Abstract
Background/Objective
Since muscle strength is modifiable and handgrip strength is a reliable biomarker for strength and mortality, exploring its association with mortality in individuals with severe obesity could help identify protective thresholds. We aimed to examine the dose-response association between handgrip strength and mortality in adults with severe obesity.
Subjects/Methods
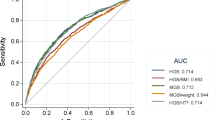
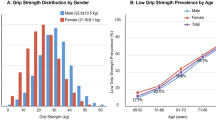
We retrieved data from the Survey of Health, Ageing and Retirement in Europe (SHARE). Handgrip strength was measured in participants with a body mass index (BMI) higher than 40 kg/m2. We used time-varying Cox proportional hazards regression to assess the association between handgrip strength and all-cause mortality risk. To account for potential non-linearity, we employed restricted cubic splines. We examined a total of 2229 adults (67.9% women; BMI of 43.8 kg/m2).
Results
We found an association between handgrip strength and mortality, showing a minimal and optimal dose for a reduced risk with 31 kg (HR 0.97, 95% CI, 0.96–0.99) and 36 kg (HR 0.90, 95% CI, 0.81–0.99), respectively. Additional sex-stratified analysis showed that lower than median levels of handgrip strength were gradually associated with increased risk in both men and women.
Conclusions
The association between handgrip strength and all-cause mortality in European adults with severe obesity highlights practical thresholds for risk reduction, with 31 kg as the minimum and 36 kg as the optimal strength level. In both men and women, handgrip strength below the median was linked to a gradual increase in mortality risk, emphasizing the importance of maintaining adequate muscle strength to improve health outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data described in the manuscript can be accessed through an application to the SHARE database. Code book and analytic code will be made publicly and freely available upon reasonable request to the corresponding author.
References
Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, et al. The science of obesity management: an endocrine society scientific statement. Endocr Rev. 2018;39:79–132.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet Lond Engl. 2024;403:1027–50.
Xu H, Cupples LA, Stokes A, Liu CT. Association of obesity with mortality over 24 years of weight history: findings from the Framingham Heart Study. JAMA Netw Open. 2018;1:e184587.
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9.
Prado CMM, Wells JCK, Smith SR, Stephan BCM, Siervo M. Sarcopenic obesity: a Critical appraisal of the current evidence. Clin Nutr Edinb Scotl. 2012;31:583–601.
Carbone S, Billingsley HE, Rodriguez-Miguelez P, Kirkman DL, Garten R, Lee Franco R, et al. Lean mass abnormalities in heart failure: the role of sarcopenia, sarcopenic obesity, and cachexia. Curr Probl Cardiol. 2020;45:100417.
Carbone S, Lavie CJ, Arena R. Obesity and heart failure: focus on the obesity paradox. Mayo Clin Proc. 2017;92:266–79.
Ventura HO, Carbone S, Lavie CJ. Muscling up to improve heart failure prognosis. Eur J Heart Fail. 2018;20:1588–90.
Upadhya B, Haykowsky MJ, Eggebeen J, Kitzman DW. Sarcopenic obesity and the pathogenesis of exercise intolerance in heart failure with preserved ejection fraction. Curr Heart Fail Rep. 2015;12:205–14.
Emami A, Saitoh M, Valentova M, Sandek A, Evertz R, Ebner N, et al. Comparison of sarcopenia and cachexia in men with chronic heart failure: results from the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF). Eur J Heart Fail. 2018;20:1580–7.
Williams PT. Dose-response relationship of physical activity to premature and total all-cause and cardiovascular disease mortality in walkers. PLoS ONE. 2013;8:e78777.
Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–25.
Armstrong MEG, Green J, Reeves GK, Beral V, Cairns BJ, Million Women Study Collaborators. Frequent physical activity may not reduce vascular disease risk as much as moderate activity: large prospective study of women in the United Kingdom. Circulation. 2015;131:721–9.
Koolhaas CM, Dhana K, Schoufour JD, Ikram MA, Kavousi M, Franco OH. Impact of physical activity on the association of overweight and obesity with cardiovascular disease: the Rotterdam Study. Eur J Prev Cardiol. 2017;24:934–41.
Fogelholm M. Physical activity, fitness and fatness: relations to mortality, morbidity and disease risk factors. A systematic review. Obes Rev J Int Assoc Study Obes. 2010;11:202–21.
Tomlinson DJ, Erskine RM, Morse CI, Winwood K, Onambélé-Pearson G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology. 2016;17:467–83.
ten Hoor GA, Plasqui G, Schols AMWJ, Kok G. A benefit of being heavier is being strong: a cross-sectional study in young adults. Sports Med Open. 2018;4:12.
Bohannon RW. Grip strength: an indispensable biomarker for older adults. Clin Inter Aging. 2019;14:1681–91.
López-Bueno R, Andersen LL, Koyanagi A, Núñez-Cortés R, Calatayud J, Casaña J, et al. Thresholds of handgrip strength for all-cause, cancer, and cardiovascular mortality: a systematic review with dose-response meta-analysis. Ageing Res Rev. 2022;82:101778.
Bhaskaran K, dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53.
Bauer S, Reiter L, Weijs PJM, Schoufour JD, Boirie Y, Topinková E, et al. Adherence to resistance training and hypocaloric diet among persons near retirement age — a secondary data analysis of three randomized controlled trials. J Nutr Health Aging. 2024;28:100344.
Bergmann M, Wagner M, Börsch-Supan A. SHARE Wave 9 methodology: from the SHARE Corona Survey 2 to the SHARE Main Wave 9 Interview [Internet]. 2024. https://share-eric.eu/fileadmin/user_upload/Methodology_Volumes/SHARE_Methodenband_WEB_Wave9.pdf
Börsch-Supan A, Brandt M, Hunkler C, Kneip T, Korbmacher J, Malter F, et al. Data resource profile: the survey of health, ageing and retirement in Europe (SHARE). Int J Epidemiol. 2013;42:992–1001.
Andersen LL, Calatayud J, Núñez-Cortés R, Polo-López A, López-Bueno R. Facilitators and barriers for working beyond statutory pension age: A prospective cohort study across 26 European countries. Scand J Work Environ Health. 2024. https://doi.org/10.5271/sjweh.4189
López-Bueno R, Andersen LL, Calatayud J, Casaña J, Grabovac I, Oberndorfer M, et al. Associations of handgrip strength with all-cause and cancer mortality in older adults: a prospective cohort study in 28 countries. Age Ageing. 2022;51:afac117.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J. 2004;25:2212–9.
Qi KJ, Li Q, Lu GL, Zhang MJ, Zhang MZ, Yan JM, et al. The combined effect of handgrip strength and obesity phenotype on the risk of stroke in Chinese middle-aged and elderly: A cohort study. Arch Gerontol Geriatr. 2024;124:105481.
Wei L, Wang B, Wang Y. Low handgrip strength with asymmetry is associated with elevated all-cause mortality risk in older Chinese adults with abdominal obesity. PLoS ONE. 2024;19:e0306982.
da Silva Alexandre T, Scholes S, Ferreira Santos JL, de Oliveira Duarte YA, de Oliveira C. Dynapenic abdominal obesity increases mortality risk among English and Brazilian older adults: a 10-year follow-up of the ELSA and SABE studies. J Nutr Health Aging. 2018;22:138–44.
He N, Zhang Y, Zhang L, Zhang S, Ye H. Relationship between sarcopenia and cardiovascular diseases in the elderly: an overview. Front Cardiovasc Med. 2021;8:743710.
Sacheck JM, Kuder JF, Economos CD. Physical fitness, adiposity, and metabolic risk factors in young college students. Med Sci Sports Exerc. 2010;42:1039–44.
Garcia-Hermoso A, Tordecilla-Sanders A, Correa-Bautista JE, Peterson MD, Izquierdo M, Prieto-Benavides D, et al. Handgrip strength attenuates the adverse effects of overweight on cardiometabolic risk factors among collegiate students but not in individuals with higher fat levels. Sci Rep. 2019;9:6986.
Aadahl M, Beyer N, Linneberg A, Thuesen BH, Jørgensen T. Grip strength and lower limb extension power in 19-72-year-old Danish men and women: the Health2006 study. BMJ Open. 2011;1:e000192.
Kuh D, Bassey EJ, Butterworth S, Hardy R, Wadsworth MEJ, Musculoskeletal Study Team. Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol A Biol Sci Med Sci. 2005;60:224–31.
Benito PJ, López-Plaza B, Bermejo LM, Peinado AB, Cupeiro R, Butragueño J, et al. Strength plus endurance training and individualized diet reduce fat mass in overweight subjects: a randomized clinical trial. Int J Environ Res Public Health. 2020;17:2596.
Cabanas-Sánchez V, Duarte Junior MA, Lavie CJ, Celis-Morales C, Rodríguez-Artalejo F, Martínez-Gómez D. Physical activity and cause-specific cardiovascular mortality among people with and without cardiovascular disease: a cohort study of 0.6 million US adults. Mayo Clin Proc. 2024;99:564–77.
Martinez-Gomez D, Rodriguez-Artalejo F, Ding D, Ekelund U, Cabanas-Sanchez V. Trends in the association between meeting the physical activity guidelines and risk of mortality in US adults. Prog Cardiovasc Dis. 2024;83:116–23.
Acknowledgements
We acknowledge the participants for their contribution.
Author information
Authors and Affiliations
Contributions
ATB, JC, and LLA contributed to the study conception and design. Material preparation and data collection were performed by LLA. Data analysis was performed by LLA. The first draft of the manuscript was written by ATB, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The SHARE project, operating under the umbrella of the Max Planck Society since 2011, has had its research-ethical assessments reviewed and approved by the Ethics Council of the Max Planck Society, which carefully evaluated the project’s design and subprojects, including the SHARE Corona Survey and the collection of dried blood spots, ensuring compliance with ethical research principles.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tur-Boned, A., Andersen, L.L., López-Bueno, R. et al. Beyond body mass index: the role of muscle strength in reducing mortality risk in older adults with severe obesity – multi-country cohort study. Eur J Clin Nutr 79, 787–792 (2025). https://doi.org/10.1038/s41430-025-01616-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01616-y