M, Kritchevsky S, Swede H, Newman AB, et al. Chronic inflammation and risk of lung cancer in older adults in the health, aging and body composition cohort study. J Geriatr Oncol. 2019;10:265–71.
Taams LS. Inflammation and immune resolution. Clin Exp Immunol. 2018;193:1–2.
Perwez Hussain S, Harris CC. Inflammation and cancer: an ancient link with novel potentials. Int J Cancer. 2007;121:2373–80.
Jiang X, Shapiro DJ. The immune system and inflammation in breast cancer. Mol Cell Endocrinol. 2014;382:673–82.
Bhatelia K, Singh K, Singh R. TLRs: linking inflammation and breast cancer. Cell Signal. 2014;26:2350–7.
Cevenini E, Caruso C, Candore G, Capri M, Nuzzo D, Duro G, et al. Age-related inflammation: the contribution of different organs, tissues and systems. How to face it for therapeutic approaches. Curr Pharm Des. 2010;16:609–18.
Ferrante A Jr. Obesity‐induced inflammation: a metabolic dialogue in the language of inflammation. J Intern Med. 2007;262:408–14.
Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J Am Coll Cardiol. 2004;44:152–8.
Barbaresko J, Koch M, Schulze MB, Nöthlings U. Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev. 2013;71:511–27.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17:1689–96.
Jang H, Chung M, Kang S, Park Y. Association between the dietary inflammatory index and risk for cancer recurrence and mortality among patients with breast cancer. Nutrients 2018;10:1095.
Huang W-Q, Mo X-F, Ye Y-B, Shivappa N, Lin F-Y, Huang J, et al. A higher Dietary Inflammatory Index score is associated with a higher risk of breast cancer among Chinese women: a case–control study. Br J Nutr. 2017;117:1358–67.
Ge I, Rudolph A, Shivappa N, Flesch-Janys D, Hebert JR, Chang-Claude J. Dietary inflammation potential and postmenopausal breast cancer risk in a German case-control study. Breast. 2015;24:491–6.
Zucchetto A, Serraino D, Shivappa N, Hébert JR, Stocco C, Puppo A, et al. Dietary inflammatory index before diagnosis and survival in an Italian cohort of women with breast cancer. Br J Nutr. 2017;117:1456–62.
Shivappa N, Sandin S, Löf M, Hébert JR, Adami H-O, Weiderpass E. Prospective study of dietary inflammatory index and risk of breast cancer in Swedish women. Br J Cancer. 2015;113:1099.
Shivappa N, Blair CK, Prizment AE, Jacobs DR, Hébert JR. Prospective study of the dietary inflammatory index and risk of breast cancer in postmenopausal women. Mol Nutr Food Res. 2017;61:1600592.
Tabung FK, Steck SE, Liese AD, Zhang J, Ma Y, Johnson KC, et al. Patterns of change over time and history of the inflammatory potential of diet and risk of breast cancer among postmenopausal women. Breast Cancer Res Treat. 2016;159:139–49.
Tabung FK, Steck SE, Liese AD, Zhang J, Ma Y, Caan B, et al. Association between dietary inflammatory potential and breast cancer incidence and death: results from the Women’s Health Initiative. Br J Cancer. 2016;114:1277.
Shivappa N, Hébert JR, Rosato V, Montella M, Serraino D, La Vecchia C. Association between the dietary inflammatory index and breast cancer in a large Italian case–control study. Mol Nutr Food Res. 2017;61:1600500.
Wang L, Liu C, Zhou C, Zhuang J, Tang S, Yu J, et al. Meta-analysis of the association between the dietary inflammatory index (DII) and breast cancer risk. Eur J Clin Nutr. 2019;73:509–17.
Jayedi A, Emadi A, Shab-Bidar S. Dietary inflammatory index and site-specific cancer risk: a systematic review and dose-response meta-analysis. Adv Nutr. 2018;9:388–403.
Zahedi H, Djalalinia S, Sadeghi O, Asayesh H, Noroozi M, Gorabi AM, et al. Dietary inflammatory potential score and risk of breast cancer: systematic review and meta-analysis. Clin Breast Cancer. 2018;18:e561–e70.
Liu Z-Y, Gao X-P, Zhu S, Liu Y-H, Wang L-J.JingC-X, et al. Dietary inflammatory index and risk of gynecological cancers: a systematic review and meta-analysis of observational studies. Gynecol Oncol. 2018;30:1–14.
Moradi S, Issah A, Mohammadi H, Mirzaei K. Associations between dietary inflammatory index and incidence of breast and prostate cancer: a systematic review and meta-analysis. Nutrition 2018;55:168–78.
Namazi N, Larijani B, Azadbakht L. Association between the dietary inflammatory index and the incidence of cancer: a systematic review and meta-analysis of prospective studies. Public Health. 2018;164:148–56.
Chen H, Gao Y, Wei N, Du K, Jia Q. Strong association between the dietary inflammatory index (DII) and breast cancer: a systematic review and meta-analysis. Aging. 2021;13:13039.
Aghababayan S, Mobarakeh ZS, Qorbani M, Tiznobeyk Z, Aminianfar A, Sotoudeh G. Higher dietary inflammatory index scores are associated with increased odds of Benign breast diseases in a case–control study. J Inflamm Res. 2020;13:61.
Gardeazabal I, Ruiz-Canela M, Sánchez-Bayona R, Romanos-Nanclares A, Aramendía-Beitia J, Shivappa N, et al. Dietary inflammatory index and incidence of breast cancer in the SUN project. Clin Nutr. 2019;38:2259–68.
Graffouillere L, Deschasaux M, Mariotti F, Neufcourt L, Shivappa N, Hébert JR, et al. The dietary inflammatory index is associated with prostate cancer risk in French middle-aged adults in a prospective study. J Nutr. 2015;146:785–91.
Jalali S, Shivappa N, Hébert JR, Heidari Z, Hekmatdoost A, Rashidkhani B. Dietary inflammatory index and odds of breast cancer in a case-control study from Iran. Nutr Cancer. 2018;70:1034–42.
Lee S, Quiambao AL, Lee J, Ro J, Lee E-S, Jung S-Y, et al. Dietary inflammatory index and risk of breast cancer based on hormone receptor status: a case-control study in Korea. Nutrients 2019;11:1949.
Niclis C, Shivappa N, Hébert JR, Tumas N, Díaz MDP. The inflammatory potential of diet is associated with breast cancer risk in urban Argentina: a multilevel analysis. Nutr Cancer. 2020;73:1–10.
Obón-Santacana M, Romaguera D, Gracia-Lavedan E, Molinuevo A, Molina-Montes E, Shivappa N, et al. Dietary inflammatory index, dietary non-enzymatic antioxidant capacity, and colorectal and breast cancer risk (MCC-Spain Study). Nutrients. 2019;11:1406.
Vahid F, Shivappa N, Hatami M, Sadeghi M, Ameri F, Naeini YJ, et al. Association between dietary inflammatory index (DII) and risk of breast cancer: a case-control study. Asian Pac J Cancer Prev. 2018;19:1215.
Wang K, Sun J-Z, Wu Q-X, Li Z-Y, Li D-X, Xiong Y-F, et al. Long-term anti-inflammatory diet in relation to improved breast cancer prognosis: a prospective cohort study. NPJ Breast Cancer. 2020;6:1–11.
Zheng J, Tabung FK, Zhang J, Liese AD, Shivappa N, Ockene JK, et al. Association between post-cancer diagnosis dietary inflammatory potential and mortality among invasive breast cancer survivors in the Women’s Health Initiative. Cancer Epidemiol Biomark Prev. 2018;27:454–63.
Park YMM, Shivappa N, Petimar J, Hodgson ME, Nichols HB, Steck SE. et al. Dietary inflammatory potential, oxidative balance score, and risk of breast cancer: findings from the Sister Study. Int J Cancer. 2021;149:615–26.
Hajji-Louati M, Cordina-Duverger E, Laouali N, Mancini F-R, Guénel P. A case–control study in France showing that a pro-inflammatory diet is associated with a higher risk of breast cancer. Sci Rep. 2021;11:1–10.
Schröder J. Face-to-Face Surveys (Version 2.0). 2016.
Shim J-S, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:1–8.
Kuo C-L, Duan Y, Grady J. Unconditional or conditional logistic regression model for age-matched case–control data? Front Public Health. 2018;6:57.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Honma S, Shimodaria K, Shimizu Y, Tsuchiya N, Saito H, Yanaihara T, et al. The influence of inflammatory cytokines on estrogen production and cell proliferation in human breast cancer cells. Endocr J. 2002;49:371–7.
Macciò A, CObesity Madeddu. inflammation, and postmenopausal breast cancer: therapeutic implications. Sci World J. 2011;11:2020–36.
Yue W, Wang JP, Li Y, Fan P, Liu G, Zhang N, et al. Effects of estrogen on breast cancer development: role of estrogen receptor independent mechanisms. Int J Cancer. 2010;127:1748–57.
Livesey G, Taylor R, Livesey HF, Buyken AE, Jenkins DJ, Augustin LS, et al. Dietary glycemic index and load and the risk of type 2 diabetes: a systematic review and updated meta-analyses of prospective cohort studies. Nutrients. 2019;11:1280.
Fowler ME, Akinyemiju TF. Meta‐analysis of the association between dietary inflammatory index (DII) and cancer outcomes. Int J Cancer. 2017;141:2215–27.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6:e1000097.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Chichester (UK); John Wiley & Sons; 2019.
Sterne JA Meta-analysis in Stata: an updated collection from the Stata Journal: StataCorp LP; 2009.
Duval S, Tweedie R. Trim and fill: a simple funnel‐plot–based method of testing and adjusting for publication bias in meta‐analysis. Biometrics. 2000;56:455–63.
Nordmann AJ, Kasenda B, Briel M. Meta-analyses: what they can and cannot do. Swiss Med Wkly. 2012;142:1–11.
Swan SH, Shaw GM, Schulman J. Reporting and selection bias in case-control studies of congenital malformations. Epidemiology. 1992;3:356–63.
Song JW, Chung KC. Observational studies: cohort and case-control studies. Plast Reconstr Surg. 2010;126:2234.
Neupane B, Walter SD, Krueger P, Loeb M. Community controls were preferred to hospital controls in a case–control study where the cases are derived from the hospital. J Clin Epidemiol. 2010;63:926–31.
Li L, Zhang M. Population versus hospital controls for case-control studies on cancers in Chinese hospitals. BMC Med Res Methodol. 2011;11:167.
Savy M, Martin-Prével Y, Traissac P, Eymard-Duvernay S, Delpeuch F. Dietary diversity scores and nutritional status of women change during the seasonal food shortage in rural Burkina Faso. J Nutr. 2006;136:2625–32.
Betensky RA. Measures of follow-up in time-to-event studies: why provide them and what should they be? Clin Trials. 2015;12:403–8.
Sun Y-S, Zhao Z, Yang Z-N, Xu F, Lu H-J, Zhu Z-Y, et al. Risk factors and preventions of breast cancer. Int J Biol Sci. 2017;13:1387.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS, et al. A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr. 2014;17:1825–33.
Capellino S, Straub RH, Cutolo M. Aromatase and regulation of the estrogen‐to‐androgen ratio in synovial tissue inflammation: common pathway in both sexes. Ann NY Acad Sci. 2014;1317:24–31.
West KM, Blacksher E, Burke W. Genomics, health disparities, and missed opportunities for the nation’s research agenda. JAMA. 2017;317:1831–2.
IntHout J, Ioannidis JP, Borm GF, Goeman JJ. Small studies are more heterogeneous than large ones: a meta-meta-analysis. J Clin Epidemiol. 2015;68:860–9.
Author information
Authors and Affiliations
Contributions
S.P. and Z.H. contributed to the conception of the study, design, data collections, statistical analysis, data interpretation, and drafting of this manuscript. M.A.J. contributed to the statistical analysis. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hayati, Z., Jafarabadi, M.A. & Pirouzpanah, S. Dietary inflammatory index and breast cancer risk: an updated meta-analysis of observational studies. Eur J Clin Nutr 76, 1073–1087 (2022). https://doi.org/10.1038/s41430-021-01039-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-021-01039-5
This article is cited by
-
Nutrition and dietary inflammatory indices of the eight major cuisines of China
BMC Nutrition (2025)
-
The impact of low dietary inflammatory index diet on clinical parameters in patients with chronic kidney disease: a retrospective comparative study
BMC Nephrology (2025)
-
A cohort study on the association of dietary inflammatory index and a posteriori dietary patterns with lung cancer risk
Scientific Reports (2025)
-
Cancer Risk and Mortality Following Substitution of Animal Foods with Plant Foods: A Systematic Review
Current Nutrition Reports (2025)
-
Non-genetic factors and breast cancer: an umbrella review of meta-analyses
BMC Cancer (2024)