Abstract
Background
The long-term effects of breakfast on childhood z-BMI remain inconclusive.
Objective
To prospectively assess the impact of stable and altered breakfast consumption habits on z-BMI change over two years, in school-aged children across six European countries.
Methods
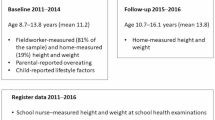
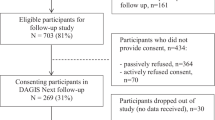
Data of 6,528 children (8.2 ± 1.0 years, 48.9% male) from the Feel4Diabetes study were used. Children’s lifestyle behaviors, including breakfast frequency, were assessed through parent‐reported questionnaires. Weight and height were objectively measured and converted to z-BMI. Participants were categorized into trajectories combining breakfast consumption habit (i.e., regular consumption, irregular consumption or omission) at baseline and follow up. Logistic regression analyzed the prospective association between breakfast trajectories and z-BMI increase, with adjustment for demographic and lifestyle variables.
Results
A statistically significant effect of breakfast trajectories was observed in z-BMI, both at baseline and follow up. Stable skippers was the only trajectory that showed a significant increase in BMI z-score from baseline to follow up (0.891 ± 1.058 vs. 1.034 ± 1.072 respectively, p < 0.05). BMI z-score at follow up of regular eaters (0.615 ± 0.967) was significantly lower, compared to both irregular eaters (1.229 ± 0.890) and stable skippers (both p < 0.05). Stable regular consumption and transition from omission to regular consumption were independently associated with significantly lower risk of z-BMI gain, compared to stable omission [OR, 95% CI: 0.55 (0.31, 0.97), p = 0.039 and 0.43 (0.21, 0.88), p = 0.021 respectively].
Conclusion
Stable regular breakfast consumption or transition from omission to regular consumption seem to contribute to superior weight regulation in children and to independently protect against z-BMI gain, compared to stable omission. Further studies are warranted to extend the evidence on the breakfast habit-BMI association among children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The original data of this work are available upon reasonable request to the corresponding author.
References
Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med 2019; 17 https://doi.org/10.1186/s12916-019-1449-8.
World Health Organization. Obesity and overweight. Fact Sheet, 2024. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
World Health Organization. WHO European Regional Obesity Report 2022. World Health Organization. Regional Office for Europe: Copenhagen, 2022. https://iris.who.int/handle/10665/353747.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8.
van de Pas KGH, de Krom MAP, Winkens B, van Dielen FMH, Vreugdenhil ACE. Health-related quality of life in children and adolescents with overweight, obesity, and severe obesity: a cross-sectional study. Obes Facts. 2023;16:282–92.
Smith JD, Fu E, Kobayashi MA. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu Rev Clin Psychol. 2020;16:351–78.
Zolotarjova J, ten Velde G, Vreugdenhil ACE. Effects of multidisciplinary interventions on weight loss and health outcomes in children and adolescents with morbid obesity. Obes Rev. 2018;19:931–46.
Coles N, Birken C, Hamilton J. Emerging treatments for severe obesity in children and adolescents. BMJ. 2016;354:i4116.
Kim J, Lim H. Nutritional management in childhood obesity. J Obes Metab Syndr. 2019;28:225–35.
O’Neil CE, Byrd-Bredbenner C, Hayes D, Jana L, Klinger SE, Stephenson-Martin S. The role of breakfast in health: definition and criteria for a quality breakfast. J Acad Nutr Diet. 2014;114:S8–26.
Sandercock GRH, Voss C, Dye L. Associations between habitual school-day breakfast consumption, body mass index, physical activity and cardiorespiratory fitness in English schoolchildren. Eur J Clin Nutr. 2010;64:1086–92.
Ptomey LT, Steger FL, Schubert MM, Lee J, Willis EA, Sullivan DK, et al. Breakfast intake and composition is associated with superior academic achievement in elementary school children. J Am Coll Nutr. 2016;35:326–33.
Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr. 2010;92:1316–25.
Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: A meta-analysis. Prev Med. 2011;53:260–7.
Blondin SA, Anzman-Frasca S, Djang HC, Economos CD. Breakfast consumption and adiposity among children and adolescents: an updated review of the literature. Pediatr Obes. 2016;11:333–48.
Wang K, Niu Y, Lu Z, Duo B, Effah CY, Guan L The effect of breakfast on childhood obesity: a systematic review and meta-analysis. Front Nutr 2023; 10. https://doi.org/10.3389/fnut.2023.1222536.
Szajewska H, Ruszczyński M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr. 2010;50:113–9.
Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. 2005;105:743–60.
Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014;100:539–47.
Vereecken C, Group the HE& DF, Dupuy M, Rasmussen M, Kelly C, Nansel TR, et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health. 2009;54:180–90.
Utter J, Scragg R, Schaaf D, Fitzgerald E, Wilson N. Correlates of body mass index among a nationally representative sample of New Zealand children. Int J Pediatr Obes. 2007;2:104–13.
Patro B, Szajewska H. Meal patterns and childhood obesity. Curr Opin Clin Nutr Metab Care. 2010;13:300–4.
Delva J, O’Malley PM, Johnston LD. Racial/ethnic and socioeconomic status differences in overweight and health-related behaviors among American students: National trends 1986–2003. J Adolesc Health. 2006;39:536–45.
Monzani A, Ricotti R, Caputo M, Solito A, Archero F, Bellone S, et al. A systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients. 2019;11:387.
Siega-Riz AM, Popkin BM, Carson T. Trends in breakfast consumption for children in the United States from 1965–1991. Am J Clin Nutr. 1998;67:748S–756S.
de la Hunty A, Gibson S, Ashwell M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obes Facts. 2013;6:70–85.
Ardeshirlarijani E, Namazi N, Jabbari M, Zeinali M, Gerami H, Jalili RB, et al. The link between breakfast skipping and overweigh/obesity in children and adolescents: a meta-analysis of observational studies. J Diabetes Metab Disord. 2019;18:657–64.
Wijtzes AI, Jansen W, Bouthoorn SH, van Lenthe FJ, Franco OH, Hofman A, et al. Meal-skipping behaviors and body fat in 6-year-old children. J Pediatr. 2016;168:118–25.e2.
Tin SPP, Ho SY, Mak KH, Wan KL, Lam TH. Breakfast skipping and change in body mass index in young children. Int J Obes (Lond). 2011;35:899–906.
Manios Y, Androutsos O, Lambrinou C-P, Cardon G, Lindstrom J, Annemans L, et al. A school- and community-based intervention to promote healthy lifestyle and prevent type 2 diabetes in vulnerable families across Europe: design and implementation of the Feel4Diabetes-study. Public Health Nutr. 2018;21:3281–90.
Anastasiou CA, group F, Fappa E, Zachari K, Mavrogianni C, et al. Development and reliability of questionnaires for the assessment of diet and physical activity behaviors in a multi-country sample in Europe the Feel4Diabetes Study. BMC Endocr Disord 2020; 20. https://doi.org/10.1186/s12902-019-0469-x.
Androutsos O, group on behalf of the F, Anastasiou C, Lambrinou CP, Mavrogianni C, Cardon G, et al. Intra- and inter- observer reliability of anthropometric measurements and blood pressure in primary schoolchildren and adults: the Feel4Diabetes-study. BMC Endocr Disord 2020; 20. https://doi.org/10.1186/s12902-020-0501-1.
Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatr Obes. 2012;7:284–94.
Kelly Y, Patalay P, Montgomery S, Sacker A. BMI development and early adolescent psychosocial well-being: UK Millennium Cohort Study. Pediatrics 2016; 138. https://doi.org/10.1542/peds.2016-0967.
Traub M, Boat” the RG “Join the H, Lauer R, Kesztyüs T, Wartha O, Steinacker JM, et al. Skipping breakfast, overconsumption of soft drinks and screen media: longitudinal analysis of the combined influence on weight development in primary schoolchildren. BMC Public Health 2018; 18. https://doi.org/10.1186/s12889-018-5262-7.
Tin SPP, Ho SY, Mak KH, Wan KL, Lam TH. Location of breakfast consumption predicts body mass index change in young Hong Kong children. Int J Obes. 2012;36:925–30.
Drenowatz C, Kobel S, Kettner S, Kesztyüs D, Wirt T, Dreyhaupt J, et al. Correlates of weight gain in German children attending elementary school. Prev Med. 2013;57:310–4.
Shang X, Li Y, Xu H, Zhang Q, Hu X, Liu A, et al. Healthy breakfast habits and changes in obesity-related cardiometabolic markers in children: a longitudinal analysis. Eur J Clin Nutr. 2020;74:1685–97.
MacFarlane A, Cleland V, Crawford D, Campbell K, Timperio A. Longitudinal examination of the family food environment and weight status among children. Int J Pediatr Obes. 2009;4:343–52.
Albertson AM, Franko DL, Thompson D, Eldridge AL, Holschuh N, Affenito SG, et al. Longitudinal patterns of breakfast eating in black and white adolescent girls. Obesity. 2007;15:2282–92.
Gingras V, Rifas-Shiman SL, Taveras EM, Oken E, Hivert M-F. Dietary behaviors throughout childhood are associated with adiposity and estimated insulin resistance in early adolescence: a longitudinal study. Int J Behav Nutr Phys Act 2018; 15. https://doi.org/10.1186/s12966-018-0759-0.
Hassan BK, Cunha DB, da Veiga GV, Pereira RA, Hoffman DJ, Sichieri R. Breakfast consumption, family breakfast, and adiposity trajectory in adolescence—the adolescent nutritional assessment longitudinal cohort study. J Acad Nutr Diet. 2019;119:944–56.
Haerens L, Vereecken C, Maes L, De Bourdeaudhuij I. Relationship of physical activity and dietary habits with body mass index in the transition from childhood to adolescence: a 4-year longitudinal study. Public Health Nutr. 2010;13:1722–8.
Tee ES, Nurliyana AR, Norimah AK, Hjbj M, Tan SY, Appukutty M, et al. Breakfast consumption among Malaysian primary and secondary school children and relationship with body weight status - Findings from the MyBreakfast Study. Asia Pac J Clin Nutr. 2018; 27. https://doi.org/10.6133/apjcn.062017.12.
Yaguchi-Tanaka Y, Tabuchi T. Skipping breakfast and subsequent overweight/obesity in children: A nationwide prospective study of 2.5- to 13-year-old children in Japan. J Epidemiol. 2021;31:417–25.
Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971-2004. JAMA. 2006;295:2385–93.
Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics. 2008;121:e638–45.
Wijtzes AI, Jansen W, Jaddoe VWV, Franco OH, Hofman A, van Lenthe FJ, et al. Social inequalities in young children’s meal skipping behaviors: The Generation R study. PLoS One. 2015;10:e0134487.
Qorbani M, Kasaeian A, Rafiemanzelat A-M, Sheidayi A, Djalalinia S, Nouri K, et al. Social inequalities in meal skipping patterns among children and adolescents: The CASPIAN-V study. Obes Sci Pract. 2021;7:690–8.
Küpers LK, de Pijper JJ, Sauer PJJ, Stolk RP, Corpeleijn E. Skipping breakfast and overweight in 2- and 5-year-old Dutch children-the GECKO Drenthe cohort. Int J Obes. 2013;38:569–71.
Alsharairi NA, Somerset SM. Skipping breakfast in early childhood and its associations with maternal and child BMI: a study of 2-5-year-old Australian children. Eur J Clin Nutr. 2015;70:450–5.
Dubois L, Girard M, Potvin Kent M, Farmer A, Tatone-Tokuda F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among pre-school children. Public Health Nutr. 2008;12:19–28.
Neuhouser ML, Lilley S, Lund A, Johnson DB. Development and validation of a beverage and snack questionnaire for use in evaluation of school nutrition policies. J Am Diet Assoc. 2009;109:1587–92.
Willett W. Food frequency methods. In: Nutritional Epidemiology Oxford University Press; 2012. p. 70–95.
Funding
The Feel4Diabetes study has received funding from the European Union’s Horizon 2020 research and innovation program [Grant Agreement: n° 643708]. The content of this article reflects only the authors’ views and the European Community is not liable for any use that may be made of the information contained therein. The funding body had no role in the design of this study and collection, analysis, and interpretation of the data, and in writing this manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
PK acquired data and drafted the manuscript. CAA contributed in the design of the work and in the interpretation of the results, acquired data and drafted the manuscript. EK contributed in the design and in the interpretation of the results and revised the manuscript. VI, IR, SL, LAM, JL, KW, GC, KM and YM conceived the work and revised the manuscript. NU, TT and NGL acquired data and revised the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted conforming to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were granted approval by the human bioethics committees of all of the participating tertiary institutions [Medical Ethics Committee of the Ghent University Hospital, Belgium (Ethical Approval (EA) No.: B670201524237; 21/04/15); Ethics Committee of the Medical University of Varna, Bulgaria (EA No.: 52/10-3-2016; 10/03/16) and the Municipalities of Sofia and Varna, as well as the Ministry of Education and Science local representatives; Hospital district of Southwest Finland ethical committee (EA: No.: 174/1801/2015; 13/03/15); Bioethics Committee of Harokopio University, Greece and the Greek Ministry of Education; (EA No.: 46/3-4-2015; 03/04/15); National Committee for Scientific Research in Medicine, Hungary (EA No.: 20095/2016/EKU; 29/03/16); Clinical Research Ethics Committee and the Department of Consumers´ Health of the Government of Aragón, Spain (EA No.: CP03/2016; 08/04/15)]. All participants gave signed informed consent before inclusion into the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kostarellou, P., Anastasiou, C.A., Karaglani, E. et al. Prospective association between breakfast consumption frequency and BMI z-score among European school-aged children. The Feel4Diabetes Study. Eur J Clin Nutr 79, 427–434 (2025). https://doi.org/10.1038/s41430-025-01570-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01570-9