Abstract
Background/objective
The complex interplay between adiposity, bone health and cardiometabolic risk (CMR) factors is unclear in Indian children. We aimed to investigate the mediating role of number of CMR factors on the relationship between fat % and bone mineral content (BMC) % in South Indian children aged 5–16 years.
Subjects and methods
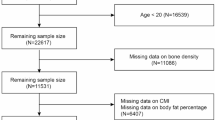
Healthy children (n = 317), from India, underwent anthropometric, blood biochemistry, blood pressure, along with body composition and BMC assessments using Dual-energy X-ray absorptiometry. Based on the number of CMR factors, children were categorised into three groups: 0, 1 and ≥ 2. Analysis of variance was used to compare the parameters between the CMR groups and mediation analysis was performed to examine if the number of CMR factors mediated the relationship between fat % and BMC %.
Results
The prevalence of 0, 1 and ≥ 2 CMR factors was 42.3%, 33.9% and 23.9% respectively; mean BMC % was lowest in ≥ 2 CMR group. In the whole group, BMC % had significant negative correlation with fat % (r = −0.68, p < 0.0001) and positive correlation with lean % (r = 0.64, p < 0.0001). Adjusted for age and sex, results suggested significant mediating effect of number of CMR factors on the relationship between fat % and BMC % (Average Causal Mediation Effects =−0.002, bootstrapped 95% CI: −0.0039, −0.0001, p < 0.01), but losing significance when adjusted for co-variates.
Conclusion
Number of CMR factors mediates the relationship between fat % and BMC % in Indian children. Further studies are needed to confirm these findings, understand mechanisms and plan appropriate strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Additional data can be made available from the corresponding author on reasonable request.
Change history
04 December 2024
The original online version of this article was revised. In the ‘Statistical Methods’ section, the sentence “Comparison of BMC % between three CMR groups stratified by various ranges of fat %, android fat %, gynoid fat % (<20, 21–30, 31–50 and >40) and waist-to-height ratio (WHtR) cutoff were performed using ANOVA” was corrected to read “Comparison of BMC % between three CMR groups stratified by various ranges of fat %, android fat %, gynoid fat % (<20, 21–30, 31–40 and >40) and waist-to-height ratio (WHtR) cutoff were performed using ANOVA.”
12 December 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41430-024-01553-2
References
Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Fam Med Prim Care. 2015;4:187.
Kansra AR, Lakkunarajah S, Jay MS. Childhood and adolescent obesity: a review. Front Pediatr. 2021;8:866.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obes Rev. 2016;17:95–107.
Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT. et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc Health. Lancet Child Adolesc Health. 2022;6:158–70.
Oza C, Khadilkar V, Karguppikar M, Ladkat D, Gondhalekar K, Shah N, et al. Prevalence of metabolic syndrome and predictors of metabolic risk in Indian children, adolescents and youth with type 1 diabetes mellitus. Endocrine. 2022;75:794–803.
Gupta A, Sachdeva A, Mahajan N, Gupta A, Sareen N, Pandey RM, et al. Prevalence of pediatric metabolic syndrome and associated risk factors among school-age children of 10–16 years living in District Shimla, Himachal Pradesh, India. Indian J Endocrinol Metab. 2018;22:373.
Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF and Population Council. (2019). Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi.
Sachdev HS, Porwal A, Sarna A, Acharya R, Ramesh S, Kapil U, et al. Intraindividual double-burden of anthropometric undernutrition and “metabolic obesity” in Indian children: a paradox that needs action. Eur J Clin Nutr. 2021;75:1205–17.
Babhulkar S, Seth S. Prevalence of osteoporosis in India: an observation of 31238 adults. Int J Res Orthop. 2021;7:362–8.
Khinda R, Valecha S, Kumar N, Walia JP, Singh K, Sethi S, et al. Prevalence and predictors of osteoporosis and osteopenia in postmenopausal women of Punjab, India. Int J Environ Res Public Health. 2022;19:2999.
Sopher AB, Fennoy I, Oberfield SE. An update on childhood bone health: mineral accrual, assessment, and treatment. Curr Opin Endocrinol Diab Obes 2015;22:35.
Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46:294–305.
Wey HE, Binkley TL, Beare TM, Wey CL, Specker BL. Cross-sectional versus longitudinal associations of lean and fat mass with pQCT bone outcomes in children. J Clin Endocrinol Metab. 2011;96:106–14.
Pollock NK. Childhood obesity, bone development, and cardiometabolic risk factors. Mol Cell Endocrinol. 2015;410:52–63.
Goulding A, Grant AM, Williams SM. Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Miner Res. 2005;20:2090–6.
Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res® 2013;471:1199–207.
Heaney RP. Bone mineral content, not bone mineral density, is the correct bone measure for growth studies. Am J Clin Nutr 2003;78:350–1.
Koo HC, Lim GP, Kaur S, Chan KQ, Chan KE, Chung C, et al. Bone health and its positive relationships with body composition in Malaysian schoolchildren: findings from a cross-sectional study. Children 2021;8:569.
Zhang L, Li H, Zhang Y, Kong Z, Zhang T, Zhang Z. Association of body compositions and bone mineral density in chinese children and adolescents: compositional data analysis. BioMed Res Int. 2021;2021:1904343.
Khadilkar A, Chiplonkar S, Agrawal DP, Sanwalka N, Khadilkar V. Bone health status in Indian overweight/obese children. Indian J Pediatr. 2016;83:1473–5.
Dimitri P. Fat and bone in children–where are we now? Ann Pediatr Endocrinol Metab. 2018;23:62.
Hetherington-Rauth M, Bea JW, Blew RM, Funk JL, Lee VR, Varadi TC, et al. Effect of cardiometabolic risk factors on the relationship between adiposity and bone mass in girls. Int J Obes. 2018;42:1185–94.
Pollock NK, Bernard PJ, Gutin B, Davis CL, Zhu H, Dong Y. Adolescent obesity, bone mass, and cardiometabolic risk factors. J Pediatr. 2011;158:727–34.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY, US: Guilford Press; 2013.
Soares MJ, Calton EK, Pathak K, Zhao Y. Hypothesized pathways for the association of vitamin D status and insulin sensitivity with resting energy expenditure: a cross sectional mediation analysis in Australian adults of European ancestry. Eur J Clin Nutr. 2022;76:1457–63.
Lakshmi S, Metcalf B, Joglekar C, Yajnik CS, Fall CH, Wilkin TJ. Differences in body composition and metabolic status between white UK and Asian Indian children (EarlyBird 24 and the Pune Maternal Nutrition Study). Pediatr Obes. 2012;7:347–54.
D’Angelo S, Yajnik CS, Kumaran K, Joglekar C, Lubree H, Crozier SR, et al. Body size and body composition: a comparison of children in India and the UK through infancy and early childhood. J Epidemiol Community Health. 2015;69:1147–53.
Bharathi AV, Kurpad AV, Thomas T, Yusuf S, Saraswathi G, Vaz M. Development of food frequency questionnaires and a nutrient database for the Prospective Urban and Rural Epidemiological (PURE) pilot study in South India: methodological issues. Asia Pac J Clin Nutr. 2008;17:178–85.
Swaminathan S, Selvam S, Thomas T, Kurpad AV, Vaz M. Longitudinal trends in physical activity patterns in selected urban south Indian school children. Indian J Med Res. 2011;134:174–80.
Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual, Human Kinetics Books, 1988.
World Health Organization, BMI-for-age (5–19 years). [cited on July 14, 2022]. Available from, https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series Geneva: WHO; 1995.
Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73:e35–66.
Kuriyan R, Thomas T, Lokesh DP, Sheth NR, Mahendra A, Joy R, et al. Waist circumference and waist for height percentiles in urban South Indian children aged 3–16 years. Indian Pediatr. 2011;48:765–71.
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128:S213–56.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
World Health Organization. Nutrition in adolescence. Issues and challenges for the health sector. Discussion paper Geneva: WHO, 2005.
Martin RL, Perez E, He YJ, Dawson R, Millard WJ. Leptin resistance is associated with hypothalamic leptin receptor mRNA and protein downregulation. Metab Clin Exp. 2000;49:1479–84.
Hetherington-Rauth M, Bea JW, Blew RM, Funk JL, Lee VR, Roe DJ, et al. Relationship of cardiometabolic risk biomarkers with DXA and pQCT bone health outcomes in young girls. Bone. 2019;120:452–8.
Pollock NK, Bernard PJ, Wenger K, Misra S, Gower BA, Allison JD, et al. Lower bone mass in prepubertal overweight children with prediabetes. J Bone Min Res. 2010;2512:2760–9.
Witkowska-Sędek E, Pyrżak B. Chronic inflammation and the growth hormone/insulin-like growth factor-1 axis. Cent Eur J Immunol. 2020;45:469–75.
Yuan S, Wan ZH, Cheng SL, Michaëlsson K, Larsson SC. Insulin-like growth factor-1, bone mineral density, and fracture: a Mendelian randomization study. J Clin Endocrinol Metab. 2021;106:1552–8.
Misra A, Shrivastava U. Obesity and dyslipidemia in South Asians. Nutrients. 2013;5:2708–33.
Iyengar SS, Puri R, Narasingan SN. Lipid Association of India expert consensus statement on management of dyslipidemia in Indians 2016-part 1. J Prim Care Spec. 2016;2:134–5.
Misra A, Wasir JS, Vikram NK. Carbohydrate diets, postprandial hyperlipidaemia, abdominal obesity & Asian Indians: a recipe for atherogenic disaster. Indian J Med Res. 2005;121:5.
Berg AH, Scherer PE. Adipose tissue, inflammation, and cardiovascular disease. Circ Res. 2005;96:939–49.
Magni P, Dozio E, Galliera E, Ruscica M, Corsi MM. Molecular aspects of adipokine-bone interactions. Curr Mol Med. 2010;10:522–32.
Acknowledgements
The authors acknowledge Jayakumar Joseph and the entire study team for their involvement in data collection. We are grateful to all the children who participated in the study.
Funding
The study was supported by the International Atomic Energy Agency (IAEA), Vienna.
Author information
Authors and Affiliations
Contributions
SAF: data analysis and prepared the different versions of the manuscript. PS: helped in data analysis and contributed to preparing the drafts of the manuscript. SS: performed statistical analysis, interpretation of findings and reviewed the draft. DP: was involved in conducting the research and reviewing the manuscript. JA: was involved in the data collection and reviewed the manuscript. RK: conceptualized, designed and supervised the research, interpretation of results, critically reviewed and edited the draft and has primary responsibility for the final content. Each author had participated sufficiently in the work to take public responsibility of appropriate portions of the content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was obtained from the St John’s Medical College Institutional Ethical committee (reference no.84/2011). Date of approval: Study was approved on 7th July 2011. Informed written consent was obtained from parents and oral assent was obtained from children >10 years of age.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41430_2024_1494_MOESM1_ESM.docx
Comparison of BMC % between the number of CMR factors stratified by various fat ranges of total fat %, regional fat % distribution and waist-to-height ratio
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farheen, S.A., S, P., Selvam, S. et al. Do cardiometabolic risk factors mediate the relationship between body composition and bone mineral content in South Indian children aged 5 to 16 years?. Eur J Clin Nutr 78, 1014–1021 (2024). https://doi.org/10.1038/s41430-024-01494-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-024-01494-w