Abstract
Background and aims
Ulcerative colitis (UC) and Crohn’s disease (CD) are inflammatory bowel diseases (IBD) with varying clinical presentations. Current literature lacks specific dietary recommendations, though diets may serve as potential tools.
Methods
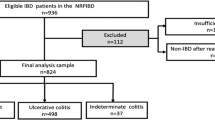
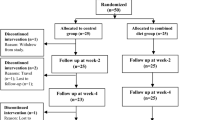
This study, conducted at IRCCS Ca’ Granda Foundation Ospedale Maggiore Policlinico of Milan from April 2020 to July 2022, aimed to evaluate the diets of UC and CD patients, focusing on preferred and avoided foods.
Results
Results showed 67.4% and 80.9% of participants in remission by Mayo and HBI scores, respectively, with normal nutritional status and higher weight in CD versus UC patients and controls. Lactose-free diets were most common (21.3% UC, 17.4% CD, 11.6% controls), followed by gluten-free diets (23.4% UC, 13.4% CD, 9.3% controls). Low-FODMAPS diet adoption was minimal. Fibre avoidance was notable in CD (52%) and UC (45%) versus controls (5%). Pasta and bread consumption were high across groups. No dietary associations with disease activity or intergroup differences were found.
Conclusions
The study population exhibited mild to moderate disease activity, normal nutritional status and prevalent dietary restrictions affecting nutrient intake and quality of life. Lactose-free diets were frequently employed, while gluten-free and low-FODMAPS diets were less common. Encouraging supervised fibre intake is recommended to prevent microbiota alterations negatively impacting intestinal health and homeostasis in IBD patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Silaghi A, Constantin VD, Socea B, Fierbinteanu-Braticevici C, Ionescu AG, Smarandache CG, et al. Inflammatory bowel disease: pathogenesis, diagnosis and current therapeutic approach. J Mind Med Sci. 2022;9:56–77.
Zhang YZ, Li YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014;20:91–99.
Passarella A, Grewal P, Vrabie R Diagnosis and monitoring in inflammatory bowel disease: who, when, where, and how. In: Rajapakse R, Ed. Inflammatory bowel disease pathogenesis, diagnosis and management, softcover edn. Port Jefferson, NY: Humana Press, 2022:25–61.
Advani R, Rajapakse R Extraintestinal manifestations in inflammatory bowel disease. In: Rajapakse R, Ed. Inflammatory bowel disease pathogenesis, diagnosis and management, softcover edn. Port Jefferson, NY: Humana Press, 2022:115–36.
Rogler G, Singh A, Kavanaugh A, Rubin DT, Motoya S, Ahmad T, et al. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161:1118–32.
Yu YR, Rodriguez JR. Clinical presentation of Crohn’s, ulcerative colitis, and indeterminate colitis: symptoms, extraintestinal manifestations, and disease phenotypes. Semin Pediatr Surg. 2017;26:349–55.
Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ, Colombel J-F, et al. Ulcerative colitis. Lancet. 2012;380:1606–19.
van Rheenen PF, Aloi M, Assa A, Braegger C, Bronsky J, Chartone-Souza D, et al. The medical management of paediatric Crohn’s disease: an ECCO-ESPGHAN guideline update. J Crohns Colitis. 2020;7:jjaa161.
Mitrev N, Huang H, Hannah B, Jacobson K, Quigley EMM, Hansen J, et al. Review of exclusive enteral therapy in adult Crohn’s disease. BMJ Open Gastroenterol. 2021;8:e000745.
Doley J. Enteral nutrition overview. Nutrients. 2022;14:2180.
Bischoff SC, Bager P, Escher J, Felice C, Heuschkel R, Kierkus J, et al. ESPEN guideline on clinical nutrition in inflammatory bowel disease. Clin Nutr. 2023;42:352–79.
Roncoroni L, Gori R, Elli L, Di Sabatino A, Roda G, Vecchi M, et al. Nutrition in patients with inflammatory bowel diseases: a narrative review. Nutrients. 2022;14:751.
Herfarth HH, Martin CF, Sandler RS, Kappelman MD, Long MD, Zong G, et al. Prevalence of a gluten-free diet and improvement of clinical symptoms in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2014;20:1194–7.
Day AS, Yao CK, Costello SP, Andrews JM, Lemberg DA, Keenan HA, et al. Food avoidance, restrictive eating behaviour and association with quality of life in adults with inflammatory bowel disease: a systematic scoping review. Appetite. 2021;167:105650.
Gerasimidis K, Whelan K, Russell RK, Thomas AG Inflammatory bowel disease nutritional consequences. In: Lomer M, Whelan K, eds. Advanced nutrition and dietetics in gastroenterology. Chichester: Wiley Blackwell; 2014:180-90.
Dhaliwal A, Quinlan JI, Overthrow K, Bartnikas L, Larson J, Cheifetz AS, et al. Sarcopenia in inflammatory bowel disease: a narrative overview. Nutrients. 2021;13:656.
Mazzeo T, Roncoroni L, Lombardo V, Norsa L, Branchi F, Elli L, et al. Evaluation of a modified Italian EPIC food frequency questionnaire for individuals with celiac disease. J Acad Nutr Diet. 2016;116:1810–6.
Sahu P, Kedia S, Ahuja V, Midha V, Shukla R, Paul J, et al. Diet and nutrition in the management of inflammatory bowel disease. Indian J Gastroenterol. 2021;40:253–64.
Lim HS, Kim SK, Hong SJ. Food elimination diet and nutritional deficiency in patients with inflammatory bowel disease. Clin Nutr Res. 2018;7:48–55.
McDowell C, Farooq U, Haseeb M Inflammatory bowel disease. In: StatPearls [Internet]. 2023 Aug 4.
Spooren CEGM, Wintjen DSJ, de Jong MJ, Verspaget HW, Cornillie FJ, Russell RK, et al. Risk of impaired nutritional status and flare occurrence in IBD outpatients. Dig Liver Dis. 2019;51:1265–9.
Nguyen GC, Munsell M, Harris ML. Nationwide prevalence and prognostic significance of clinically diagnosable protein-calorie malnutrition in hospitalized inflammatory bowel disease patients. Inflamm Bowel Dis. 2008;14:1105–11.
Skrzypczak D, Ratajczak AE, Szymczak-Tomczak A, Nogaj J, Chaplin S, Dzieckońska-Kubiak B, et al. A vicious cycle of osteosarcopenia in inflammatory bowel diseases – aetiology, clinical implications and therapeutic perspectives. Nutrients. 2021;13:293.
Naruse T, Sato H, Takahashi K, Sato C, Kojima Y, Kawata Y et al. Association between Clinical Characteristics and Sarcopenia or Sarcopenic Obesity in Crohn's Disease. Intern Med. 2025;64:1451–58.
Nguyen DL, Limketkai BN, Medici V, Chak A, Lewis JD, Kane SV, et al. Nutritional strategies in the management of adult patients with inflammatory bowel disease: dietary considerations from active disease to disease remission. Curr Gastroenterol Rep. 2016;18:55.
Damas OM, Garces L, Abreu MT. Diet as adjunctive treatment for inflammatory bowel disease: review and update of the latest literature. Curr Treat Options Gastroenterol. 2019;17:313–25.
Slavin J. Fiber and prebiotics: mechanisms and health benefits. Nutrients. 2013;5:1417–35.
Maslowski KM, Mackay CR. Diet, gut microbiota and immune responses. Nat Immunol. 2011;12:5–9.
Parada Venegas D, De la Fuente MK, Landskron G, González MJ, Quera R, Dijkstra G, et al. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;10:277.
Macfarlane S, Macfarlane GT. Regulation of short-chain fatty acid production. Proc Nutr Soc. 2003;62:67–72.
Lewis JD, Abreu MT. Diet as a trigger or therapy for inflammatory bowel diseases. Gastroenterology. 2017;152:398–414.
Kim S, Kim J-H, Park BO, Lee CH, Kim H-J, Cho JH, et al. Perspectives on the therapeutic potential of short-chain fatty acid receptors. BMB Rep. 2014;47:173–8.
Koleva PT, Valcheva RS, Sun X, Poutahidis T, Erdman SE, Horvath K, et al. Inulin and fructo-oligosaccharides have divergent effects on colitis and commensal microbiota in HLA-B27 transgenic rats. Br J Nutr. 2012;108:1633–43.
Faghfoori Z, Shakerhosseini R, Navai L, Soltani O, Esmaili F, Hekmatdoost A, et al. Effects of an oral supplementation of germinated barley foodstuff on serum CRP level and clinical signs in patients with ulcerative colitis. Health Promot Perspect. 2014;4:116–21.
Fritsch J, Garces L, Quintero MA, Roncoroni L, Elli L, Gasbarrini A, et al. Low-fat, high-fiber diet reduces markers of inflammation and dysbiosis and improves quality of life in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2021;19:1189–99.
Benjamin JL, Hedin CR, Koutsoumpas A, Ng SC, McCarthy NE, Hart AL, et al. Randomised, double-blind, placebo-controlled trial of fructo-oligosaccharides in active Crohn’s disease. Gut. 2011;60:923–9.
Limketkai BN, Iheozor-Ejiofor Z, Gjuladin Hellon T, Roncoroni L, Shea-Donohue T, Kane SV, et al. Dietary interventions for induction and maintenance of remission in inflammatory bowel disease. Cochrane Database Syst Rev. 2019;2:CD012839.
Lewis JD, Sandler RS, Brotherton C, Li X, Thomas AG, Black C, et al. A randomised trial comparing the specific carbohydrate diet to a Mediterranean diet in adults with Crohn’s disease. Gastroenterology. 2021;161:837–.e9.
Levine A, Wine E, Assa A, Sigall-Boneh R, Shaoul R, Cohen S, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomised controlled trial. Gastroenterology. 2019;157:440–.e8.
Yanai H, Levine A, Hirsch A, Lomer M, Berry L, Sigall-Boneh R, et al. The Crohn’s disease exclusion diet for induction and maintenance of remission in adults with mild-to-moderate Crohn’s disease (CDED-AD): an open-label, pilot, randomised trial. Lancet Gastroenterol Hepatol. 2022;7:49–59.
Cox SR, Lindsay JO, Fromentin S, Faiz O, Brodod S, Ijaz UZ, et al. Effects of low FODMAP diet on symptoms, fecal microbiome, and markers of inflammation in patients with quiescent inflammatory bowel disease in a randomised trial. Gastroenterology. 2020;158:176–88.
Gearry RB, Irving PM, Barrett JS, Chambers S, Xuewei Q, Bach E, et al. Reduction of dietary poorly absorbed short-chain carbohydrates (FODMAPs) improves abdominal symptoms in patients with inflammatory bowel disease – a pilot study. J Crohns Colitis. 2009;3:8–14.
Prince AC, Myers CE, Joyce T, Irving PM, Lomer MCE, Brostoff J, et al. Fermentable carbohydrate restriction (low FODMAP diet) in clinical practice improves functional gastrointestinal symptoms in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1129–36.
Czuber-Dochan W, Morgan M, Hughes LD, Norton C, Jones CN, White S, et al. Perceptions and psychosocial impact of food, nutrition, eating and drinking in people with inflammatory bowel disease: a qualitative investigation of food-related quality of life. J Hum Nutr Diet. 2020;33:115–27.
Palamenghi L, Figliuc P, Leone S, Porta A, Vegetti F, Macchi C, et al. Food and inflammatory bowel diseases: a scoping review on the impact of food on patients’ psychosocial quality of life. Health Soc Care Community. 2022;30:1695–712.
Guadagnoli L, Mutlu EA, Doerfler B, Jackson A, Paquette M, Raskin JB, et al. Food-related quality of life in patients with inflammatory bowel disease and irritable bowel syndrome. Qual Life Res. 2019;28:2195–205.
Aswani-Omprakash T, Shah ND. Sociocultural considerations for food-related quality of life in inflammatory bowel disease. Gastroenterol Clin North Am. 2022;51:885–95.
Acknowledgements
We wish to thank ‘io e il glutine ONLUS’ for the non-financial support.
Funding
This study was partially funded by Italian Ministry of Health, Current research IRCCS.
Author information
Authors and Affiliations
Contributions
Conceptualization AS, VL, KAB, and LR; Writing-Original Draft Preparation AS, VL, KAB, RG, GG, and LR; Writing Review & Editing, LE, AC, FC, GET, and LR; Methodology LE, LR; Supervision MA, LE, and MV; Visualization FM, LD, and VM; Funding Acquisition, MV. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical considerations
The Local Ethics Committee (n. 19_2019bis) approved the study protocol according to the Helsinki Declaration.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Scricciolo, A., Lombardo, V., Bascuñán, K.A. et al. Assessment of nutritional status and eating behaviours in patients with chronic inflammatory bowel disease: a pilot study. Eur J Clin Nutr 79, 1130–1137 (2025). https://doi.org/10.1038/s41430-025-01645-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01645-7