Abstract
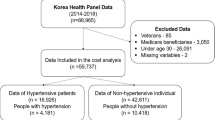
This study was a cost-effectiveness analysis of intensive blood pressure (BP) control among hypertensive patients in Korea. We constructed a Markov model comparing intensive versus standard BP control treatment and calculated the incremental cost-effectiveness ratio. The study population consisted of hypertensive patients over 50 years old with systolic blood pressures (SBPs) exceeding 140 mmHg and at high risk of cardiovascular disease. Treatment alternatives included lowering the SBP below 120 mmHg (intensive) and 140 mmHg (standard) for target BP. We assumed five scenarios with different medication adherence. The effectiveness variable was quality-adjusted life years (QALYs), and costs included medical costs related to hypertension (HT), complications, and nonmedical costs. In addition, we performed a sensitivity analysis to confirm the robustness of the results of this study. Scenario 5, with 100% medication adherence, showed the lowest incremental cost-effectiveness ratio (ICER) of $1,373 USD, followed by scenario 1 (first 15 years: 62.5%, 16–30 years: 65.2%, after 30 years: 59.5%), scenario 2 (first five years: 62.5% decrease by 5% every five years), and scenario 3 (first 10 years: 62.5% decrease by 10% every 10 years). The ICERs in all scenarios were lower than the willingness to pay (WTP) threshold of $9,492–$32,907 USD in Korea. Tornado analysis showed that the ICERs were changed greatly according to stroke incidence. Intensive treatment of HT prevents cardiovascular disease (CVD); therefore, intensive treatment is more cost-effective than standard treatment despite the consumption of more health resources. ICERs are considerably changed according to medication adherence, confirming the importance of patient adherence to treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Korean Society H, Hypertension Epidemiology Research Working G, Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018;24:13.
Lee EM. Optimal strategy of hypertension screening in a nationwide health examination: early and periodic blood pressure measurement. Korean Circ J. 2021;51:623–5.
Lee HY, Lee SW, Kim HC, Ihm SH, Park SH, Kim TH. Cost-effectiveness analysis of hypertension screening in the Korea National Health Screening Program. Korean Circ J. 2021;51:610–22.
Kim HC, Ihm SH, Kim GH, Kim JH, Kim KI, Lee HY, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens 2019;25:16.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:e13–e115.
SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N. Engl J Medicine\ 2015;373:2103–16.
Kim HC, Jeon YW, Heo ST. Global Impact of the 2017 American College of Cardiology/American Heart Association Hypertension Guidelines. Circulation 2018;138:2312–4.
Richman IB, Fairley M, Jorgensen ME, Schuler A, Owens DK, Goldhaber-Fiebert JD. Cost-effectiveness of Intensive Blood Pressure Management. JAMA Cardiol 2016;1:872–9.
Moise N, Huang C, Rodgers A, Kohli-Lynch CN, Tzong KY, Coxson PG, et al. Comparative cost-effectiveness of conservative or intensive blood pressure treatment guidelines in adults aged 35–74 years: the cardiovascular disease policy model. Hypertension 2016;68:88–96.
Xie X, He T, Kang J, Siscovick DS, Li Y, Pagan JA. Cost-effectiveness analysis of intensive hypertension control in China. Preventive Med. 2018;111:110–4.
Li C, Chen K, Cornelius V, Tomeny E, Wang Y, Yang X, et al. Applicability and cost-effectiveness of the Systolic Blood Pressure Intervention Trial (SPRINT) in the Chinese population: A cost-effectiveness modeling study. PLoS Med. 2021;18:e1003515.
Group SR, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Choi KH, Yu YM, Ah YM, Chang MJ, Lee JY. Persistence with antihypertensives in uncomplicated treatment-naive very elderly patients: a nationwide population-based study. BMC cardiovascular Disord. 2017;17:232.
Health Insurance Review and Assessment. Guidelines for Economic Evaluation of Medicine.). Health Insurance Review and Assessment,: Seoul, 2011.
Lee Y-h, Han K, Ko S-H, Ko KS, Lee K-U. Data analytic process of a nationwide population-based study using national health information database established by national health insurance service. Diabetes Metab J. 2016;40:79–82.
Bress AP, Bellows BK, King JB, Hess R, Beddhu S, Zhang Z, et al. Cost-effectiveness of intensive versus standard blood-pressure control. N Engl J Med. 2017;377:745–55.
Hay JW, Smeeding J, Carroll NV, Drummond M, Garrison LP,Mansley EC, et al. Good research practices for measuring drug costs in cost effectiveness analyses: issues and recommendations: the ISPOR Drug Cost Task Force report–Part I. Value Health. 2010;13:3–7.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford university press 2015.
Lajoie J. Understanding the Measurement of Global Burden of Disease. National Collaborating Centre for Infect Dis. 2014. Project No. 147.
Sullivan PW, Ghushchyan VJMDM. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006;26:410–20.
Kim Younhee, Shin Sangjin, Park Sunyoung, Song Hyunjin, Park Jooyeon, Bae Eunyoung, et al. A study of identifying factors affecting cost-effectiveness threshold calculation in Korea. Korean J Health Econ Policy. 2010;16:79–100.
Park S. Ideal target blood pressure in hypertension. Korean circulation J. 2019;49:1002–9.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67.
Ko MJ, Jo AJ, Park CM, Kim HJ, Kim YJ, Park DW. Level of blood pressure control and cardiovascular events: SPRINT criteria versus the 2014 hypertension recommendations. J Am Coll Cardiol. 2016;67:2821–31.
Lonn EM, Bosch J, Lopez-Jaramillo P, Zhu J, Liu L, Pais P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–20.
Group SR, Lewis CE, Fine LJ, Beddhu S, Cheung AK, Cushman WC, et al. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med 2021;384:1921–30.
Chi G, Jamil A, Jamil U, Balouch MA, Marszalek J, Kahe F, et al. Effect of intensive versus standard blood pressure control on major adverse cardiac events and serious adverse events: A bivariate analysis of randomized controlled trials. Clin Exp Hypertens. 2018(e-pub ahead of print 2018/04/11; https://doi.org/10.1080/10641963.2018.1462373):1–8.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering treatment in hypertension: 8. Outcome reductions vs. discontinuations because of adverse drug events - meta-analyses of randomized trials. J Hypertens. 2016;34:1451–63.
Hasan SS, Kow CS, Dawoud D, Mohamed O, Baines D, Babar ZU. Pharmaceutical policy reforms to regulate drug prices in the Asia Pacific region: the case of Australia, China, India, Malaysia, New Zealand, and South Korea. Value Health Reg Issues. 2019;18:18–23.
Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens 2019;25:20.
Derington CG, King JB, Bryant KB, McGee BT, Moran AE, Weintraub WS, et al. Cost-effectiveness and challenges of implementing intensive blood pressure goals and team-based care. Curr Hypertens Rep. 2019;21:91.
Carter BL, Coffey CS, Ardery G, Uribe L, Ecklund D, James P, et al. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2015;8:235–43.
Funding
This research was supported by grant KSH-R-2018-02 from The Korean Society of Hypertension.
Author information
Authors and Affiliations
Contributions
KTH and LHY conceived and designed the study and had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. LYS and LHY drafted the paper. All authors contributed to data collection and interpretation. All authors critically revised the manuscript for relevant intellectual content and gave final approval for the version to be published. All authors agree to be accountable for all aspects of ensuring any questions related to the accuracy or integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, Y.S., Lee, HY. & Kim, T.H. Cost-effectiveness analysis of intensive blood pressure control in Korea. Hypertens Res 45, 507–515 (2022). https://doi.org/10.1038/s41440-021-00774-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-021-00774-3
Keywords
This article is cited by
-
The Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025)
Hypertension Research (2026)
-
Cost-effectiveness of strengthening blood pressure classification in South Korea: comparing the 2017 ACC/AHA and KSH guidelines
Clinical Hypertension (2024)
-
Examining the potential impacts of intensive blood pressure treatment on the socioeconomic inequity in hypertension prevalence in China: a nationally representative cross-sectional study
Hypertension Research (2023)