Abstract
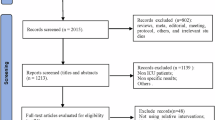
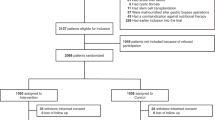
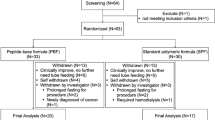
The incidence of malnutrition in patients undergoing abdominal surgery exceeds 50%, and postoperative nutritional support is crucial for improving patient outcomes. While Enhanced Recovery After Surgery (ERAS) protocols highlight early nutrition support, their impact on different nutritional strategies remains unclear. This study assessed the effects and safety of enteral nutrition (EN), early-supplemental parenteral nutrition (E-SPN), late-supplemental parenteral nutrition (L-SPN), and total parenteral nutrition (TPN) through network meta-analysis. Three databases were searched to obtain randomized controlled trials involving four interventions for postoperative nutritional supportive therapy in abdominal surgical patients. We used The Cochrane Handbook tool (2.0) to assess the risk bias of included studies. The primary outcome was the occurrence of postoperative adverse events. Network meta-analysis was performed using STATA 14. A total of 48 studies involving 6277 patients were included. Network meta-analysis showed that compared with other nutritional therapy E-SPN was likely more effective than other modalities in terms of reduction of postoperative adverse events (OR = 3.02, 95% CI: 1.81–5.02), infectious adverse events (OR = 3.12, 95% CI: 1.59–6.15), non-infectious adverse events (OR = 2.47, 95% CI: 1.14–5.34), shortening the resumption of exhaust time (SMD = 0.98, 95% CI: 0.59–1.36), and improvement of serum albumin (SMD = −2.74, 95% CI: −4.98–0.50). The final surface under the cumulative ranking curve value indicated that E-SPN achieved the best effect in those outcomes. The obtained results support using E-SPN in patients undergoing abdominal surgery, which might reduce adverse events, shorten recovery time, and improve patient outcomes. However, since serum albumin is primarily an inflammatory marker rather than a direct indicator of nutritional status, its role in evaluating SPN benefits should be interpreted with caution. Further research is needed to assess SPN’s effectiveness in patients undergoing surgery according to an ERAS protocol.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A. Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections - results from a National Quality Registry. Clin Nutr. 2020;39:1593–9. https://doi.org/10.1016/j.clnu.2019.07.003.
Lim SL, Ong KC, Chan YH, Loke WC, Ferguson M, Daniels L. Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr. 2012;31:345–50. https://doi.org/10.1016/j.clnu.2011.11.001.
Koterazawa Y, Oshikiri T, Takiguchi G, Urakawa N, Hasegawa H, Yamamoto M, et al. Severe weight loss after minimally invasive oesophagectomy is associated with poor survival in patients with oesophageal cancer at 5 years. BMC Gastroenterol. 2020;20:407 https://doi.org/10.1186/s12876-020-01543-1.
Ford KL, Prado CM, Weimann A, Schuetz P, Lobo DN. Unresolved issues in perioperative nutrition: a narrative review. Clin Nutr. 2022;41:1578–90. https://doi.org/10.1016/j.clnu.2022.05.015.
Doley J. Enteral nutrition overview. Nutrients. 2022;14. https://doi.org/10.3390/nu14112180.
Quiroz-Olguín G, Gutiérrez-Salmeán G, Posadas-Calleja JG, Padilla-Rubio MF, Serralde-Zúñiga AE. The effect of enteral stimulation on the immune response of the intestinal mucosa and its application in nutritional support. Eur J Clin Nutr. 2021;75:1533–9. https://doi.org/10.1038/s41430-021-00877-7.
Irani JL, Hedrick TL, Miller TE, Lee L, Steinhagen E, Shogan BD, et al. Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American society of colon and rectal surgeons and the society of American gastrointestinal and endoscopic surgeons. Dis Colon Rectum. 2023;66:15–40. https://doi.org/10.1097/dcr.0000000000002650.
Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN practical guideline: clinical nutrition in surgery. Clin Nutr. 2021;40:4745–61. https://doi.org/10.1016/j.clnu.2021.03.031.
Chinese Society of Parenteral and Enteral Nutrition (CSPEN). Guideline for clinical application of parenteral and enteral nutrition in adults patients in China (2023 edition). Natl Med J China. 2023;103:946–74. https://doi.org/10.3760/cma.j.cn112137-20221116-02407.
Yeh DD, Fuentes E, Quraishi SA, Cropano C, Kaafarani H, Lee J, et al. Adequate nutrition may get you home: effect of caloric/protein deficits on the discharge destination of critically Ill surgical patients. JPEN J Parenter Enter Nutr. 2016;40:37–44. https://doi.org/10.1177/0148607115585142.
Jiang Z, Wen C, Wang C, Zhao Z, Bo L, Wan X, et al. Plasma metabolomics of early parenteral nutrition followed with enteral nutrition in pancreatic surgery patients. Sci Rep. 2019;9:18846. https://doi.org/10.1038/s41598-019-55440-z.
Oshima T, Heidegger CP, Pichard C. Supplemental parenteral nutrition is the key to prevent energy deficits in critically Ill patients. Nutr Clin Pr. 2016;31:432–7. https://doi.org/10.1177/0884533616651754.
Compher C, Bingham AL, McCall M, Patel J, Rice TW, Braunschweig C, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: the American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enter Nutr. 2022;46:12–41. https://doi.org/10.1002/jpen.2267.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: society of critical care medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2016;40:159–211. https://doi.org/10.1177/0148607115621863.
Bost RB, Tjan DH, van Zanten AR. Timing of (supplemental) parenteral nutrition in critically ill patients: a systematic review. Ann Intensive Care. 2014;4:31. https://doi.org/10.1186/s13613-014-0031-y.
Gao X, Liu Y, Zhang L, Zhou D, Tian F, Gao T, et al. Effect of early vs late supplemental parenteral nutrition in patients undergoing abdominal surgery: a randomized clinical trial. JAMA Surg. 2024;157:384–93. https://doi.org/10.1001/jamasurg.2022.0269.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. https://doi.org/10.7326/m14-2385.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898 https://doi.org/10.1136/bmj.l4898.
Kavanagh BP. The GRADE system for rating clinical guidelines. PLoS Med. 2009;6:e1000094 https://doi.org/10.1371/journal.pmed.1000094.
Wu GZ, Gao SQ, Mao GJ, Luo JS. Clinical efficacy of different nutritional methods in patients after laparoscopic radical surgery for distal gastric cancer. World Chin J Digestol. 2020;28:898–903. https://doi.org/10.11569/wcjd.v28.i18.898.
Huang D, Sun Z, Huang J, Shen Z. Early enteral nutrition in combination with parenteral nutrition in elderly patients after surgery due to gastrointestinal cancer. Int J Clin Exp Med. 2015;8:13937–45.
Liu ZH, Su GQ, Zhang SY, Zhang JB, Huang XR. Study on early postoperative nutritional support in elderly patients with gastric cancer. Chin J Gastrointest Surg. 2013;16:1063–6.
Nagata S, Fukuzawa K, Iwashita Y, Kabashima A, Kinoshita T, Wakasugi K et al. Comparison of enteral nutrition with combined enteral and parenteral nutrition in post-pancreaticoduodenectomy patients: a pilot study. Nutr J. 2009;8. https://doi.org/10.1186/1475-2891-8-24
Xu B, Chen H, Zhang Q, Chen P. Supplemental parenteral nutrition improves patient outcomes after esophageal cancer surgery: a single-center randomized controlled study. Medicine. 2022;101:e31893 https://doi.org/10.1097/MD.0000000000031893.
Kang WM, Yu JC, Ma ZQ, Wang J, Ge JN, Li ZT. Comparison of clinical efficacy between standard sequential early enteral nutrition plus parenteral nutrition and parenteral nutrition support in patients undergoing gastrointestinal surgery: a clinical randomized controlled trial. Chin J Clin Nutr. 2011;19:148–53. https://doi.org/10.3760/cma.j.issn.1674-635X.2011.03.004.
Chen H, Jia JG, Li F, Yang L, Yang P, Sun JB. Effects of early postoperative nutritional support on immune system and inflammatory responses after gastrointestinal surgey. Chin J Clin Nutr. 2006;14:144–8.
Jiang YJ, Kong XJ, Tian ZB, Wang PG. Comparative studies on application of combination of postoperative enteral nutrition and parenteral nutrition with total parenteral nutrition after gastrointestinal surgery. Chin J Clin Nutr. 2006;14:18–21.
Lidder P, Flanagan D, Fleming S, Russell M, Morgan N, Wheatley T, et al. Combining enteral with parenteral nutrition to improve postoperative glucose control. Brit J Nutr. 2010;103:1635–1641. https://doi.org/10.1017/S0007114509993631.
Chu L, Ren Y, Zhang L, Yu X. Evaluation of effects of nutritional risk assessment and enteral and parenteral nutritional interventions after esophageal cancer surgery. Int J Clin Exp Med. 2018;11:5110–6.
Liu QY, Li JF, Liang X. Comparison of the clinical efficacy between the early enteral nutrition and parenteral nutrition on patients after liver transplantation. Acta Med Mediterr. 2018;34:859–63. https://doi.org/10.19193/0393-6384_2018_3_131.
Gabor S, Renner H, Matzi V, Ratzenhofer B, Lindenmann J, Sankin O, et al. Early enteral feeding compared with parenteral nutrition after oesophageal or oesophagogastric resection and reconstruction. Brit J Nutr. 2005;93:509–13. https://doi.org/10.1079/BJN20041383.
Malhotra A, Mathur AK, Gupta S. Early enteral nutrition after surgical treatment of gut perforations: a prospective randomised study. J Postgrad Med. 2004;50:102–6.
Wang J, Zhao J, Zhang Y, Liu C. Early enteral nutrition and total parenteral nutrition on the nutritional status and blood glucose in patients with gastric cancer complicated with diabetes mellitus after radical gastrectomy. Exp Therapeutic Med. 2018;16:321–7. https://doi.org/10.3892/etm.2018.6168.
Fujita T, Daiko H, Nishimura M. Early enteral nutrition reduces the rate of life-threatening complications after thoracic esophagectomy in patients with esophageal cancer. Eur Surg Res. 2012;48:79–84. https://doi.org/10.1159/000336574.
Perinel J, Mariette C, Dousset B, Sielezneff I, Gainant A, Mabrut JY, et al. Early enteral versus total parenteral nutrition in patients undergoing pancreaticoduodenectomy a randomized multicenter controlled trial (Nutri-DPC). Ann Surg. 2016;264:731–7. https://doi.org/10.1097/SLA.0000000000001896.
Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, Di Carlo V. Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Critical Care Med. 2001;29:242–8. https://doi.org/10.1097/00003246-200102000-00003.
Alivizatos V, Athanasopoulos P, Makris N, Karageorgos N. Early postoperative glutamine-supplemented parenteral nutrition versus enteral immunonutrition in cancer patients undergoing major gastrointestinal surgery. J B U. 2005;10:119–22.
Wu S, You D, Lu L, Tong Y, Hu Q, Jin T, et al. Effect of enteral nutrition support on the curative effect and immune system in patients with rectal cancer during fast track surgery. Int J Clin Exp Med. 2020;13:6065–73.
Liu H, Ling W, Cao H. Effects of immune-enhanced enteral nutrition and parenteral nutrition on immune and nutritional function in elderly patients with gastric cancer after total gastrectomy. J Shanghai Jiaotong Univ. 2011;31:1000–4. https://doi.org/10.3969/j.issn.1674-8115.2011.07.029.
Xiao-Bo Y, Qiang L, Xiong Q, Zheng R, Jian Z, Jian-Hua Z, et al. Efficacy of early postoperative enteral nutrition in supporting patients after esophagectomy. Minerva Chirurgica. 2014;69:37–46.
Liu C, Du Z, Lou C, Wu C, Yuan Q, Wang J, et al. Enteral nutrition is superior to total parenteral nutrition for pancreatic cancer patients who underwent pancreaticoduodenectomy. Asia Pac J Clin Nutr. 2011;20:154–60.
Li J, Ji Z, Yuan C, Zhang Y, Chen W, Ju X, et al. Limited efficacy of early enteral nutrition in patients after total gastrectomy. J Invest Surg. 2011;24:103–8. https://doi.org/10.3109/08941939.2011.557469.
Bozzetti F, Braga M, Gianotti L, Gavazzi C, Mariani L. Postoperative enteral versus parenteral nutrition in malnourished patients with gastrointestinal cancer: a randomised multicentre trial. Lancet. 2001;358:1487–92. https://doi.org/10.1016/S0140-6736(01)06578-3.
Hamai Y, Hihara J, Emi M, Ibuki Y, Kurokawa T, Yoshikawa T, et al. Prospective randomized trial of early postoperative enteral and total parenteral nutrition for treating esophageal cancer. Anticancer Res. 2021;41:6237–46. https://doi.org/10.21873/anticanres.15444.
Kamei H, Hachisuka T, Nakao M, Takagi K. Quick recovery of serum diamine oxidase activity in patients undergoing total gastrectomy by oral enteral nutrition. Am J Surg. 2005;189:38–43. https://doi.org/10.1016/j.amjsurg.2004.03.015.
Boelens PG, Heesakkers FF, Luyer MD, van Barneveld KW, de Hingh IH, Nieuwenhuijzen GA, et al. Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg. 2014;259:649–655. https://doi.org/10.1097/SLA.0000000000000288.
Chen L, Zheng S, Xie Q, Huang L, Yin G. The effect of different nutritional nursing support on the nutritional status and disease recovery of elderly patients with gastrointestinal tumors during the perioperative period. Comput Math Methods Med. 2022;2022:4977922. https://doi.org/10.1155/2022/4977922.
Wu PR, Xu L, Zhang ZM. Comparative study of postoperative early enteral nutrition and parenteral nutrition in esophageal carcinoma. Chin J Gastrointest Surg. 2006;9:320–2.
Xu HB, Huang HP. Clinical application of early enteral nutrition support after operation of esophagus carcinoma. Tumor. 2007;27:832–4.
Wu GH, Zhang YW, Pan HT, Zhang B, Liu ZH, Wu ZH. A randomized controlled trial of postoperative artificial nutrition in malnourished patients with gastrointestinal cancer. Chin J Gastrointest Surg. 2007;10:546–9.
Dong GH, Cai JF, Hao J, Zhong QG, Li YJ. Effect of early enteral nutrition on immune function of the patients after operation for severe abdominal trauma. Chin J Gastrointest Surg. 2006;9:145–7.
Li B, Liu HY, Guo SH, Sun P, Gong FM, Jia BQ. Impact of early enteral and parenteral nutrition on prealbumin and high-sensitivity C-reactive protein after gastric surgery. Genetics Mol Res. 2015;14:7130–5. https://doi.org/10.4238/2015.June.29.6.
Seike J, Tangoku A, Yuasa Y, Okitsu H, Kawakami Y, Sumitomo M. The effect of nutritional support on the immune function in the acute postoperative period after esophageal cancer surgery: Total parenteral nutrition versus enteral nutrition. J Med Investig. 2011;58:75–82. https://doi.org/10.2152/jmi.58.75.
Zhao G, Cao S, Zhang K, Xin Y, Han J, Dong Q, et al. Effect of early enteral nutrition on immune response and clinical outcomes after esophageal cancer surgery. Chin J Gastrointest Surg. 2014;17:356–60. https://doi.org/10.3760/cma.j.issn.1671-0274.2014.04.014.
Luo Z, Wang J, Zhang Z, Li H, Huang L, Qiao Y, et al. Efficacy of early enteral immunonutrition on immune function and clinical outcome for postoperative patients with gastrointestinal cancer. JPEN J Parenter Enter Nutr. 2018;42:758–65. https://doi.org/10.1177/0148607117715439.
Yu HZ, Long X, Liu CM, Cao YL, Li SX, Wu XQ. Impact of enteral nutrition or parenteral nutrition in post-operative colorectal cancer patients on viscera organ functions and “passing wind” time. Chin J Clin Nutr. 2009;17:268–70. https://doi.org/10.3760/cma.j.issn.1674-635X.2009.05.003.
Feng HQ, Dai L, Ma SH, Kang XZ, Yang YQ, Chen KN. Impact of early enteral nutrition on the intestinal motility of patients after esophagectomy. Chin J Gastrointest Surg. 2012;15:957–9. https://doi.org/10.3760/cma.j.issn.1671-0274.2012.09.023.
Gao JL, Gao W. Dou ZX. Effect of early postoperative enteral nutrition on nutrition status and immune function in gastric cancer patients. World Chin J Digestol. 2015;23:3451–5. https://doi.org/10.11569/wcjd.v23.i21.3451.
Wu W, Zhong M, Zhu DM, Song JQ, Huang JF, Wang Q, et al. Effect of early full-calorie nutrition support following esophagectomy: a randomized controlled trial. J Parenter Enter Nutr. 2017;41:1146–54. https://doi.org/10.1177/0148607116651509.
Tomova R, Tzaneva P, Nikolov M, Simeonov V. Interpretation of data in patients with enteral and parenteral nutrition. Central Eur J Med. 2012;7:720–8. https://doi.org/10.2478/s11536-012-0077-x.
Kang WM, Yu JC, Zhang Q, Ke MY, Qian JM. Effects of enteral and parenteral nutrition on gastroenteric hormones and gastric motility after subtotal gastrectomy. Chin Med Sci J. 2008;23:113–6. https://doi.org/10.1016/S1001-9294(09)60022-5.
Li B, Liu HY, Guo SH, Sun P, Gong FM, Jia BQ. The postoperative clinical outcomes and safety of early enteral nutrition in operated gastric cancer patients. J B U. 2015;20:468–72.
Guo JC, Li J, Hu Y, Zhang TP, Liao Q, Dai MH, et al. The role of perioperative enteral and parenteral nutrition treatment in pancreatic cancer: a multicenter, prospective randomized controlled trial. Chin J Surg. 2013;51:987–90. https://doi.org/10.3760/cma.j.issn.0529-5815.2013.11.003.
Hu QG. Zheng QC. The influence of enteral nutrition in postoperative patients with poor liver function. World J Gastroenterol. 2003;9:843–6. https://doi.org/10.3748/wjg.v9.i4.843.
Xie TP, Zhao YF, Peng L, Zhu J, Li Q. Effect of early enteral nutrition on liver functions in patients following esophageal cancer surgery. Chin J Clin Nutr. 2007;15:95–98.
Wang SY, Hung YL, Hsu CC, Hu CH, Huang RY, Sung CM et al. Optimal perioperative nutrition therapy for patients undergoing pancreaticoduodenectomy: a systematic review with a component network meta-analysis. Nutrients. 2021;13; https://doi.org/10.3390/nu13114049.
Chen R, Yin W, Gao H, Zhang H, Huang Y. The effects of early enteral nutrition on the nutritional statuses, gastrointestinal functions, and inflammatory responses of gastrointestinal tumor patients. Am J Transl Res. 2021;13:6260–9.
Berlana D. Parenteral nutrition overview. Nutrients. 2022;14. https://doi.org/10.3390/nu14214480.
Yan X, Zhou FX, Lan T, Xu H, Yang XX, Xie CH, et al. Optimal postoperative nutrition support for patients with gastrointestinal malignancy: a systematic review and meta-analysis. Clin Nutr. 2017;36:710–21. https://doi.org/10.1016/j.clnu.2016.06.011.
Seo JM, Joshi R, Chaudhary A, Hsu HS, Trung LV, Inciong JF, et al. A multinational observational study of clinical nutrition practice in patients undergoing major gastrointestinal surgery: the Nutrition Insights Day. Clin Nutr ESPEN. 2021;41:254–60. https://doi.org/10.1016/j.clnesp.2020.11.029.
Evans DC, Corkins MR, Malone A, Miller S, Mogensen KM, Guenter P, et al. The use of visceral proteins as nutrition markers: an ASPEN position paper. Nutr Clin Pr. 2021;36:22–28. https://doi.org/10.1002/ncp.10588.
Burcharth J, Falkenberg A, Schack A, Ekeloef S, Gögenur I. The effects of early enteral nutrition on mortality after major emergency abdominal surgery: a systematic review and meta-analysis with Trial Sequential Analysis. Clin Nutr. 2021;40:1604–12. https://doi.org/10.1016/j.clnu.2021.02.050.
Sim J, Hong J, Na EM, Doo S, Jung YT. Early supplemental parenteral nutrition is associated with reduced mortality in critically ill surgical patients with high nutritional risk. Clin Nutr. 2021;40:5678–83. https://doi.org/10.1016/j.clnu.2021.10.008.
Author information
Authors and Affiliations
Contributions
DR Kong, TW Wang and JQ Huang designed the study, TW Wang, JQ Huang, M Deng and Z Shang performed the study, TW Wang analyzed the data and drafted the manuscript, JQ Huang, JD Su and XY Duan participated amending the manuscript, DR Kong reviewed and edited. All authors have read and agreed to published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, T., Huang, J., Shang, Z. et al. Efficacy and safety of nutrition therapy for patients undergoing abdominal surgery: a systematic review and network meta-analysis. Eur J Clin Nutr 79, 1078–1086 (2025). https://doi.org/10.1038/s41430-025-01637-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01637-7