Abstract
Objectives
to analyze the association between food and nutrition insecurity (FNI) and sociodemographic, clinical, and anthropometric indicators in individuals with cancer eligible for curative radiotherapy.
Methods
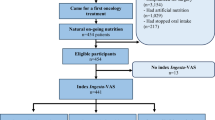
Study with the collection of sociodemographic and clinical data, and nutritional, anthropometric, and FNI assessment. Estimated Prevalence Ratio (PR) and 95% confidence intervals (95% CI) of FNI and exposure variables using the Poisson regression model with robust variance.
Results
252 individuals were evaluated, 51.2% female, 60.7% elderly, 40.1% with breast or uterine cancer, 27.8% with urological cancer, 18.2% with head and neck cancer, and 7.5% with difficulty acquiring an enteral diet or nutritional supplement. The prevalence of FNI was 17.9%, 6.4% being moderate and 3.6% severe. FNI was less frequent in the high-income tertile (PR = 0,38; 95% CI: 0,18–0,79), and in individuals with urological tumors (PR = 0.12; 95% CI: 0.04–0.37), while higher prevalences were identified in non-white individuals (PR = 1,82; 95% CI: 1.01–3.28) among those with stage IV tumor (PR = 1.42; 95% CI: 1.03–1.95), with severe weight loss (PR = 2.99; 95% CI: 1.75–4.82), severely malnourished (PR = 2.58; 95% CI: 1.34–4.95) and bedridden (PR = 5.54; 95% CI: 2.72–11.29). Additionally, a higher prevalence of FNI associated with a reduction in usual food consumption (PR = 2.09; 95% CI: 1.24–3.54), the need to modify the consistency of the diet (PR = 3.45; 95% CI: 2.11–5.67), use of caloric supplements (PR = 2.07; 95% CI: 1.17–3.69) or enteral feeding (PR = 3.46; 95% CI: 2.01–5.94).
Conclusion
One in five individuals with cancer presented FNI associated with socioeconomic and nutritional vulnerability in the radiotherapy pre-treatment phase.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Pearce A, Sharp L, Hanly P, Barchuk A, Bray F, de Camargo Cancela M, et al. Productivity losses due to premature mortality from cancer in Brazil, Russia, India, China, and South Africa (BRICS): a population-based comparison. Cancer Epidemiol. 2018;53:27–34.
Patel KG, Borno HT, Seligman HK. Food insecurity screening: a missing piece in cancer management. Cancer. 2019;125:3494–501.
Wünsch Filho V, Antunes JLF, Boing AF, Lorenzi RL. Perspectivas da investigação sobre determinantes sociais em câncer. Physis: Rev de Saúde Coletiva. 2008;18:427–50.
INCA. Tratamento do câncer Rio de Janeiro: Instituto Nacional de Câncer; 2022 [Available from: https://www.inca.gov.br/tratamento/radioterapia.
Citak E, Tulek Z, Uzel O. Nutritional status in patients with head and neck cancer undergoing radiotherapy: a longitudinal study. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 2019;27:239–47.
Jin S, Lu Q, Sun Y, Xiao S, Zheng B, Pang D, et al. Nutrition impact symptoms and weight loss in head and neck cancer during radiotherapy: a longitudinal study. BMJ Supportive Palliat Care. 2021;11:17–24.
Lin TA, Wei L-J, Ludmir EB. Radiotherapy alone vs radiotherapy with concurrent chemoradiotherapy and survival of patients with low-risk nasopharyngeal carcinoma. JAMA. 2023;329:260–1.
Nazari V, Pashaki AS, Hasanzadeh E. The reliable predictors of severe weight loss during the radiotherapy of head and neck cancer. Cancer Treat Res Commun. 2021;26:100281.
Yurut-Caloglu V, Caloglu M, Turkkan G. The importance of weight loss during definitive radiotherapy in patients with laryngeal carcinoma. J Cancer Res Ther. 2022;18:638–43.
Paixão EMS, Gonzalez MC, Nakano EY, Ito MK, Pizato N. Weight loss, phase angle, and survival in cancer patients undergoing radiotherapy: a prospective study with 10-year follow-up. Eur J Clin Nutr. 2021;75:823–8.
Croisier E, Morrissy A, Brown T, Grigg A, Chan P, Goh J, et al. Nutrition risk screening and implications for patients with gynaecological cancers undergoing pelvic radiotherapy and/or other treatment modalities: a retrospective observational study. Nutr Diet J Dietit Assoc Aust. 2022;79:217–28.
Henson CC, Burden S, Davidson SE, Lal S. Nutritional interventions for reducing gastrointestinal toxicity in adults undergoing radical pelvic radiotherapy. Cochrane Database Syst Rev. 2013;26:CD009896.
Saltaouras G, Lightowler H, Coe S, Watson E. Diet and nutrition information and support needs in pelvic radiotherapy: a systematic, mixed-methods review. Eur J Cancer Care. 2020;29:e13297.
Bezerra MS, Jacob MCM, Ferreira MAF, Vale D, Mirabal IRB, CdO Lyra. Insegurança alimentar e nutricional no Brasil e sua correlação com indicadores de vulnerabilidade. Ciência Saúde Coletiva. 2020;25:3833–46.
Raber M, Jackson A, Basen-Engquist K, Bradley C, Chambers S, Gany FM, et al. Food insecurity among people with cancer: nutritional needs as an essential component of care. J Natl Cancer Inst. 2022;114:1577–83.
BRASIL. Lei Orgânica de Segurança Alimentar Nutricional (Losan). Lei n° 11.346, de 15 de setembro de 2006. Cria o Sistema Nacional de Segurança Alimentar e Nutricional-SISAN com vistas em assegurar o direito humano à alimentação adequada e dá outras providências. In: CONSEA, editor. Diário Oficial da União: Conselho Nacional de Segurança Alimentar e Nutricional; 2006.
BRASIL. [Emenda Constituição (1964)]. Emenda Constitucional no 64, de 4 de fevereiro de 2010. Brasília: Diário Oficial da União; 2010
Mazur CE, Schmidt ST, SdA Rigon, Schieferdecker MEM. Home enteral nutrition therapy: Interface between human right to adequate food and food security and nutrition. DEMETRA: Alimentção, Nutrção Saúde. 2014;9:757–69.
Ribeiro-Silva RDC, Pereira M, Campello T, Aragão É, Guimarães JMDM, Ferreira AJ, et al. Implicações da pandemia COVID-19 para a segurança alimentar e nutricional no Brasil. Ciência Saúde Coletiva. 2020;25:3421–30.
Gany F, Melnic I, Ramirez J, Wu M, Li Y, Paolantonio L, et al. The association between housing and food insecurity among medically underserved cancer patients. Support care cancer. 2021;29:7765–74.
Simmons LA, Modesitt SC, Brody AC, Leggin AB. Food insecurity among cancer patients in Kentucky: a pilot study. J Oncol Pract. 2006;2:274–9.
Berger M, Lin H, Bhattacharyya N. A national evaluation of food insecurity in a head and neck cancer population. Laryngoscope. 2021;131:1539–42.
Camacho-Rivera M, Islam J, Rodriguez D, Vidot D, Bailey Z. Food insecurity disparities and mental health impacts among cancer survivors during the COVID-19 Pandemic. Health equity. 2022;6:729–37.
Chan J, Polo A, Zubizarreta E, Bourque J, Hanna T, Gaudet M, et al. Access to radiotherapy and its association with cancer outcomes in a high-income country: Addressing the inequity in Canada. Radiother Oncol J Eur Soc Ther Radiol Oncol 2019;141:48–55.
Ojinnaka C, Bruening M. Black-White racial disparities in health care utilization and self-reported health among cancer survivors: the role of food insecurity. Cancer. 2021;127:4620–7.
HEG. Relatório de Sustentabilidade 2022 Erasto Gaertner: Hospital Erasto Gaertner; 2022. Available from: https://erastogaertner.com.br/arquivos/relatorio2022/heg-relatorio-2022.pdf.
OMS. Classificação Internacional de Doenças para Oncologia: CID-O. 3. ed. ed. São Paulo: Editora da Organização Mundial da Saúde; 2013.
WHO. Expert Committee on Physical Status: the Use and Interpretation of Anthropometry: World Health Organization; 1995. Available from: https://apps.who.int/iris/bitstream/handle/10665/37003/WHO_TRS_854.pdf?sequence=1&isAllowed=y.
Blackburn GL, Bistrian BR, Maini BS, Schlamm HT, Smith MF. Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Enter Nutr. 1977;1:11–22.
INCA. Inquérito brasileiro de nutrição oncológica. 1 ed. Rio de Janeiro2013.
Segall-Corrêa AM, Marin-León L, Melgar-Quiñonez H, Pérez-Escamilla R. Refinement of the Brazilian household food insecurity measurement scale: recommendation for a 14-item EBIA. Rev de Nutrção. 2014;27:241–51.
Kepple AW, Segall-Corrêa AM. Conceituando e medindo segurança alimentar e nutricional. Ciência Saúde Coletiva. 2011;16:187–99.
Segall-Correa AM. Insegurança alimentar medida a partir da percepção das pessoas. Estudos Avançados. 2007;21:143–54.
INCA. Estimativa 2023: incidência de câncer no Brasil. Rio de Janeiro: Instituto Nacional de Câncer; 2022. 160 p.
Bullock A, Patterson M, Paton L, Currow D, Johnson M. Malnutrition, sarcopenia and cachexia: exploring prevalence, overlap, and perceptions in older adults with cancer. European Journal of Clinical Nutr. 2024.
Charkhchi P, Fazeli DS, Carlos R. Housing and Food Insecurity, Care Access, and Health Status Among the Chronically Ill: An Analysis of the Behavioral Risk Factor Surveillance System. J Gen Intern Med. 2018;33:644–50.
Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017 2018. Available from: https://www.ers.usda.gov/webdocs/publications/90023/err-256.pdf.
Gany F, Lee T, Ramirez J, Massie D, Moran A, Crist M, et al. Are our severely ill patients hungry? J Clin Oncol. 2011;29:19626.
Derette K, Rollet Q, Launay L, Launoy G. Bryere J. Evolution of socioeconomic inequalities in cancer incidence between 2006 and 2016 in France: a population-based study. Eur J Cancer Prev Off J Eur Cancer Prev Organ (ECP) 2022;31:473–81.
Sousa ACADL, Barbosa KCDO, Barroso MLF. Soares ALFdH. Brasil: fumar y consumo de bebidas alcohólicas en los últimos diez años (vigitel) y el papel del Cirujano Dental en la prevención del cáncer oral. Research. Soc Dev. 2021;10:39110817278.
Bezerra TA, Olinda RAD, Pedraza DF. Insegurança alimentar no Brasil segundo diferentes cenários sociodemográficos. Ciência Saúde Coletiva. 2017;22:637–51.
Hoffmann R. Determinantes da insegurança alimentar no brasil: análise dos dados da PNAD de 2004. Segurança Alimentar e Nutricional. 2008;15:49–61.
Segall-Corrêa AM, Marin-Leon L, Helito H, Pérez-Escamilla R, Santos LMP, Paes-Sousa R. Transferência de renda e segurança alimentar no Brasil: análise dos dados nacionais. Rev de Nutrção. 2008;21:39s–51s.
Gany F, Lee T, Ramirez J, Massie D, Moran A, Crist M, et al. Do our patients have enough to eat? Food insecurity among urban low-income cancer patients. J Health Care Poor Underserved. 2014;25:1153–68.
Coughlin SS. Food insecurity among cancer patients: a systematic review. Int J Food Nutr Sci. 2021;8:41–5.
Bauer J, Capra S, Ferguson M. Use of the scored patient-generated subjective global assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. Eur J Clin Nutr. 2002;56:779–85.
Neoh M, Abu ZZ, Mat Daud Z, Md Yusop N, Ibrahim Z, et al. Changes in nutrition impact symptoms, nutritional and functional status during head and neck cancer treatment. Nutrients. 2020;12:1225.
Pinho N, Martucci R, Rodrigues V, D’Almeida C, Thuler L, Saunders C, et al. Malnutrition associated with nutrition impact symptoms and localization of the disease: results of a multicentric research on oncological nutrition. Clin Nutr. 2019;38:1274–9.
Crowder S, Douglas K, Yanina Pepino M, Sarma K, Arthur A. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: a systematic review. J Cancer Survivorship: Res Pract 2018;12:479–94.
Acknowledgements
We express our gratitude to the Graduate Program in Food and Nutrition, the Department of Nutrition at the Federal University of Paraná, and the Erasto Gaertner Hospital for providing the facilities and equipment for conducting the research and data analysis. We extend our thanks to all those who contributed at every stage of the study.
Funding
The project utilized resources from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) e Fundação Araucária through the institutional program for undergraduate research students. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Contributions
PCA: study concept, data acquisition, analysis, and manuscript drafting. AFOH: study concept, data acquisition, and manuscript critical review. DAH: study concept, statistical analysis, data interpretation, manuscript critical review, and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was conducted in accordance with relevant guidelines and regulations. The project was approved by the Research Ethics Committee of the Federal University of Paraná on 02/21/2022 under the Certificate of Presentation of Ethical Appreciation protocol number 53073721.0.0000.0102 and was subsequently approved by the Erasto Gaertner Hospital’s Research Ethics Committee on 03/09/2022. The Free and Informed Consent Form was applied, and consent to participate in the research was given upon agreement and signature of the term by the participant.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Andrade, P.C., de Oliveira Hinokuma, A.F. & Höfelmann, D.A. Food and nutrition insecurity and clinical and anthropometric indicators in individuals with cancer eligible for radiotherapy. Eur J Clin Nutr 79, 690–697 (2025). https://doi.org/10.1038/s41430-025-01593-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01593-2