Abstract
Objectives
This study aimed to assess and compare the Institute of Medicine (IOM) guidelines and the recently published China guidelines regarding their applicability for gestational weight gain (GWG) management among Chinese pregnant women.
Method
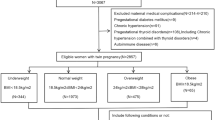
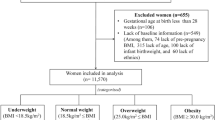
Data were extracted from the Electronic Medical Record System of Zhoushan, China. Adverse outcomes include small for gestational age (SGA), large for gestational age (LGA), low birth weight and macrosomia. GWG were estimated by the China and IOM GWG guidelines, respectively. Multiple logistical regression models were used to analyze the associations of GWG with outcomes. The modified guidelines were developed.
Results
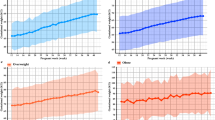
Among 9975 pregnant women without comorbidities (i.e., gestational diabetes mellitus and pregnancy-induced hypertension), comparing women with normal GWG in both guideline, those with insufficient GWG in the IOM guidelines but normal GWG in the China guidelines were more likely to delivery infants with SGA (aOR = 1.38; 95% CI: 1.07, 1.79); while those with normal GWG in the IOM guidelines but excessive GWG in the China guidelines had an increased risk of LGA (aOR = 1.49; 95% CI: 1.12, 1.98) and macrosomia (aOR = 1.70; 95% CI: 1.11, 2.60). Similar results weren’t observed among 4438 pregnant women with comorbidities. The modified guidelines were developed by combining the weekly GWG targets from the IOM (bottom values) and the China guidelines (upper values). The modified guidelines with Chinese BMI cut-off points exhibited the highest sensitivity for all adverse outcomes.
Conclusion
The China guidelines would better recognize pregnant women at risk of LGA and macrosomia but overlook a subgroup of women at risk of SGA, as recognized by the IOM guidelines. These disparities emphasized neither guidelines may be entirely suitable for GWG management in China. The modified guideline would be more appropriate for Chinese pregnant women, but further validation through research is needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All datasets generated during and analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Champion ML, Harper LM. Gestational weight gain: update on outcomes and interventions. Curr Diab Rep. 2020;20:11.
Rasmussen KM, Yaktine AL (eds). Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009.
Cheikh Ismail L, Bishop DC, Pang R, Ohuma EO, Kac G, Abrams B, et al. Gestational weight gain standards based on women enrolled in the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project: a prospective longitudinal cohort study. BMJ. 2016;352:i555.
Kac G, Carilho TRB, Rasmussen KM, Reichenheim ME, Farias DR, Hutcheon JA, et al. Gestational weight gain charts: results from the Brazilian Maternal and Child Nutrition Consortium. Am J Clin Nutr. 2021;113:1351–60.
Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317:2207–25.
Goldstein RF, Abell SK, Ranasinha S, Misso ML, Boyle JA, Harrison CL, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018;16:153.
Zheng W, Huang W, Zhang L, Tian Z, Yan Q, Wang T, et al. Suggested gestational weight gain for Chinese women and comparison with institute of medicine criteria: a large population-based study. Obes Facts. 2021;14:1–9.
Jiang X, Liu M, Song Y, Mao J, Zhou M, Ma Z, et al. The Institute of Medicine recommendation for gestational weight gain is probably not optimal among non-American pregnant women: a retrospective study from China. J Matern Fetal Neonatal Med. 2019;32:1353–8.
Arora P, Tamber Aeri B. Gestational Weight Gain among Healthy Pregnant Women from Asia in Comparison with Institute of Medicine (IOM) Guidelines-2009: a systematic review. J Pregnancy. 2019;2019:3849596.
Huang X, Tan H, Cai M, Shi T, Mi C, Lei J. Gestational weight gain in Chinese women - results from a retrospective cohort in Changsha, China. BMC Pregnancy Childbirth. 2018;18:185.
Chinese Nutrition Society. Weight monitoring and evaluation during pregnancy period of Chinese women. http://www.nhc.gov.cn/fzs/s7848/202208/2c1c388fcd0c47c58630e5f971ebb468/files/3e00de62d92749fbbe749427a5ab75ef.pdf
He J, Hu K, Wang B, Wang H. Effects of women with gestational diabetes mellitus related weight gain on pregnancy outcomes and its experiences in weight management programs: a mixed-methods systematic review. Front Endocrinol. 2023;14:1247604.
Jiang W, Mo M, Si S, Wu J, Pu L, Huang M, et al. Association of hypertensive disorders of pregnancy with infant growth in the first 36 months of life. Eur J Pediatr. 2022;181:133–41.
Peng Z, Si S, Cheng H, Zhou H, Chi P, Mo M, et al. The Associations of Maternal Hemoglobin Concentration in different time points and its changes during pregnancy with birth weight outcomes. Nutrients. 2022;14:2542.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253.
Zhou B.Coorperative Meta-Analysis Group Of Working Group On Obesity In C. [Prospective study for cut-off points of body mass index in Chinese adults]. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23:431–4.
Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Guideline of preconception and prenatal care. Zhonghua Fu Chan Ke Za Zhi. 2018;53:7–13.
International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82.
Hypertensive Disorders in Pregnancy Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association. Diagnosis and treatment of hypertension and pre-eclampsia in pregnancy: a clinical practice guideline in China. Zhonghua Fu Chan Ke Za Zhi. 2020;55:227–38.
National Health Commission of the People’s Republic of China. Growth standard for newborns by gestational age. 2022. http://www.nhc.gov.cn/wjw/fyjk/202208/d6dcc281e9b74db88dc972b34cbd3ec7.shtml
Minschart C, Lammertyn A, Van Crombrugge P, Moyson C, Verhaeghe J, Vandeginste S, et al. Low gestational weight gain in women with gestational diabetes is safe with better metabolic profile postpartum. J Clin Endocrinol Metab. 2023;108:665–79.
Zheng W, Huang W, Liu C, Yan Q, Zhang L, Tian Z, et al. Weight gain after diagnosis of gestational diabetes mellitus and its association with adverse pregnancy outcomes: a cohort study. BMC Pregnancy Childbirth. 2021;21:216.
Bogdanet D, Mustafa M, Khattak A, Shea PMO, Dunne FP. Atlantic DIP: is weight gain less than that recommended by IOM safe in obese women with gestational diabetes mellitus? Int J Obes. 2021;45:1044–51.
Su L, Zhang Y, Chen C, Lu L, Sutton D, D’Alton M, et al. Gestational weight gain and mode of delivery by the class of obesity: a meta-analysis. Obes Rev. 2022;23:e13509.
Wong T, Barnes RA, Ross GP, Cheung NW, Flack JR. Are the Institute of Medicine weight gain targets applicable in women with gestational diabetes mellitus? Diabetologia. 2017;60:416–23.
Farias DR, Carrilho TRB, Rasmussen KM, Hutcheon JA, Reichenheim ME, Barros DC, et al. Comparison between the Brazilian and 3 international gestational weight gain charts. Am J Clin Nutr. 2022;116:1157–67.
Acknowledgements
We extend our deepest gratitude to all participants and their families and thank the medical staffs for their works.
Funding
The authors acknowledge the financial support from the National Key Research and Development Programme of China (grant number 2021YFC2701901 and 2022YFC2703505); the 4+X Clinical Research Project of Women’s Hospital, School of Medicine, Zhejiang University (ZDFY2021-4X104); Major research and development projects of Zhejiang science and Technology Department (grant number 2018C03010); Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province (grant number 2020E10004); and Leading Innovative and Entrepreneur Team Introduction Pro-gram of Zhejiang (grant number 2019R01007).
Author information
Authors and Affiliations
Contributions
All authors have seen and approved the final version of the manuscript. L.H., Y.H., and Y.Y. conceived the designed and study. P.C., Y.Z. and X.A. completed the data analyses. H.C. and H.Z. interpreted the results. P.C., H.C., Y.Q., L.Z. and D.A. took part in the study design and data collection. ZP, S.S., D.C. and H.L. took part in the study design and supervised field investigation. L.H and Y.H. drafted the manuscript which revised by Y.Y.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to publish
All of the authors have read and approved the publication of the paper.
Ethics approval and consent to participate
This study protocol was approved by the institutional review board of Zhejiang University School of Medicine (No. 2011-1-002). This study conformed to the principles of the declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, L., Huang, Y., Chi, P. et al. The effects of China-recommended gestational weight gain guidelines and the Institute of Medicine guidelines on adverse birth outcomes: A population- based cohort study. Eur J Clin Nutr 79, 667–675 (2025). https://doi.org/10.1038/s41430-025-01576-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01576-3