Abstract
Objectives
Nutrition support improves ICU patients’ nutritional status and outcomes, but optimal models remain unclear. We performed a Bayesian and frequentist network meta-analysis (NMA) and systematic review to assess improvements in nutritional indicators and clinical outcomes.
Methods
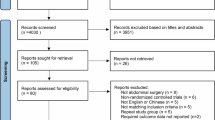
We systematically searched PubMed, Embase, Cochrane, and Web of Science up to November 23, 2023 for Randomised controlled trials (RCT), case-control studies, and cohort studies. Outcomes mainly included serum albumin values, length of hospitalization, infection rates, feeding-related complication rates and mortality. All the analyses were conducted using STATA 17.0 and R software version 4.5.1.
Results
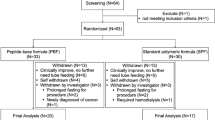
A total of 26 studies were included, enrolling 7698 critically ill ICU patients receiving four different types of nutrition support, including parenteral nutrition (PN), enteral nutrition (EN), enteral immunonutrition (EIN), and parenteral nutrition combined with enteral nutrition (PN + EN). The NMA results showed that according to SUCRA, PN + EN had the highest probability of being the most effective intervention for improving serum albumin values (SUCRA = 84.5%) and reducing infection rates (SUCRA = 83.0%) and mortality rates (SUCRA = 82.7%). PN had the highest probability of reducing the length of hospitalization (SUCRA = 77.9%), while EIN had the highest probability of reducing feeding-related complication rates (SUCRA = 81.0%).
Conclusion
The available evidence suggests that all four models of nutrition support affect the nutritional status and clinical outcomes of critically ill patients in the ICU to varying degrees. However, EN + PN appears to be the most effective approach in improving clinical outcomes and nutrition support in critically ill ICU patients. More high-quality studies are needed to validate these findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Sharma K, Mogensen KM, Robinson MK. Pathophysiology of critical illness and role of nutrition. Nutr Clin Pr. 2019;34:12–22.
Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review [formula: see text]. JPEN J Parenter Enter Nutr. 2017;41:744–58.
Zaragoza-García I, Arias-Rivera S, Frade-Mera MJ, Martí JD, Gallart E, San José-Arribas A, et al. Enteral nutrition management in critically ill adult patients and its relationship with intensive care unit-acquired muscle weakness: a national cohort study. PLoS One. 2023;18:e0286598.
Pilotto S, Agustoni F, Morelli AM, Lobascio F, Cereda E, Bironzo P, et al. Nutritional support in lung cancer: Time to combine immunonutrition with immunotherapy?. Nutrition. 2022;98:111637.
Mirhosiny M, Arab M, Shahrbabaki PM. How do physicians and nurses differ in their perceived barriers to effective enteral nutrition in the intensive care unit?. Acute Crit Care. 2021;36:342–50.
Ma M, Zheng Z, Zeng Z, Li J, Ye X, Kang W. Perioperative enteral immunonutrition support for the immune function and intestinal mucosal barrier in gastric cancer patients undergoing gastrectomy: a prospective randomised controlled study. Nutrients. 2023;15.
Reintam Blaser A, Starkopf J, Alhazzani W, Berger MM, Casaer MP, Deane AM, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2017;43:380–98.
Alsharif DJ, Alsharif FJ, Aljuraiban GS, Abulmeaty MMA. Effect of supplemental parenteral nutrition versus enteral nutrition alone on clinical outcomes in critically ill adult patients: a systematic review and meta-analysis of randomised controlled trials. Nutrients. 2020;12.
Chittawatanarat K, Pokawinpudisnun P, Polbhakdee Y. Mixed fibers diet in surgical ICU septic patients. Asia Pac J Clin Nutr. 2010;19:458–64.
Li X, Yang Y, Ma ZF, Gao S, Ning Y, Zhao L, et al. Enteral combined with parenteral nutrition improves clinical outcomes in patients with traumatic brain injury. Nutr Neurosci. 2022;25:530–6.
Reintam Blaser A, Deane AM, Preiser JC, Arabi YM, Jakob SM. Enteral feeding intolerance: updates in definitions and pathophysiology. Nutr Clin Pr. 2021;36:40–49.
Cadena AJ, Habib S, Rincon F, Dobak S. The benefits of parenteral nutrition (PN) versus enteral nutrition (EN) among adult critically ill patients: What is the evidence? A literature review. J Intensive Care Med. 2020;35:615–26.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj. 2009;339:b2700.
You SB, Ulrich CM. Ethical considerations in evaluating discharge readiness from the intensive care unit. Nurs Ethics. 2023:9697330231212338.
Alsamman MA, Alsamman S, Moustafa A, Khan MS, Steinbrunner J, Koselka H. Critical care utilization in patients with diabetic ketoacidosis, stroke, and gastrointestinal bleed: two hospitals experience. Cureus. 2019;11:e4698.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomised studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366:l4898.
Lin L, Zhang J, Hodges JS, Chu H. Performing arm-based network meta-analysis in R with the pcnetmeta Package. J Stat Softw. 2017;80.
Xu C, Niu Y, Wu J, Gu H, Zhang C. Software and package applicating for network meta-analysis: A usage-based comparative study. J Evid Based Med. 2018;11:176–83.
Bhatnagar N, Lakshmi PV, Jeyashree K. Multiple treatment and indirect treatment comparisons: An overview of network meta-analysis. Perspect Clin Res. 2014;5:154–8.
Su YX, Tu YK. Statistical approaches to adjusting weights for dependent arms in network meta-analysis. Res Synth Methods. 2018;9:431–40.
Spineli LM. An empirical comparison of Bayesian modelling strategies for missing binary outcome data in network meta-analysis. BMC Med Res Methodol. 2019;19:86.
Veroniki AA, Straus SE, Fyraridis A, Tricco AC. The rank-heat plot is a novel way to present the results from a network meta-analysis including multiple outcomes. J Clin Epidemiol. 2016;76:193–9.
Levinson M, Bryce A. Enteral feeding, gastric colonisation and diarrhoea in the critically ill patient: is there a relationship?. Anaesth Intensive Care. 1993;21:85–88.
Eyer SD, Micon LT, Konstantinides FN, Edlund DA, Rooney KA, Luxenberg MG, et al. Early enteral feeding does not attenuate metabolic response after blunt trauma. J Trauma. 1993;34:639–43. discussion 643-634.
Hasse JM, Blue LS, Liepa GU, Goldstein RM, Jennings LW, Mor E, et al. Early enteral nutrition support in patients undergoing liver transplantation. JPEN J Parenter Enter Nutr. 1995;19:437–43.
Kudsk KA, Minard G, Croce MA, Brown RO, Lowrey TS, Pritchard FE, et al. A randomised trial of isonitrogenous enteral diets after severe trauma. An immune-enhancing diet reduces septic complications. Ann Surg. 1996;224:531–40. discussion 540-533.
Watters JM, Kirkpatrick SM, Norris SB, Shamji FM, Wells GA. Immediate postoperative enteral feeding results in impaired respiratory mechanics and decreased mobility. Ann Surg. 1997;226:369–77.
Minard G, Kudsk KA, Melton S, Patton JH, Tolley EA. Early versus delayed feeding with an immune-enhancing diet in patients with severe head injuries. JPEN J Parenter Enter Nutr. 2000;24:145–9.
Pupelis G, Selga G, Austrums E, Kaminski A. Jejunal feeding, even when instituted late, improves outcomes in patients with severe pancreatitis and peritonitis. Nutrition. 2001;17:91–94.
Bertolini G, Iapichino G, Radrizzani D, Facchini R, Simini B, Bruzzone P, et al. Early enteral immunonutrition in patients with severe sepsis: results of an interim analysis of a randomised multicentre clinical trial. Intensive Care Med. 2003;29:834–40.
Martin CM, Doig GS, Heyland DK, Morrison T, Sibbald WJ. Multicentre, cluster-randomised clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT). Cmaj. 2004;170:197–204.
Klek S, Kulig J, Sierzega M, Szybinski P, Szczepanek K, Kubisz A, et al. The impact of immunostimulating nutrition on infectious complications after upper gastrointestinal surgery: a prospective, randomised, clinical trial. Ann Surg. 2008;248:212–20.
Moses V, Mahendri NV, John G, Peter JV, Ganesh A. Early hypocaloric enteral nutritional supplementation in acute organophosphate poisoning-a prospective randomised trial. Clin Toxicol (Philos). 2009;47:419–24.
Wu XM, Ji KQ, Wang HY, Li GF, Zang B, Chen WM. Total enteral nutrition in prevention of pancreatic necrotic infection in severe acute pancreatitis. Pancreas. 2010;39:248–51.
Heidegger CP, Berger MM, Graf S, Zingg W, Darmon P, Costanza MC, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet. 2013;381:385–93.
Sanghvi KP, Joshi P, Nabi F, Kabra N. Feasibility of exclusive enteral feeds from birth in VLBW infants >1200 g-an RCT. Acta Paediatr. 2013;102:e299–304.
Harvey SE, Parrott F, Harrison DA, Bear DE, Segaran E, Beale R, et al. Trial of the route of early nutritional support in critically ill adults. N Engl J Med. 2014;371:1673–84.
de Betue CT, van Steenselen WN, Hulst JM, Olieman JF, Augustus M, Mohd Din SH, et al. Achieving energy goals at day 4 after admission in critically ill children; predictive for outcome?. Clin Nutr. 2015;34:115–22.
Fan M, Wang Q, Fang W, Jiang Y, Li L, Sun P, et al. Early enteral combined with parenteral nutrition treatment for severe traumatic brain injury: effects on immune function, nutritional status and outcomes. Chin Med Sci J. 2016;31:213–20.
Mazaherpur S, Khatony A, Abdi A, Pasdar Y, Najafi F. The Effect of Continuous Enteral Nutrition on Nutrition Indices, Compared to the Intermittent and Combination Enteral Nutrition in Traumatic Brain Injury Patients. J Clin Diagn Res. 2016;10:Jc01–jc05.
Wu W, Zhong M, Zhu DM, Song JQ, Huang JF, Wang Q, et al. Effect of early full-calorie nutrition support following esophagectomy: a randomised controlled trial. JPEN J Parenter Enter Nutr. 2017;41:1146–54.
Reignier J, Boisramé-Helms J, Brisard L, Lascarrou JB, Ait Hssain A, Anguel N, et al. Enteral versus parenteral early nutrition in ventilated adults with shock: a randomised, controlled, multicentre, open-label, parallel-group study (NUTRIREA-2). Lancet. 2018;391:133–43.
Yang S, Guo J, Ni Q, Chen J, Guo X, Xue G, et al. Enteral nutrition improves clinical outcome and reduces costs of acute mesenteric ischaemia after recanalisation in the intensive care unit. Clin Nutr. 2019;38:398–406.
Srinivasan V, Hasbani NR, Mehta NM, Irving SY, Kandil SB, Allen HC, et al. Early enteral nutrition is associated with improved clinical outcomes in critically ill children: a secondary analysis of nutrition support in the heart and lung failure-paediatric insulin titration trial. Pediatr Crit Care Med. 2020;21:213–21.
Lou JQ, Li Q, Cui QW, Zhang P, Sun H, Tang H, et al. A prospective randomised controlled study on the curative effects of enteral immunonutrition support therapy in adult burn patients at nutritional risk. Chin J Burns. 2022;38:722–34.
Yang XJ, Wang XH, Yang MY, Ren HY, Chen H, Zhang XY, et al. Exploring choices of early nutritional support for patients with sepsis based on changes in intestinal microecology. World J Gastroenterol. 2023;29:2034–49.
Rao YK, Saxena R, Midha T, Rao N, Saxena V. Clinical outcome of enteral nutrition versus IV fluids in newborns on inotropes: a randomised study. J Clin Neonatol. 2020;9:261–5.
Collins N. The difference between albumin and prealbumin. Adv Ski Wound Care. 2001;14:235–6.
Moon SJ, Ko RE, Park CM, Suh GY, Hwang J, Chung CR. The effectiveness of early enteral nutrition on clinical outcomes in critically ill sepsis patients: a systematic review. Nutrients. 2023;15.
Ünal Aslan KS. Examining the nutrition, oral mucositis, and gastrointestinal system symptoms of intensive care units patients receiving enteral and parenteral nutrition. Turk J Gastroenterol. 2023;34:813–21.
Lopez-Delgado JC, Grau-Carmona T, Mor-Marco E, Bordeje-Laguna ML, Portugal-Rodriguez E, Lorencio-Cardenas C, et al. Parenteral nutrition: current use, complications, and nutrition delivery in critically ill patients. Nutrients. 2023;15.
Zhong M, Qiu Y, Pan T, Wang R, Gao Y, Wang X, et al. Improving enteral nutrition tolerance and protein intake maybe beneficial to intensive care unit patients. Sci Rep. 2023;13:21614.
Martens PJ, Gysemans C, Verstuyf A, Mathieu AC. Vitamin D’s effect on immune function. Nutrients. 2020;12.
Palesty JA, Dudrick SJ. Cachexia, malnutrition, the refeeding syndrome, and lessons from Goldilocks. Surg Clin North Am. 2011;91:653–73.
Zou B, Xi F, Yu W. Early parenteral nutrition comparing to enteral nutrition cannot reduce 28-day mortality in critically ill patients: a retrospective comparative cohort study based on the MIMIC‑IV database. Ann Transl Med. 2023;11:77.
Yu K, Guo N, Zhang D, Xia Y, Meng Y, Weng L, et al. Prevalence and risk factors of enteral nutrition intolerance in intensive care unit patients: a retrospective study. Chin Med J. 2022;135:1814–20.
Sharma SK, Rani R, Thakur K. Effect of early versus delayed parenteral nutrition on the health outcomes of critically ill adults: a systematic review. J Crit Care Med. 2021;7:160–9.
Funding
This study was supported by the Scientific Research Fund of Yunnan Provincial Department of Education (grant number 2024J0847) and the Science and Technology Program of Yunnan Province Science and Technology Department (grant number 202101BA070001-118).
Author information
Authors and Affiliations
Contributions
Conceptualization: Tingting Shi and Yunmei Chen; methodology: Tingting Shi, Ting Li, and Xiaoling Zhu; formal analysis and investigation: Tingting Shi; writing—original draft preparation: Tingting Shi; writing—review and editing: Tingting Shi, Ting Li; supervision: Yunmei Chen and Xiaoling Zhu; all authors have commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, T., Li, T., Zhu, X. et al. Comparison of the effects of different models of nutrient supply on nutritional status and clinical outcomes in ICU patients: a systematic review and network meta-analysis. Eur J Clin Nutr (2026). https://doi.org/10.1038/s41430-026-01704-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41430-026-01704-7