Abstract
It is currently unclear if next-generation sequencing (NGS) technologies can be implemented in the diagnosis setting at an affordable cost. The aim of this study was to measure the total cost of performing NGS in clinical practice in France, in both germline and somatic cancer genetics.
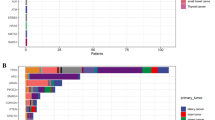
The study was performed on 15 French representative cancer molecular genetics laboratories performing NGS panels’ tests. The production cost was estimated using a micro-costing method with resources consumed collected in situ in each laboratory from a healthcare provider perspective. In addition, we used a top–down methodology for specific post-sequencing steps including bioinformatics, technical validation, and biological validation. Additional non-specific costs were also included. Costs were detailed per step of the process (from the pre-analytical phase to delivery of results), and per cost driver (consumables, staff, equipment, maintenance, overheads). Sensitivity analyses were performed.
The mean total cost of NGS for targeted gene panels was estimated to 607€ (±207) in somatic genetics and 550€ (±140) in germline oncogenetic analysis. Consumables were the highest cost driver of the sequencing process. The sensitivity analysis showed that a 25% reduction of consumables resulted in a 15% decrease in total NGS cost in somatic genetics, and 13% in germline analysis. Additional costs accounted for 30–32% of the total NGS costs.
Beyond cost assessment considerations, the diffusion of NGS technologies will raise questions about their efficiency when compared to more targeted approaches, and their added value in a context of routine diagnosis.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
15 June 2018
Since the publication of the article, it has been noted that there is an error in Table 2. Where 543€ is listed in the final column of the table, this should have been written as 550€.
References
Mardis ER. A decade’s perspective on DNA sequencing technology. Nature. 2011;470:198–203.
Tsiati AC, Norris-Kirby A, Rich RG, et al. Comparison of Sanger sequencing, pyrosequencing, and melting curve analysis for the detection of KRAS mutations: diagnostic and clinical implications. J Mol Diagn. 2010;12:425–32.
Martinez DA, Nelson MA. The next generation becomes the now generation. PLoS Genet. 2010;6:e1000906.
Sikkema-Raddatz B, Johansson LF, de Boer EN, et al. Targeted next-generation sequencing can replace Sanger sequencing in clinical diagnostics. Hum Mutat. 2013;34:1035–42.
Boyd SD. Diagnostic applications of high-throughput DNA sequencing. Annu Rev Pathol. 2013;8:381–410.
Gagan J, Van Allen EM. Next-generation sequencing to guide cancer therapy. Genome Med. 2015;7:80.
French National Cancer Institute (INCa). Molecular Genetics centres activity 2015. http://lesdonnees.e-cancer.fr/Themes/Soins/Les-tests-de-genetique-somatique.
Fineberg HV. Shattuck Lecture. A successful and sustainable health system--how to get there from here. N Engl J Med. 2012;366:1020–1027.
Armstrong K. Can genomics bend the cost curve? JAMA. 2012;307:1031–32.
Johansen Taber KA, Dickinson BD, Wilson M. The promise and challenges of next-generation genome sequencing for clinical care. JAMA Intern Med. 2014;174:275–80.
Christensen KD, Dukhovny D, Siebert U, Green RC. Assessing the costs and cost-effectiveness of genomic sequencing. J Pers Med. 2015;5:470–86.
Douglas MP, Ladabaum U, Pletcher MJ, Marshall DA, Phillips KA. Economic evidence on identifying clinically actionable findings with whole genome sequencing: a scoping review. Genet Med. 2016;18:111–6.
Hartman M, Martin AB, Lassman D, Catlin A, National Health Expenditure Accounts Team. National health spending in 2013: growth slows, remains in step with the overall economy. Health Aff. 2015;34:150–60..
Feero WG, Wicklund C, Veenstra DL. The economics of genomic medicine: insights from the IOM Roundtable on Translating Genomic-Based Research for Health. JAMA. 2013;309:1235–6.
Mardis ER. Anticipating the $1,000 genome. Genome Biol. 2006;7:112.
Hayden EC. Technology: the $1,000 genome. Nature. 2014;507:294–5.
Nimwegen KJM, van, Soest RA, van, Veltman JA, et al. Is the $1000 genome as near as we think? A cost analysis of next-generation sequencing. Clin Chem. 2016;62:1458–64.
Buchanan J, Wordsworth S, Schuh A. Issues surrounding the health economic evaluation of genomic technologies. Pharmacogenomics. 2013;14:1833–47.
Fugel H-J, Nuijten M, Postma M, Redekop K. Economic evaluation in stratified medicine: methodological issues and challenges. Front Pharmacol. 2016;7:113.
Frank M, Prenzler A, Eils R, Graf von der Schulenburg J-M. Genome sequencing: a systematic review of health economic evidence. Health Econ Rev. 2013;3:29.
Sabatini LM, Mathews C, Ptak D, et al. Genomic sequencing procedure microcosting analysis and health economic cost-impact analysis: a report of the association for molecular pathology. J Mol Diagn. 2016;18:319–28.
Tan SS, Rutten FFH, van Ineveld BM, Redekop WK, Hakkaart-van Roijen L, Comparing methodologies for the cost estimation of hospital services. Eur J Health Econ. 2009;10:39–45.
Evans JP, Dale DC, Fomous C. Preparing for a consumer-driven genomic age. N Engl J Med. 2010;363:1099–103.
Dietel M, Jöhrens K, Laffert MV, et al. A 2015 update on predictive molecular pathology and its role in targeted cancer therapy: a review focussing on clinical relevance. Cancer Gene Ther. 2015;22:417–30.
Wetterstrand KA. DNA Sequencing Costs: Data from the NHGRI Genome Sequencing Program (GSP). www.genome.gov/sequencingcostsdata.
van Amerongen RA, Retèl VP, Coupé VM, Nederlof PM, Vogel MJ, van Harten WH. Next-generation sequencing in NSCLC and melanoma patients: a cost and budget impact analysis. Ecancermedicalscience. 2016;10:684.
Plöthner M, Frank M, von der Schulenburg J-MG. Cost analysis of whole genome sequencing in German clinical practice. Eur J Health Econ. 2017;18:623–33.
Mardis E, Raison C. Next-generation sequencing, cancer and molecular diagnostics: an interview with Elaine Mardis. Expert Rev Mol Diagn. 2015;15:449–50.
Stein LD. The case for cloud computing in genome informatics. Genome Biol. 2010;11:207.
Muir P, Li S, Lou S, et al. The real cost of sequencing: scaling computation to keep pace with data generation. Genome Biol. 2016;17. https://doi.org/10.1186/s13059-016-0917-0.
Crawford JM, Bry L, Pfeifer J, et al. The business of genomic testing: a survey of early adopters. Genet Med. 2014;16:954–61.
Deverka PA, Dreyfus JC. Clinical integration of next generation sequencing: coverage and reimbursement challenges. J Law Med Ethics. 2014;42:22–41.
Van den Bulcke M. Tests de Panels de gènes par Next Generation Sequencing pour un traitement ciblé en oncologie et en hémato-oncologie – Synthèse - KCE_240Bs_NGS_traitement_cible_Synthese.pdf. https://kce.fgov.be/sites/default/files/page_documents/KCE_240Bs_NGS_traitement_cible_Synthese.pdf. Accessed 13 Apr 2017.
Evans BJ. The limits of FDA’s authority to regulate clinical research involving high-throughput DNA sequencing. Food Drug Law J. 2015;70:259–87.
Bennette CS, Gallego CJ, Burke W, Jarvik GP, Veenstra DL. The cost-effectiveness of returning incidental findings from next-generation genomic sequencing. Genet Med. 2015;17:587–95.
Phillips KA, Ann Sakowski J, Trosman J, Douglas MP, Liang S-Y, Neumann P. The economic value of personalized medicine tests: what we know and what we need to know. Genet Med. 2014;16:251–7.
Acknowledgements
We are grateful to all the staff of the laboratories involved in this study that participated in data collection, and we thank especially the laboratories that allowed site visits. In somatic genetics, these laboratories were: Gustave Roussy: Biopathology integrated genetic platform Molecular Pathology; Angers University Hospital; Plateforme SNP, Transcriptom et Epigénomique; Comprehensive Cancer Center Curie, Paris; Unité de Parmacogénomique; Service de Génétique; Rennes University Hospital; Cancer Somatic Genetics Laboratory; Lille University Hospital; Cancer Molecular Genetic Centre; Lille University Hospital; Laboratory of Oncohaematology; Department of Biology-Pathology-Genetics; Comprehensive Cancer Center Bergonié, Bordeaux; Molecular Pathology Unit. In germline genetics, these laboratories were: Lille University Hospital; Digestive Molecular Oncogenetic Unit; Comprehensive Cancer Centre CRLCC François Baclesse, Caen; Cancer Biology and Genetics Laboratory; Comprehensive Cancer Center Curie, Paris; Unité Génétique Constitutionnelle; Service de Génétique; Oscar Lambret Cancer Centre, Lille; Human Molecular Oncology Unit; Gustave Roussy; Biopathology integrated Genetic platform; Oncogenetic Laboratory; Lille University Hospital; Endocrine Molecular Oncogenetic Unit; Rouen University Hospital; Molecular Genetics, Department of Genetics; Nantes University Hospital; Plateforme de Génétique moléculaire des cancers; Service de génétique médicale. We are grateful to Frederique Nowak and Etienne Lonchamp (biology, transfer and innovations department, National Cancer Institute, France), Huong Ly Hoang (Institut Curie, Paris, France), Maroua Mimouni (URC-Eco, Ile-de-France, Paris, France), Dominik Heinz, and Marie Warren Collon (Cancer Centre Léon Bérard, Lyon, France).
Funding
This study was supported by a grant from the French National Cancer Institute, dedicated to economic analyses of innovative techniques (reference number 2013-1-NGS-02). This research was funded by the National Cancer Institute in France (INCa) and the Canceropôle Ile de France. The views expressed in this work are those of the authors and not those of the funding bodies.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marino, P., Touzani, R., Perrier, L. et al. Cost of cancer diagnosis using next-generation sequencing targeted gene panels in routine practice: a nationwide French study. Eur J Hum Genet 26, 314–323 (2018). https://doi.org/10.1038/s41431-017-0081-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41431-017-0081-3
This article is cited by
-
EMQN best practice guidelines for analysis and reporting of microsatellite instability in solid tumours
European Journal of Human Genetics (2026)
-
Advancing chronic myeloid leukemia research with next-generation sequencing: potential benefits, limitations, and future clinical integration
Human Genetics (2025)
-
Innovative laboratory techniques shaping cancer diagnosis and treatment in developing countries
Discover Oncology (2025)
-
Transcriptome profiling of pediatric extracranial solid tumors and lymphomas enables rapid low-cost diagnostic classification
Scientific Reports (2024)
-
A novel colorectal cancer test combining microsatellite instability and BRAF/RAS analysis: Clinical validation and impact on Lynch syndrome screening
BJC Reports (2024)