Abstract
Background/Objectives
Predictive equations estimate post-bariatric surgery resting energy expenditure (REE), but lack accuracy assessment, especially for the remaining body mass. This study aimed to evaluate the agreement between indirect calorimetry and REE predictive methods.
Subjects/Methods
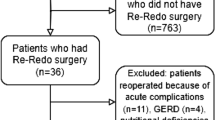
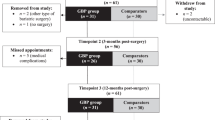
It enrolled 226 females [median age 43.0 (36.2; 50.4) years] who underwent mid- to long-term post-Roux-en-Y gastric bypass [median postoperative time 6.1 (4.0; 9.0) years]. The measured REE (mREE) was obtained using indirect calorimetry, while the estimated REE (eREE) was derived from 18 predictive equations and an artificial neural network model. Analyses were performed for the total sample and body mass index (BMI) subgroups (<30 kg/m² and ≥30 kg/m²). eREE within ±10% of mREE was considered accurate; Bland–Altman plots were performed to evaluate agreement.
Results
In the BMI < 30 kg/m² subgroup [n = 115; 1372 ± 153 kcal (5744.3 ± 640.6 kJ)], mREE did not differ from four predictive equations; Henry [1371 ± 95 kcal (5740.1 ± 397.8 kJ), p = 0.922, bias −1.0 kcal (−4.2 kJ)] and Dietary Reference Intakes-Institute of Medicine [1382 ± 102 kcal (5786.2 ± 427.1 kJ), p = 0.315, bias 10.2 kcal (42.7 kJ)] equations showed better agreement and accurate prediction performance among BMI categories (79.1 and 82.6%, respectively). The BMI ≥ 30 kg/m² subgroup mREE [n = 111; 1516 ± 186 kcal (6347.2 ± 778.7 kJ)] was significantly lower than all predictive methods and had higher bias and over-prediction, except for Mifflin-St Jeor equation [1523 ± 186 kcal (6376.5 ± 778.7 kJ), p = 0.469, bias 7.7 kcal (32.2 kJ)].
Conclusion
Equations for estimating REE show wide performance variation, with limited accurate options in this population, especially among those with BMI > 30 kg/m².
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data presented in this study are available on request from the corresponding author.
References
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J, et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Fourth IFSO Global Registry Report 2018. Obes Surg. 2019;29:782–95.
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L. Bariatric Surgery Survey 2018: Similarities and Disparities Among the 5 IFSO Chapters. Obes Surg. 2021;31:1937–48
Iovino P, Himpens J, Scopinaro N, Vitiello A, Santonicola A, Buchwald H, et al. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes Surg. 2018;28:3783–94.
Maciejewski ML, Arterburn DE, Van Scoyoc L, Smith VA, Yancy WS, Weidenbacher HJ, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151:1046–55.
Ahmed B, King WC, Gourash W, Belle SH, Hinerman A, Pomp A, et al. Long-term weight change and health outcomes for sleeve gastrectomy (SG) and matched Roux-en-Y gastric bypass (RYGB) participants in the Longitudinal Assessment of Bariatric Surgery (LABS) study. Surgery. 2018;164:774–83.
Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc. 2017;31:4331–45.
Hayoz C, Hermann T, Raptis DA, Bronnimann A, Peterli R, Zuber M. Comparison of metabolic outcomes in patients undergoing laparoscopic roux-en-Y gastric bypass versus sleeve gastrectomy - a systematic review and meta-analysis of randomised controlled trials. Swiss Med Wkly. 2018;148:w14633.
Silva LB, Oliveira BMPM, Correia F. Evolution of body composition of obese patients undergoing bariatric surgery. Clin Nutr ESPEN. 2019;31:95–9.
Magro DO, Ueno M, Coelho-Neto JS, Callejas-Neto F, Pareja JC, Cazzo E. Long-term weight loss outcomes after banded Roux-en-Y gastric bypass: a prospective 10-year follow-up study. Surg Obes Relat Dis. 2018;14:910–7.
King WC, Hinerman AS, Belle SH, Wahed AS, Courcoulas AP. Comparison of the Performance of Common Measures of Weight Regain after Bariatric Surgery for Association with Clinical Outcomes. JAMA J Am Med Assoc. 2018;320:1560–9.
Westerterp KR. Control of energy expenditure in humans. Eur J Clin Nutr. 2017;71:340–4.
Schadewaldt P, Nowotny B, Straßburger K, Kotzka J, Roden M. Indirect calorimetry in humans: A postcalorimetric evaluation procedure for correction of metabolic monitor variability. Am J Clin Nutr. 2013;97:763–73.
Haugen AH, Chan LN, Li F. Indirect calorimetry: A practical guide for clinicians. Nutr Clin Pract. 2007;22:377–88.
Oshima T, Berger MM, De Waele E, Guttormsen AB, Heidegger C-P, Hiesmayr M, et al. Indirect calorimetry in nutritional therapy. A position paper by the ICALIC study group. Clin Nutr. 2017;36:651–62.
AARC. AARC Clinical Practice Guideline. Metabolic measurement using indirect calorimetry during mechanical ventilation – 2004 Revision & Update. Respir Care. 2004;49:1073e9.
Byham-Gray LD, Parrott JS, Peters EN, Fogerite SG, Hand RK, Ahrens S, et al. Modeling a Predictive Energy Equation Specific for Maintenance Hemodialysis. J Parenter Enter Nutr. 2018;42:587–96.
Jésus P, Marin B, Fayemendy P, Nicol M, Lautrette G, Sourisseau H, et al. Resting energy expenditure equations in amyotrophic lateral sclerosis, creation of an ALS-specific equation. Clin Nutr. 2019;38:1657–65.
de Oliveira Fernandes T, Avesani CM, Aoike DT, Cuppari L. New predictive equations to estimate resting energy expenditure of non-dialysis dependent chronic kidney disease patients. J Nephrol. 2021;34:1235–42.
Osuna-Padilla I, Aguilar-Vargas A, Rodríguez-Moguel NC, Villazón-De la Rosa A, Osuna-Ramírez I, Ormsby CE, et al. Resting energy expenditure in HIV/AIDS patients: Development and validation of a predictive equation. Clin Nutr ESPEN. 2020;40:288–92.
Disse E, Ledoux S, Bétry C, Caussy C, Maitrepierre C, Coupaye M, et al. An artificial neural network to predict resting energy expenditure in obesity. Clin Nutr. 2018;37:1661–9.
Harris JA, Benedict FG. A Biometric Study of Human Basal Metabolism. Proc Natl Acad Sci. 1918;4:370–3.
Roza AM, Shizgal HM. The Harris Benedict equation reevaluated: Resting energy requirements and the body cell mass. Am J Clin Nutr. 1984;40:168–82.
World Health Organization. Energy and protein requirements. Report of a joint FAO/WHO/UNU Expert Consultation. Switzerland: World Health Organization; 1985.
Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39:5–41.
Henry C. Basal metabolic rate studies in humans: measurement and development of new equations. Public Health Nutr. 2005;8:1133–52.
Institute of Medicine (U.S.). Panel on Macronutrients., Institute of Medicine (U.S.). Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. National Academies Press; 2005.
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–7.
Müller MJ, Bosy-Westphal A, Klaus S, Kreymann G, Lührmann PM, Neuhäuser-Berthold M, et al. World Health Organization equations have shortcomings for predicting resting energy expenditure in persons from a modern, affluent population: generation of a new reference standard from a retrospective analysis of a German database of resting energy expe. Am J Clin Nutr. 2004;80:1379–90.
Weijs PJM, Vansant GAAM. Validity of predictive equations for resting energy expenditure in Belgian normal weight to morbid obese women. Clin Nutr. 2010;29:347–51.
Frankenfield DC. Bias and accuracy of resting metabolic rate equations in non-obese and obese adults. Clin Nutr. 2013;32:976–82.
Orozco-Ruiz X, Pichardo-Ontiveros E, Tovar AR, Torres N, Medina-Vera I, Prinelli F, et al. Development and validation of new predictive equation for resting energy expenditure in adults with overweight and obesity. Clin Nutr. 2018;37:2198–205.
Lazzer S, Bedogni G, Lafortuna CL, Marazzi N, Busti C, Galli R, et al. Relationship between basal metabolic rate, gender, age, and body composition in 8,780 white obese subjects. Obesity. 2010;18:71–78.
Horie LM, Gonzalez MC, Torrinhas RS, Cecconello I, Waitzberg DL. New specific equation to estimate resting energy expenditure in severely obese patients. Obesity. 2011;19:1090–4.
Lamarca F, Vieira FT, Lima RM, Nakano EY, da Costa THM, Pizato N, et al. Effects of Resistance Training With or Without Protein Supplementation on Body Composition and Resting Energy Expenditure in Patients 2–7 Years PostRoux-en-Y Gastric Bypass: a Controlled Clinical Trial. Obes Surg. 2021;31:1635–46.
Berber LCL, Melendez-Araújo MS, Nakano EY, de Carvalho KMB, Dutra ES. Grazing Behavior Hinders Weight Loss in Long-Term Post Bariatric Surgery: a Cross-Sectional Study. Obes Surg. 2021;31:4076–82.
Berti LV, Campos J, Ramos A, Rossi M, Szego T, Cohen R. Position of the SBCBM - nomenclature and definition of outcomes of bariatric and metabolic surgery. ABCD Arq Bras Cir Dig. 2015;28:2–2.
da Silva FBL, Gomes DL, de Carvalho KMB. Poor diet quality and postoperative time are independent risk factors for weight regain after Roux-en-Y gastric bypass. Nutrition. 2016;32:1250–3.
Deitel M, Gawdat K, Melissas J. Reporting Weight Loss 2007. Obes Surg. 2007;17:565–8.
Compher C, Frankenfield D, Keim N, Roth-Yousey L. Best Practice Methods to Apply to Measurement of Resting Metabolic Rate in Adults: A Systematic Review. J Am Diet Assoc. 2006;106:881–903.
Fullmer S, Benson-Davies S, Earthman CP, Frankenfield DC, Gradwell E, Lee PSP, et al. Evidence Analysis Library Review of Best Practices for Performing Indirect Calorimetry in Healthy and Non-Critically Ill Individuals. J Acad Nutr Diet. 2015;115:1417–46.
Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155–63.
Duvoisin C, Favre L, Allemann P, Fournier P, Demartines N, Suter M. Roux-en-Y Gastric Bypass: Ten-year Results in a Cohort of 658 Patients. Ann Surg. 2018;268:1019–25.
Jiménez A, Ibarzabal A, Moizé V, Pané A, Andreu A, Molero J, et al. Ten-year outcomes after Roux-en-Y gastric bypass and sleeve gastrectomy: an observational nonrandomized cohort study. Surg Obes Relat Dis. 2019;15:382–8.
de Oliveira VLP, Martins GP, Mottin CC, Rizzolli J, Friedman R. Predictors of Long-Term Remission and Relapse of Type 2 Diabetes Mellitus Following Gastric Bypass in Severely Obese Patients. Obes Surg. 2018;28:195–203.
Hawkins RB, Mehaffey JH, McMurry TL, Kirby J, Malin SK, Schirmer B, et al. Clinical significance of failure to lose weight 10 years after roux-en-y gastric bypass. Surg Obes Relat Dis. 2017;13:1710–6.
Larjani S, Spivak I, Hao Guo M, Aliarzadeh B, Wang W, Robinson S, et al. Preoperative predictors of adherence to multidisciplinary follow-up care postbariatric surgery. Surg Obes Relat Dis. 2016;12:350–6.
Khorgami Z, Zhang C, Messiah SE, de la Cruz-Muñoz N. Predictors of Postoperative Aftercare Attrition among Gastric Bypass Patients. Bariatr Surg Pract Patient Care. 2016;10:79–83.
Nuijten MAH, Monpellier VM, Eijsvogels TMH, Janssen IMC, Hazebroek EJ, Hopman MTE. Rate and Determinants of Excessive Fat-Free Mass Loss After Bariatric Surgery. Obes Surg. 2020;30:3119–26.
Cole AJ, Kuchnia AJ, Beckman LM, Jahansouz C, Mager JR, Sibley SD, et al. Long-Term Body Composition Changes in Women Following Roux-en-Y Gastric Bypass Surgery. J Parenter Enter Nutr. 2017;41:583–91.
Lamarca F, Melendez-Araújo MS, Porto de Toledo I, Dutra ES, de Carvalho KMB. Relative Energy Expenditure Decreases during the First Year after Bariatric Surgery: A Systematic Review and Meta-Analysis. Obes Surg. 2019;29:2648–59.
Wolfe BM, Schoeller DA, McCrady-Spitzer SK, Thomas DM, Sorenson CE, Levine JA. Resting Metabolic Rate, Total Daily Energy Expenditure, and Metabolic Adaptation 6 Months and 24 Months After Bariatric Surgery. Obesity. 2018;26:862–8.
Nuijten MAH, Eijsvogels TMH, Monpellier VM, Janssen IMC, Hazebroek EJ, Hopman MTE. The magnitude and progress of lean body mass, fat-free mass, and skeletal muscle mass loss following bariatric surgery: A systematic review and meta-analysis. Obes Rev J Int Assoc Study Obes. 2022;23:e13370.
Heshka S, Lemos T, Astbury NM, Widen E, Davidson L, Goodpaster BH, et al. Resting Energy Expenditure and Organ-Tissue Body Composition 5 Years After Bariatric Surgery. Obes Surg. 2020;30:587–94.
Dias Rodrigues JC, Lamarca F, Lacroix de Oliveira C, Cuppari L, Lourenço RA, Avesani CM. Agreement between prediction equations and indirect calorimetry to estimate resting energy expenditure in elderly patients on hemodialysis. ESPEN J. 2014;9:e91–6.
Nwanosike EM, Conway BR, Merchant HA, Hasan SS. Potential applications and performance of machine learning techniques and algorithms in clinical practice: A systematic review. Int J Med Inform. 2022;159:104679.
Enodien B, Taha-Mehlitz S, Saad B, Nasser M, Frey DM, Taha A. The development of machine learning in bariatric surgery. Front Surg. 2023;10:1–8.
Bektaş M, Reiber BMM, Pereira JC, Burchell GL, van der Peet DL. Artificial Intelligence in Bariatric Surgery: Current Status and Future Perspectives. Obes Surg. 2022;32:2772–83.
Bellini V, Valente M, Turetti M, Del Rio P, Saturno F, Maffezzoni M, et al. Current Applications of Artificial Intelligence in Bariatric Surgery. Obes Surg. 2022;32:2717–33.
Acknowledgements
We are particularly thankful to Gabriela Sousa de Oliveira, Isabela Nogueira Martins Sena Rios, and Gustavo Neves de Souza Gomes for contributing to data collection.
Funding
This study was funded by the Foundation for Research Support of the Federal District (FAPDF; grant number 0193.001.462/2016), the Brazilian National Council for Scientific and Technological Development and the Ministry of Health (CNPq/MS; grant number 408340/2017-7). The authors RML and KMBC also thank CNPq (grant numbers 305746/2022-7 and 302740/2022-8) for the financial support.
Author information
Authors and Affiliations
Contributions
Conceptualization, FL and ESD; Formal analysis, FL; Funding acquisition, KMBC; Investigation, FL, FTV and MSMA; Methodology, FL, FTV, MSMA, RML, ESD and KMBC; Project administration, KMBC; Supervision, RML, ESD and KMBC; Writing – original draft, FL; Writing – review & editing, FL, FTV, MSMA, RML, ESD and KMBC.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committee of the Faculty of Health Sciences of the University of Brasília [protocol codes 2,052,734 (2017) and 3,595,291 (2018)]. Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lamarca, F., T. Vieira, F., S. Melendez-Araújo, M. et al. Resting energy expenditure of females mid- to long-term after bariatric surgery: agreement between indirect calorimetry and predictive methods. Eur J Clin Nutr 79, 587–596 (2025). https://doi.org/10.1038/s41430-025-01577-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01577-2