Abstract
Introduction
Photobiomodulation (PBM) with low-level laser therapy (LLLT) is a non-invasive method for accelerating orthodontic tooth movement (OTM). Several systematic reviews (SRs) have assessed the effectiveness of LLLT on OTM acceleration. However, the interpretations and analysis of the findings of these SRs are inconclusive and inconsistent due to the substantial heterogeneity of their results, mainly due to the wide variety of parameters employed in the primary studies. This umbrella review (UR) aims to (i) Evaluate and summarize the findings of SRs evaluating the effect of LLLT on OTM acceleration. (ii) Suggest an evidence-based protocol with the most predictable application LLLT parameters for OTM acceleration.
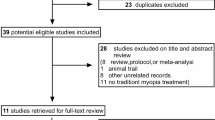
Methods
Medline (PubMed), Web of Science, and Scopus were searched from inception to December 2023. AMSTAR-2 and ROBIS were used to evaluate methodological quality and risk of bias respectively.
Results
Six SRs met the inclusion criteria. All the SRs suggest that PBM with LLLT tends to be effective in accelerating OTM. However, the high heterogeneity of SRs hinders a precise evaluation of the LLLT’s effect on OTM acceleration. The parameters most associated with OTM acceleration are LLLT frequency: At least twice a month, irradiation points: 4-10 points, irradiation time per point: 3–50 s, output power: 20–150 mW, energy density: 5.3 J/cm2 and wavelength range:780–810 nm. The risk of bias assessment identified that 50% of the included SR had a risk of bias ranging from uncertain to high. Similarly, three SRs obtained a “Critically low-quality” assessment.
Conclusions
Although, all the SRs included in this UR suggest that LLLT may accelerate OTM in comparison to control groups. The primary goal of future studies examining the influence of LLLT on the acceleration of OTM should be to create standardised protocols for the use of LLLT, allowing the development of more predictable therapies. The research protocol was registered on the Prospero CRD42024497420.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this article.
References
Grajales M, Ríos-Osorio N, Jimenez-Peña O, Mendez-Sanchez J, Sanchez-Fajardo K, García-Perdomo HA. Effectiveness of photobiomodulation with low-level lasers on the acceleration of orthodontic tooth movement: a systematic review and meta-analysis of split-mouth randomised clinical trials. Lasers Med Sci. 2023;38:200.
Li Y, Jacox LA, Little SH, Ko CC. Orthodontic tooth movement: the biology and clinical implications. Kaohsiung J Med Sci. 2018;34:207–14.
Tsichlaki A, Chin SY, Pandis N, Fleming PS. How long does treatment with fixed orthodontic appliances last? A systematic review. Am J Orthod Dentofacial Orthop. 2016;149:308–18.
Tam SY, Tam VCW, Ramkumar S, Khaw ML, Law HKW, Lee SWY. Review on the cellular mechanisms of low-level laser therapy use in oncology. Front Oncol. 2020;10:1255.
Rola P, Włodarczak S, Lesiak M, Doroszko A, Włodarczak A. Changes in cell biology under the influence of low-level laser therapy. Photonics. 2022;9:502.
Chintavalakorn R, Saengfai NN, Sipiyaruk K. The protocol of low-level laser therapy in orthodontic practice: a scoping review of literature. J Int Soc Prev Community Dent. 2022;12:267–86.
Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011;29:191–6.
Jedliński M, Romeo U, Del Vecchio A, Palaia G, Galluccio G. Comparison of the effects of photobiomodulation with different lasers on orthodontic movement and reduction of the treatment time with fixed appliances in novel scientific reports: a systematic review with meta-analysis. Photobiomodul Photomed Laser Surg. 2020;38:455–65.
Domínguez Camacho A, Montoya Guzmán D, Velásquez Cujar SA. Effective wavelength range in photobiomodulation for tooth movement acceleration in orthodontics: a systematic review. Photobiomodul Photomed Laser Surg. 2020;38:581–90.
AlShahrani I, Togoo RA, Hosmani J, Alhaizaey A. Photobiomodulation in acceleration of orthodontic tooth movement: a systematic review and meta-analysis. Complement Ther Med. 2019;47:102220.
Ge MK, He WL, Chen J, Wen C, Yin X, Hu ZA, et al. Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci. 2015;30:1609–18.
Yavagal CM, Matondkar SP, Yavagal PC. Efficacy of laser photobiomodulation in accelerating orthodontic tooth movement in children: a systematic review with meta-analysis. Int J Clin Pediatr Dent. 2021;14:S94–S100.
Long H, Zhou Y, Xue J, Liao L, Ye N, Jian F, et al. The effectiveness of low-level laser therapy in accelerating orthodontic tooth movement: a meta-analysis. Lasers Med Sci. 2015;30:1161–70.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–40.
Thomson K, Bambra C, McNamara C, Huijts T, Todd A. The effects of public health policies on population health and health inequalities in European welfare states: protocol for an umbrella review. Syst Rev. 2016;5:57.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.5 (updated August 2024). Cochrane. 2024. Available from www.training.cochrane.org/handbook.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Zheng DH, Du YQ, Zhang QQ, Hou FC, Niu SQ, Zang YJ, et al. Effect of low-level laser therapy on orthodontic dental alignment: a systematic review and meta-analysis. Lasers Med Sci. 2023;38:184.
de Almeida VL, de Andrade Gois VL, Andrade RN, Cesar CP, de Albuquerque-Junior RL, de Mello Rode S, et al. Efficiency of low-level laser therapy within induced dental movement: a systematic review and meta-analysis. J Photochem Photobiol B. 2016;158:258–66.
Huang T, Wang Z, Li J. Efficiency of photobiomodulation on accelerating the tooth movement in the alignment phase of orthodontic treatment-A systematic review and meta-analysis. Heliyon. 2023;9:e13220.
Olmedo-Hernández OL, Mota-Rodríguez AN, Torres-Rosas R, Argueta-Figueroa L. Effect of the photobiomodulation for acceleration of the orthodontic tooth movement: a systematic review and meta-analysis. Lasers Med Sci. 2022;37:2323–41.
Baghizadeh Fini M, Olyaee P, Homayouni A. The effect of low-level laser therapy on the acceleration of orthodontic tooth movement. J Lasers Med Sci. 2020;11:204–11.
Sousa MV, Pinzan A, Consolaro A, Henriques JF, de Freitas MR. Systematic literature review: influence of low-level laser on orthodontic movement and pain control in humans. Photomed Laser Surg. 2014;32:592–9.
Farsaii A, Al-Jewair T. Insufficient evidence supports the use of low-level laser therapy to accelerate tooth movement, prevent orthodontic relapse, and modulate acute pain during orthodontic treatment. J Evid Based Dent Pract. 2017;17:262–4.
Reis CLB, de Souza Furtado TC, Mendes WD, Matsumoto MAN, Alves SYF, Stuani MBS, et al. Photobiomodulation impacts the levels of inflammatory mediators during orthodontic tooth movement? A systematic review with meta-analysis. Lasers Med Sci. 2022;37:771–87.
Cronshaw M, Parker S, Anagnostaki E, Lynch E. Systematic review of orthodontic treatment management with photobiomodulation therapy. Photobiomodul Photomed Laser Surg. 2019;37:862–8.
Jnaneshwar PR, Venkatesan K, Prince T, Pethuraj V, Rajaram K, Bhat S. Assessment of the effect of frequency of low-level laser therapy exposure at different intervals on orthodontic tooth movement - A systematic review and meta-analysis. J Orthod Sci. 2023;12:14.
Imani MM, Golshah A, Safari-Faramani R, Sadeghi M. Effect of low-level laser therapy on orthodontic movement of human canine: a systematic review and meta-analysis of randomized clinical trials. Acta Inform Med. 2018;26:139–43.
Figueiredo Deana N, Alves N, Sandoval P. Effectiveness of photobiomodulation therapy in accelerating orthodontic tooth movement: a meta-analysis of randomized clinical trials. J Oral Res. 2019;8:416–32.
Bakdach WMM, Hadad R. Effectiveness of low-level laser therapy in accelerating the orthodontic tooth movement: A systematic review and meta-analysis. Dent Med Probl. 2020;57:73–94.
Papatheodorou SI, Evangelou E. Umbrella reviews: what they are and why we need them. Methods Mol Biol. 2022;2345:135–46.
Schlesinger S, Schwingshackl L, Neuenschwander M, Barbaresko J. A critical reflection on the grading of the certainty of evidence in umbrella reviews. Eur J Epidemiol. 2019;34:889–90.
Sandoval P, Bizcar B, Navarro P, Knösel M. Efficacy of diode laser therapy in acceleration of orthodontic space closure: a split-mouth randomized clinical trial. Int J Dent Oral Health. 2017;3:1–6.
Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141:289–97.
Üretürk SE, Saraç M, Fıratlı S, Can ŞB, Güven Y, Fıratlı E. The effect of low-level laser therapy on tooth movement during canine distalization. Lasers Med Sci. 2017;32:757–64.
Impellizzeri A, Horodynski M, Fusco R, Palaia G, Polimeni A, Romeo U, et al. Photobiomodulation therapy on orthodontic movement: analysis of preliminary studies with a new protocol. Int J Environ Res Public Health. 2020;17:3547.
Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A. Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am J Orthod Dentofacial Orthop. 2017;152:622–30.
Cruz DR, Kohara EK, Ribeiro MS, Wetter NU. Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med. 2004;35:117–20.
Yamaguchi M, Hayashi M, Fujita S, Yoshida T, Utsunomiya T, Yamamoto H, et al. Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta (3) integrin in rats. Eur J Orthod. 2010;32:131–9.
Yassaei S, Aghili H, Afshari JT, Bagherpour A, Eslami F. Effects of diode laser (980 nm) on orthodontic tooth movement and interleukin 6 levels in gingival crevicular fluid in female subjects. Lasers Med Sci. 2016;31:1751–9.
Domínguez A, Velásquez SA. Acceleration of dental movement by photobiomodulation: how does it happen? Photobiomodul Photomed Laser Surg. 2021;39:379–80.
Varella AM, Revankar AV, Patil AK. Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2018;154:535–44.
Zheng J, Yang K. Clinical research: low-level laser therapy in accelerating orthodontic tooth movement. BMC Oral Health. 2021;21:324.
Saygun I, Karacay S, Serdar M, Ural AU, Sencimen M, Kurtis B. Effects of laser irradiation on the release of basic fibroblast growth factor (bFGF), insulin like growth factor-1 (IGF-1), and receptor of IGF-1 (IGFBP3) from gingival fibroblasts. Lasers Med Sci. 2008;23:211–5.
Jose JA, Somaiah S, Muddaiah S, Shetty B, Reddy G, Roopa S. A comparative evaluation of interleukin 1 beta and prostaglandin E2 with and without low-level laser therapy during En masse retraction. Contemp Clin Dent. 2018;9:267–75.
Hadis MA, Zainal SA, Holder MJ, Carroll JD, Cooper PR, Milward MR, et al. The dark art of light measurement: accurate radiometry for low-level light therapy. Lasers Med Sci. 2016;31:789–809.
Ash C, Dubec M, Donne K, Bashford T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med Sci. 2017;32:1909–18.
Karu TI. Multiple roles of cytochrome c oxidase in mammalian cells under the action of red and IR-A radiation. IUBMB Life. 2010;62:607–10.
Huang Y-Y, Chen AC-H, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose Response. 2009;7:358–83.
Ekizer A, Turker G, Uysal T, Guray E, Tasdemir Z. Light emitting diode mediated photobiomodulation therapy improves orthodontic tooth movement and miniscrew stability: A randomized controlled clinical trial. Lasers Surg Med. 2016;48:936–43.
Pérignon B, Bandiaky ON, Fromont-Colson C, Renaudin S, Peré M, Badran Z, et al. Effect of 970 nm low-level laser therapy on orthodontic tooth movement during Class II intermaxillary elastics treatment: a RCT. Sci Rep. 2021;11:23226.
Vayshenker I, Li X, Livigni DJ, Scott TR, Cromer CL. NIST measurement services: optical fiber power meter calibrations at NIST. NIST Spec Publ. 2000:250–54.
Caviedes-Bucheli J, Muñoz-Alvear HD, Lopez-Moncayo LF, Narvaez-Hidalgo A, Zambrano-Guerrero L, Gaviño-Orduña JF, et al. Use of scaffolds and regenerative materials for the treatment of immature necrotic permanent teeth with periapical lesion: umbrella review. Int Endod J. 2022;55:967–88.
Gates A, Gates M, Duarte G, Cary M, Becker M, Prediger B, et al. Evaluation of the reliability, usability, and applicability of AMSTAR, AMSTAR 2, and ROBIS: protocol for a descriptive analytic study. Syst Rev. 2018;7:85.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Conceptualization: NR, OMJ, MG. Methodology: NR, OMJ. Search strategy and article selection: NR, OMJ, MG, LAV. Data extraction: NR, OMJ, MG, LAV. Qualitative synthesis: NR, MG, OMJ, LAV. Risk of bias assessment: OMJ, NR, MG, LAV. Formal analysis: OMJ, MG, NR, GG. Writing: NR, OMJ, MG. Supervision of the manuscript: NR, GG.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiménez-Peña, O.M., Ríos-Osorio, N., Velandia-Palacio, L.A. et al. Effectiveness of photobiomodulation with low-level lasers on the acceleration of orthodontic tooth movement: an umbrella review. Evid Based Dent 26, 113–114 (2025). https://doi.org/10.1038/s41432-024-01090-8
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41432-024-01090-8