Abstract
Background/Objectives
Depressive mood is prevalent in geriatric patients who undergo rehabilitation. Malnutrition, which frequently coexists in this demographic group, likely affects mental health status significantly. This study examined the association between malnutrition and depressive mood at discharge in geriatric patients who were undergoing rehabilitation and identified the mediating roles of specific malnutrition components in this association.
Subjects/Methods
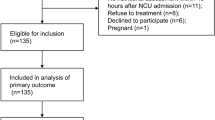
This prospective cohort study comprised 189 geriatric rehabilitation patients. Malnutrition was determined using the Global Leadership Initiative on Malnutrition (GLIM) criteria, and depressive mood was assessed using the Geriatric Depression Scale-15 (GDS-15). The potential mediation of the GLIM components in the relationship between malnutrition and depressive mood was evaluated using causal mediation analysis.
Results
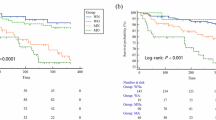
Malnutrition was positively associated with increased GDS-15 scores at both admission (p = 0.007) and discharge (p < 0.001). The severity of malnutrition corresponded with increased odds of depressive mood at discharge (moderate malnutrition: odds ratio [OR] 3.84, 95% confidence interval [CI] 1.48–9.94, p = 0.005; severe malnutrition: OR 5.11, 95% CI 1.52–15.17, p = 0.003). Notably, both muscle mass reduction (OR 1.51, 95% CI 1.01–2.27, p = 0.042) and disease burden (OR 1.37, 95% CI 1.00–1.89, p = 0.047) were identified as mediators in the association between malnutrition and depressive mood at discharge.
Conclusions
Nutritional status significantly influenced the mental health of geriatric rehabilitation patients, with muscle mass reduction and disease burden mediating this relationship. These findings emphasize the importance of a multidimensional geriatric rehabilitation approach that includes nutritional interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
This data utilized in this study is not publicly available by privacy regulations and the protection of personal information.
References
Cully JA, Gfeller JD, Heise RA, Ross MJ, Teal CR, Kunik ME. Geriatric depression, medical diagnosis, and functional recovery during acute rehabilitation. Arch Phys Med Rehabil. 2005;86:2256–60. https://doi.org/10.1016/j.apmr.2005.07.292.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med. 2003;163:2433–45. https://doi.org/10.1001/archinte.163.20.2433.
Butters MA, Whyte EM, Nebes RD, Begley AE, Dew MA, Mulsant BH, et al. The nature and determinants of neuropsychological functioning in late-life depression. Arch Gen Psychiatry. 2004;61:587–95. https://doi.org/10.1001/archpsyc.61.6.587.
Shimizu A, Maeda K, Honda T, Ishida Y, Ueshima J, Nagami S, et al. Comparison between the Global Leadership Initiative on Malnutrition and the European Society for Clinical Nutrition and Metabolism definitions for the prevalence of malnutrition in geriatric rehabilitation care. Geriatr Gerontol Int. 2020;20:1221–7. https://doi.org/10.1111/ggi.14072.
Clark AB, Reijnierse EM, Lim WK, Maier AB. Prevalence of malnutrition comparing the GLIM criteria, ESPEN definition and MST malnutrition risk in geriatric rehabilitation patients: RESORT. Clin Nutr. 2020;39:3504–11. https://doi.org/10.1016/j.clnu.2020.03.015.
Shimizu A, Maeda K, Koyanagi Y, Kayashita J, Fujishima I, Mori N. The global leadership initiative on malnutrition-defined malnutrition predicts prognosis in persons with stroke-related dysphagia. J Am Med Dir Assoc. 2019;20:1628–33. https://doi.org/10.1016/j.jamda.2019.07.008.
Hettiarachchi J, Reijnierse EM, Soh CH, Agius B, Fetterplace K, Lim WK, et al. Malnutrition is associated with poor trajectories of activities of daily living in geriatric rehabilitation inpatients: RESORT. Mech Ageing Dev. 2021;197:111500 https://doi.org/10.1016/j.mad.2021.111500.
Smoliner C, Norman K, Wagner KH, Hartig W, Lochs H, Pirlich M. Malnutrition and depression in the institutionalised elderly. Br J Nutr. 2009;102:1663–7. https://doi.org/10.1017/S0007114509990900.
Rojer AGM, Denneman BCM, Brouwer P, Ramsey KA, Trappenburg MC, Meskers CGM, et al. Determinants of instrumented sedentary and physical activity behavior in geriatric rehabilitation inpatients: RESORT. Exp Gerontol. 2021;154:111524. https://doi.org/10.1016/j.exger.2021.111524.
Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011;25:540–7. https://doi.org/10.1177/1545968311402696.
Sheikh JI. Geriatric Depression Scale (GDS) Recent evidence and development of a shorter version. Clinical Gerontology: A Guide to Assessment and Intervention 1986:165–73.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–83. https://doi.org/10.1016/0021-9681(87)90171-8. e-pub ahead of print 1987/01/01.
Shimizu A, Maeda K, Ueshima J, Inoue T, Murotani K, Ohno T, et al. Prevalence of sarcopenic obesity based on newly proposed diagnostic criteria and functional outcomes in older adults undergoing rehabilitation. Mech Ageing Dev. 2022;208:111728. https://doi.org/10.1016/j.mad.2022.111728.
Kunieda K, Ohno T, Fujishima I, Hojo K, Morita T. Reliability and validity of a tool to measure the severity of dysphagia: The Food Intake LEVEL Scale. J Pain Symptom Manag. 2013;46:201–6. https://doi.org/10.1016/j.jpainsymman.2012.07.020.
Kidd D, Stewart G, Baldry J, Johnson J, Rossiter D, Petruckevitch A. et al. The Functional Independence Measure: A comparative validity and reliability study. Disabil Rehabil. 1995;17:10–14. https://doi.org/10.3109/09638289509166622. e-pub ahead of print 1995/01/01.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. https://doi.org/10.1016/0022-3956(75)90026-6. e-pub ahead of print 1975/11/01.
Zhang XM, Jiao J, Cao J, Guo N, Zhu C, Li Z, et al. Handgrip strength and depression among older Chinese inpatients: A cross-sectional study. Neuropsychiatr Dis Treat. 2021;17:1267–77. https://doi.org/10.2147/NDT.S301064.
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle. 2019; 10:207–17. https://doi.org/10.1002/jcsm.12383. e-pub ahead of print 2019/03/29.
Stratton RJ, Hackston A, Longmore D, Dixon R, Price S, Stroud M, et al. Malnutrition in hospital outpatients and inpatients: Prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr. 2004;92:799–808 https://doi.org/10.1079/bjn20041258. e-pub ahead of print 2004/11/10.
Shimizu A, Maeda K, Wakabayashi H, Nishioka S, Nagano A, Kayashita J, et al. Predictive validity of body mass index cutoff values used in the global leadership initiative on malnutrition criteria for discriminating severe and moderate malnutrition based on in-patients with pneumonia in Asians. JPEN J Parenter Enter Nutr. 2021;45:941–50. https://doi.org/10.1002/jpen.1959.
Maeda K, Ishida Y, Nonogaki T, Mori N. Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr. 2020;39:180–4. https://doi.org/10.1016/j.clnu.2019.01.011.
Shimizu A, Fujishima I, Maeda K, Murotani K, Ohno T, Nomoto A, et al. Delayed dysphagia may be sarcopenic dysphagia in patients after stroke. J Am Med Dir Assoc. 2021;22:2527–33.e1. https://doi.org/10.1016/j.jamda.2021.07.013.
Shimizu A, Fujishima I, Maeda K, Murotani K, Ohno T, Nomoto A, et al. Association between food texture levels consumed and the prevalence of malnutrition and sarcopenia in older patients after stroke. Eur J Clin Nutr. 2022;76:1576–82. https://doi.org/10.1038/s41430-022-01126-1.
Shimizu A, Nozoe M, Ohno T, Nomoto A, Shigematsu T, Fujishima I. Association of medial gastrocnemius adiposity with poststroke severe malnutrition and functional performance of activities of daily living in older patients: A prospective analysis. Nutr Clin Pract. 2023;38:167–76. https://doi.org/10.1002/ncp.10902.
Sánchez-Torralvo FJ, Contreras-Bolívar V, Ruiz-Vico M, Abuín-Fernández J, González-Almendros I, Barrios M, et al. Relationship between malnutrition and the presence of symptoms of anxiety and depression in hospitalized cancer patients. Support Care Cancer. 2022;30:1607–13. https://doi.org/10.1007/s00520-021-06532-y.
Tennant PWG, Murray EJ, Arnold KF, Berrie L, Fox MP, Gadd SC, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: Review and recommendations. Int J Epidemiol. 2021;50:620–32. https://doi.org/10.1093/ije/dyaa213.
Westreich D, Greenland S. The Table 2 fallacy: Presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177:292–8. https://doi.org/10.1093/aje/kws412.
Rijnhart JJM, Valente MJ, Smyth HL, MacKinnon DP. Statistical mediation analysis for models with a binary mediator and a binary outcome: The differences between causal and traditional mediation analysis. Prev Sci. 2021. https://doi.org/10.1007/s11121-021-01308-6. e-pub ahead of print: 20211116.
Steen J, Loeys T, Moerkerke B, Vansteelandt S medflex: An R package for Flexible Mediation Analysis using Natural Effect Models. J Stat Softw. 2017;76. https://doi.org/10.18637/jss.v076.i11.
Saunders J, Smith T. Malnutrition: Causes and consequences. Clin Med (Lond). 2010;10:624–7. https://doi.org/10.7861/clinmedicine.10-6-624.
Muscaritoli M. The impact of nutrients on mental health and well-being: Insights from the literature. Front Nutr. 2021;8:656290. https://doi.org/10.3389/fnut.2021.656290.
Yoshimura Y, Wakabayashi H, Bise T, Nagano F, Shimazu S, Shiraishi A, et al. Sarcopenia is associated with worse recovery of physical function and dysphagia and a lower rate of home discharge in Japanese hospitalized adults undergoing convalescent rehabilitation. Nutrition. 2019;61:111–8. https://doi.org/10.1016/j.nut.2018.11.005.
Li Z, Tong X, Ma Y, Bao T, Yue J. Prevalence of depression in patients with sarcopenia and correlation between the two diseases: Systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13:128–44. https://doi.org/10.1002/jcsm.12908.
Khezrian M, McNeil CJ, Myint PK, Murray AD. The association between polypharmacy and late life deficits in cognitive, physical and emotional capability: A cohort study. Int J Clin Pharm. 2019;41:251–7. https://doi.org/10.1007/s11096-018-0761-2.
Shimizu A, Maeda K, Ueshima J, Ishida Y, Inoue T, Murotani K, et al. Effects of sarcopenia on changes in prevalence of patients with depressive mood during hospitalization in geriatric rehabilitation. Ann Geriatr Med Res. 2024. e-pub ahead of print 20240723. https://doi.org/10.4235/agmr.24.0088.
Shiraishi R, Shiraishi N, Fujimoto Y, Ogawa T. Malnutrition suppresses improvements in depression symptoms in older adult patients with stroke undergoing convalescent rehabilitation. Clin Nutr ESPEN. 2024;63:508–14. https://doi.org/10.1016/j.clnesp.2024.07.013. e-pub ahead of print 20240723.
Funding
AS reports financial support was provided by Japan Society for the Promotion of Science (23K16799).
Author information
Authors and Affiliations
Contributions
Akio Shimizu: Conceptualization, Data Curation, Writing - Original Draft Preparation, Keisuke Maeda: Supervision, Validation, Writing - Original Draft Preparation. Junko Ueshima: Methodology, Analysis, Data Curation. Yuria Ishida: Visualization, Analysis, Writing - Review & Editing. Tatsuro Inoue: Supervision, Analysis, Writing - Review & Editing. Ichiro Fujisima: Conceptualization, Investigation, Writing - Review & Editing. Naoharu Mori: Methodology, Resources, Writing - Review & Editing. Kenta Murotani: Software, Validation, Analysis. Ayano Nagano: Visualization, Validation, Writing - Original Draft Preparation. Tomohisa Ohno: Conceptualization, Visualization, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare that there is no actual or potential conflict of interest with regard to the publication of this article.
Ethics
This study was approved by the Ethics Committee of the Hamamatsu City Rehabilitation Hospital (No. 21-82) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants provided verbal informed consent for participation in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shimizu, A., Maeda, K., Ueshima, J. et al. Association of GLIM-defined malnutrition with depressive mood in older adults undergoing rehabilitation. Eur J Clin Nutr 79, 597–603 (2025). https://doi.org/10.1038/s41430-025-01584-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01584-3