Abstract
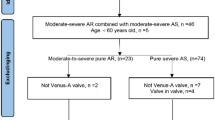
The effect of arterial stiffening on elevated pulsatile left ventricular afterload patients with aortic stenosis (AS) is pronounced beyond systemic hypertension. Circulatory afterload pulsatile efficiency (CAPE) is a marker of vascular function, defined as the ratio of steady state energy consumption (SEC) to maintain systemic circulation and pulsatile energy consumption (PEC). Twenty patients aged 80 ± 7 years were assessed at baseline and a median of 60 days post transcatheter aortic valve replacement (TAVR), with pulsatile vascular load calculated using simultaneous radial applanation tonometry derived aortic pressure and cardiac magnetic resonance phase-contrast imaging derived ascending aortic flow. Eight out of 20 patients had a reduction in PEC post TAVR, and the reduction of PEC correlated strongly with the number of days post TAVR (R = 0.62, P < 0.01). Patients assessed within the 100 days of TAVR had a rise in their PEC when compared to baseline (0.19 ± 0.09 vs 0.14 ± 0.08 W, P = 0.04). Baseline PEC correlated moderately with baseline SEC (R = 0.49, P = 0.03), and a high baseline PEC was predictive of post TAVR PEC reduction (R = 0.54, P =0.01). Overall, no significant differences were found between baseline and post TAVR for systolic aortic pressure (131 ± 20 vs 131 ± 20 mmHg), systemic vascular resistance (1894 ± 493 vs 2015 ± 519 dynes.s/cm5), aortic valve ejection time (337 ± 22 vs 324 ± 34 ms) or aortic characteristic impedance (120 ± 48 vs 107 ± 41 dynes.s/cm5). Improved flow profiles after TAVR likely unmask the true vascular properties by altering ventriculo-valvulo-arterial coupling, leading to downstream vascular remodelling secondary to flow conditioning, and results in eventual improvement of pulsatile afterload as reflected by our proposed index of CAPE.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lindman BR, Dweck MR, Lancellotti P, Généreux P, Piérard LA, O’Gara PT, et al. Management of asymptomatic severe aortic stenosis: evolving concepts in timing of valve replacement. JACC Cardiovasc Imaging. 2020;13:481–93.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e72–227.
Otto CM, Kuusisto J, Reichenbach DD, Gown AM, O’Brien KD. Characterization of the early lesion of “degenerative” valvular aortic stenosis. Histological immunohistochem Stud Circ. 1994;90:844–53.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27.
Lindman BR, Otto CM, Douglas PS, Hahn RT, Elmariah S, Weissman NJ, et al. Blood pressure and arterial load after transcatheter aortic valve replacement for aortic stenosis. Circ Cardiovasc Imaging. 2017;10:1–12.
Hungerford SL, Adji AI, Hayward CS, Muller DWM. Ageing, hypertension and aortic valve stenosis: a conscious uncoupling. Heart Lung Circ. 2021;30:1627–36.
Hachicha Z, Dumesnil JG, Pibarot P. Usefulness of the valvuloarterial impedance to predict adverse outcome in asymptomatic aortic stenosis. J Am Coll Cardiol. 2009;54:1003–11.
Soulat G, Kachenoura N, Bollache E, Perdrix L, Diebold B, Zhygalina V, et al. New estimate of valvuloarterial impedance in aortic valve stenosis: a cardiac magnetic resonance study. J Magn Reson Imaging. 2017;45:795–803.
Briand M, Dumesnil JG, Kadem L, Tongue AG, Rieu R, Garcia D, et al. Reduced systemic arterial compliance impacts significantly on left ventricular afterload and function in aortic stenosis: Implications for diagnosis and treatment. J Am Coll Cardiol. 2005;46:291–8.
Yotti R, Bermejo J, Gutiérrez-Ibañes E, Pérez Del Villar C, Mombiela T, Elízaga J, et al. Systemic vascular load in calcific degenerative aortic valve stenosis: Insight from percutaneous valve replacement. J Am Coll Cardiol. 2015;65:423–33.
O’rourke MF. Steady and pulsatile energy losses in the systemic circulation under normal conditions and in simulated arterial disease. Cardiovasc Res. 1967;1:313–26.
Hungerford SL, Adji AI, Bart NK, Lin L, Namasivayam MJ, Schnegg B, et al. A novel method to assess valvulo-arterial load in patients with aortic valve stenosis. J Hypertens. 2021;39:437–46.
Beck DT, Martin JS, Nichols WW, Gurovich AN, Braith RW. Validity of a novel wristband tonometer for measuring central hemodynamics and augmentation index. Am J Hypertens. 2014;27:926–31.
Namasivayam M, Adji A, Lin L, Hayward CS, Feneley MP, O’Rourke MF, et al. Non-invasive quantification of ventricular contractility, arterial elastic function and ventriculo-arterial coupling from a single diagnostic encounter using simultaneous arterial tonometry and magnetic resonance imaging. Cardiovasc Eng Technol. 2020;11:283–94.
Adji A, Kachenoura N, Bollache E, Avolio AP, O’Rourke MF, Mousseaux E. Magnetic resonance and applanation tonometry for noninvasive determination of left ventricular load and ventricular vascular coupling in the time and frequency domain. J Hypertens. 2016;34:1099–108.
Bonow RO, Brown AS, Gillam LD, Kapadia SR, Kavinsky CJ, Lindman BR, et al. ACC/AATS/AHA/ASE/EACTS/HVS/SCA/SCAI/SCCT/SCMR/STS 2017 appropriate use criteria for the treatment of patients with severe aortic stenosis: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Intervent. J Am Soc Echocardiogr. 2018;31:117–47.
Nichols WW, Conti CR, Walker WE, Milnor WR. Input impedance of the systemic circulation in man. Circ Res. 1977;40:451–8.
Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation. 2007;115:2856–64.
Katsanos S, Yiu KH, Clavel MA, Rodés-Cabau J, Leong D, Van Der Kley F, et al. Impact of valvuloarterial impedance on 2-year outcome of patients undergoing transcatheter aortic valve implantation. J Am Soc Echocardiogr. 2013;26:691–8.
Saeed S, Saeed N, Grigoryan K, Chowienczyk P, Chambers JB, Rajani R. Determinants and clinical significance of aortic stiffness in patients with moderate or severe aortic stenosis. Int J Cardiol. 2020;315:99–104.
Nemes A, Galema TW, Geleijnse ML, Soliman OII, Yap SC, Anwar AM, et al. Aortic valve replacement for aortic stenosis is associated with improved aortic distensibility at long-term follow-up. Am Heart J. 2007;153:147–51.
Musa TAL, Uddin A, Fairbairn TA, Dobson LE, Sourbron SP, Steadman CD, et al. Assessment of aortic stiffness by cardiovascular magnetic resonance following the treatment of severe aortic stenosis by TAVI and surgical AVR. J Cardiovasc Magn Reson. 2016;18:37.
Barbetseas J, Alexopoulos N, Brili S, Aggeli C, Marinakis N, Vlachopoulos C, et al. Changes in aortic root function after valve replacement in patients with aortic stenosis. Int J Cardiol. 2006;110:74–9.
Chirinos JA, Akers SR, Schelbert E, Snyder BS, Witschey WR, Jacob RM, et al. Arterial properties as determinants of left ventricular mass and fibrosis in severe aortic stenosis: findings from ACRIN PA 4008. J Am Heart Assoc. 2019;8:e03742.
Plunde O, Bäck M. Arterial stiffness in aortic stenosis and the impact of aortic valve replacement. Vasc Health Risk Manag. 2022;18:117–22.
Vavuranakis M, Vrachatis DA, Boudoulas H, Papaioannou TG, Moldovan C, Kariori MG, et al. Effect of transcatheter aortic valve implantation on the ascending aorta’s elasticity. Clin Res Cardiol. 2012;101:895–9. 10111. 2012
Terentes-Printzios D, Gardikioti V, Aznaouridis K, Latsios G, Drakopoulou M, Siasos G, et al. The impact of transcatheter aortic valve implantation on arterial stiffness and wave reflections. Int J Cardiol. 2021;323:213–9.
Müller C, Goliasch G, Schachinger S, Kastl S, Neunteufl T, Delle-Karth G, et al. Transcatheter aortic valve replacement (TAVR) leads to an increase in the subendocardial viability ratio assessed by pulse wave analysis. PLoS ONE. 2018;13:e0207537.
Vizzardi E, Sciatti E, Bonadei I, D’Aloia A, Gelsomino S, Lorusso R, et al. Effects of transcatheter aortic valve implantation on ascending aorta wall elastic properties: Tissue Doppler imaging and strain Doppler echocardiography study. Int J Cardiol Heart Vessel. 2014;4:198.
Goudzwaard JA, Disegna E, de Ronde-Tillmans MJAG, Lenzen MJ, de Jaegere PPT, Mattace-Raso FUS. Short-term changes of blood pressure and aortic stiffness in older patients after transcatheter aortic valve implantation. Clin Inter Aging. 2019;14:1379.
Treibel TA, Kozor R, Schofield R, Benedetti G, Fontana M, Bhuva AN, et al. Reverse myocardial remodeling following valve replacement in patients with aortic stenosis. J Am Coll Cardiol. 2018;71:860–71.
Gamaza-Chulián S, Díaz-Retamino E, Camacho-Freire S, Ruiz-Fernández D, Gutiérrez-Barrios A, Oneto-Otero J. Acceleration time and ratio of acceleration time to ejection time in aortic stenosis: new echocardiographic diagnostic parameters. J Am Soc Echocardiogr. 2017;30:947–55.
Bache RJ, Wang Y, Greenfield JC. Left ventricular ejection time in valvular aortic stenosis. Circulation. 1973;47:527–33.
Pagoulatou S, Stergiopulos N, Bikia V, Rovas G, Licker MJ, Müller H, et al. Acute effects of transcatheter aortic valve replacement on the ventricular-aortic interaction. Am J Physiol Hear Circ Physiol. 2020;319:1451–8.
Plunde O, Franco-Cereceda A, Bäck M. Cardiovascular risk factors and hemodynamic measures as determinants of increased arterial stiffness following surgical aortic valve replacement. Front Cardiovasc Med. 2021;8:754371.
Sörensen J, Harms HJ, Aalen JM, Baron T, Smiseth OA, Flachskampf FA. Myocardial efficiency: a fundamental physiological concept on the verge of clinical impact. JACC Cardiovasc Imaging. 2020;13:1564–76.
Hansson NHS, Sörensen J, Harms HJ, Kim WY, Nielsen R, Tolbod LP, et al. Myocardial oxygen consumption and efficiency in aortic valve stenosis patients with and without heart failure. J Am Heart Assoc. 2017;6:e004810.
Güçlü A, Knaapen P, Harms HJ, Vonk ABA, Stooker W, Groepenhoff H, et al. Myocardial efficiency is an important determinant of functional improvement after aortic valve replacement in aortic valve stenosis patients: a combined PET and CMR study. Eur Hear J Cardiovasc Imaging. 2015;16:882–9.
Lee C-B, Goubergrits L, Fernandes JF, Nordmeyer S, Knosalla C, Berger F, et al. Surrogates for myocardial power and power efficiency in patients with aortic valve disease. Sci Rep. 2019;9:1–10.
Nordmeyer S, Lee CB, Goubergrits L, Knosalla C, Berger F, Falk V, et al. Circulatory efficiency in patients with severe aortic valve stenosis before and after aortic valve replacement. J Cardiovasc Magn Reson. 2021;23:1–14.
Qureshi MU, Colebank MJ, Schreier DA, Tabima DM, Haider MA, Chesler NC, et al. Characteristic impedance: Frequency or time domain approach? Physiol Meas. 2018;39:014004.
Acknowledgements
We would like to thank Dr. Mark Butlin from Macquarie University for his contribution to maintain our working equipment, and the staff at the Advanced Cardiac Imaging Centre at St Vincent’s Hospital, Sydney for their support of the study.
Funding
NS is supported by a Cardiac Society of Australia and New Zealand Research Scholarship and an Australian Government Department of Education Research and Training Programme grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DWMM has been an advisory board member for Medtronic and Boston Scientific; has been a consultant to Abbott Vascular, Medtronic; has received research grant support from Abbott Vascular and Medtronic; and is a proctor for Medtronic and Abbott Vascular.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, N., Adji, A.I., Hungerford, S.L. et al. Pulsatile energy consumption as a surrogate marker for vascular afterload improves with time post transcatheter aortic valve replacement in patients with aortic stenosis. Hypertens Res 46, 730–741 (2023). https://doi.org/10.1038/s41440-022-01127-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-022-01127-4