Abstract
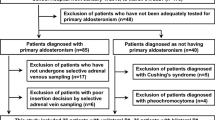
Mineralocorticoid receptor antagonists (MRAs) for bilateral primary aldosteronism (PA) are the mainstay option recommended by guidelines, but poor compliance occurs due to numerous side effects. We aimed to examine whether catheter-based adrenal ablation could be an alternative treatment for bilateral PA.644 PA patients were included from a total of 6054 hypertensive patients. Adrenal CT scan and adrenal venous sampling (AVS) were both performed for PA subtype classification. Clinical and biochemical outcomes were assessed at 6 months after treatment according to the Primary Aldosteronism Surgical Outcome (PASO) criteria.93 patients with PA were recruited to be treated by adrenal ablation, including 25 bilateral PA and 68 unilateral PA according to AVS results. Office SBP and DBP significantly decreased from baseline levels, serum potassium levels increased and ARR significantly decreased (p < 0.01) in both the bilateral and unilateral groups. In the bilateral group, complete, partial and absent clinical success was achieved in 6 (24.0%), 11 (44.0%) and 8(32.0%) patients, respectively. In the unilateral group, complete, partial and absent clinical success was achieved in 12 (17.6%), 37 (54.4%), and 19 (27.9%) patients, respectively. The numbers of patients achieving complete, partial, and absent biochemical success were 15 (60.0%), 6 (24.0%), and 4 (16.0%), respectively, in the bilateral group versus 37 (54.4%), 9 (13.2%), and 22 (32.3%), respectively, in the unilateral group. In conclusion, we provide evidence for the beneficial outcomes of unilateral adrenal ablation for patients with bilateral PA. Our findings provide insight into an alternative option for patients with bilateral excess aldosterone.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Young WF Jr. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med. 2019;285:126–48.
Reincke M, Bancos I, Mulatero P, Scholl UI, Stowasser M, Williams TA. Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol. 2021;9:876–92.
Satoh M, Maruhashi T, Yoshida Y, Shibata H. Systematic review of the clinical outcomes of mineralocorticoid receptor antagonist treatment versus adrenalectomy in patients with primary aldosteronism. Hypertens Res. 2019;42:817–24.
Dekkers T, Prejbisz A, Kool LJS, Groenewoud H, Velema M, Spiering W, et al. Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomized diagnostic trial. Lancet Diabetes Endocrinol. 2016;4:739–46.
Wu VC, Wang SM, Huang KH, Tsai YC, Chan CK, Yang SY, et al. Long-term mortality and cardiovascular events in patients with unilateral primary aldosteronism after targeted treatments. Eur J Endocrinol. 2021;186:195–205.
Hundemer GL, Curhan GC, Nicholas Y, Wang M, Anand V. Incidence of atrial fibrillation and mineralocorticoid receptor activity in patients with medically and surgically treated primary aldosteronism. JAMA Cardiol. 2018;3:768–74.
Shibata H. Adrenal ablation therapy for unilateral primaryaldosteronism: pros and cons. Hypertens Res. 2023;46:787–9.
Deinum J, Riksen NP, Lenders JW. Pharmacological treatment of aldosterone excess. Pharm Ther. 2015;154:120–33.
Williams TA, Gong S, Tsurutani Y, Tezuka Y, Thuzar M, Burrello J, et al. Adrenal surgery for bilateral primary aldosteronism: an international retrospective cohort study. Lancet Diabetes Endocrinol. 2022;10:769–71.
Bouhanick B, Delchier MC, Lagarde S, Boulestreau R, Conil C, GosseP, et al. Radiofrequency ablation for adenoma in patients with primary aldosteronism and hypertension: ADERADHTA, a pilot study. J Hypertens. 2021;39:759–65.
Sacks BA, Sacks AC, Faintuch S. Radiofrequency ablation treatment for aldosterone-producing adenomas. Curr Opin Endocrinol Diabetes Obes. 2017;24:169–73.
Rossi GP, Bisogni V, Bacca AV, Belfiore A, Cesari M, Concistrè A. The 2020 Italian Society of Arterial Hypertension (SIIA) practical guidelines for the management of primary aldosteronism. Int J Cardiol Hypertens. 2020;5:100029.
Sun F, Liu X, Zhang H, Zhou X, Zhao Z, He H, et al. Catheter-based adrenal ablation: an alternative therapy for patients with aldosterone-producing adenoma. Hypertens Res. 2023;46:91–99.
Zhao Z, Liu X, Zhang H, Li Q, He H, Yan Z, et al. Catheter-based adrenal ablation remits primary aldosteronism: a randomized medication-controlled trial. Circulation 2021;144:580–2.
Ohno Y, Naruse M, Beuschlein F, Schreiner F, Parasiliti-Caprino M, Deinum J. et al. Adrenal venous sampling-guided adrenalectomy rates in primary aldosteronism: results of an international cohort (AVSTAT). J Clin Endocrinol Metab. 2021;106:e1400–e1407.
Zhang H, Li Q, Liu X, Zhao Z, He H, Sun F, et al. Adrenal artery ablation for primary aldosteronism without apparent aldosteronoma: an efficacy and safety, proof-of-principle trial. J Clin Hypertens(Greenwich). 2020;22:1618–26.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension (Dallas, Tex : 1979) 2014;63:151–60.
Sun F, Hong Y, Zhang H, Liu X, Zhao Z, He H, et al. Determination of adrenal hypersecretion in primary Aldosteronism without aldosterone-production adenomas. BMC Endocr Disord. 2021;21:114.
Hokotate H, Inoue H, Baba Y, Tsuchimochi S, Nakajo M. Aldosteronomas: experiencewith superselective adrenal arterial embolization in 33 cases. Radiology 2003;227:401–6.
Dong H, Zou Y, He J, Deng Y, Chen Y, Song L, et al. Superselective adrenal arterial embolization for idiopathic hyperaldosteronism: 12-month results from a proof-of-principle trial. Catheter Cardiovasc Inter. 2021;97(Suppl 2):976–81.
Qiu J, Li N, Xiong HL, Yang J, Li YD, Hu CK, et al. Superselective adrenal arterial embolization for primary aldosteronism without lateralized aldosterone secretion: an efficacy and safety, proof-of-principle study. Hypertens Res. 2023;46:1297–310.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. [2018 ESC/ESH Guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH)]. J Hypertens 2018;36:1953–2041.
European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003;21:1011–53.
Tezuka Y, Turcu AF. Real-world effectiveness of mineralocorticoid receptor antagonists in primary aldosteronism. Front Endocrinol (Lausanne). 2021;12:625457.
Chen SY, Chen JY, Huang WC, Puar THK. Cardiovascular outcomes and all-cause mortality in primary aldosteronism after adrenalectomy or mineralocorticoid receptor antagonist treatment: a meta-analysis. Eur J Endocrinol. 2022;187:S47–S58.
Kim KJ, Hong N, Yu MH, Lee H, Lee S, Lim JS, et al. Time-dependent risk of atrial fibrillation in patients with primary aldosteronism after medical or surgical treatment initiation. Hypertension (Dallas, Tex : 1979) 2021;77:1964–73.
Buffolo F, Tetti M, Mulatero P. Aldosterone as a mediator of cardiovascular damage. Hypertension 2022;79:1899–911.
Brown JM, Wijkman MO. Cardiac structure and function across the spectrum of aldosteronism: the atherosclerosis risk in communities study. Hypertension 2022;79:1984–93.
Hundemer GL, Vaidya A. Management of endocrine disease: the role of surgical adrenalectomy in primary aldosteronism. Eur J Endocrinol. 2020;183:R185–R196.
DeLozier OM, Dream SY, Findling JW, Carroll TB, Evans DB, Wang TS. Selective glucocorticoid replacement following unilateral adrenalectomy for hypercortisolism and primary aldosteronism. J Clin Endocrinol Metab. 2022;107:e538–e547.
Heinrich DA, Adolf C, Holler F, Lechner B, Schneider H, Riester A. et al. Adrenal insufficiency after unilateral adrenalectomy in primary aldosteronism: long-term outcome and clinical impact. J Clin Endocrinol Metab. 2019;104:5658–64.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J 2022;69:327–59.
Fassnacht M, Dekkers OM, Else T, Baudin E, Berruti A, de Krijger R, et al. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2018;179:G1–G46.
Espinosa DY, Ana E, Welch TL, Ospina NS, Rodriguez-Gutierrez R, Atwell TD, et al. Image guided thermal ablation of adrenal metastases: hemodynamic and endocrine outcomes. Endocr Pr. 2017;23:132–40.
Pak SJ, Lee YM, Kim PN, Kim BC, Cho JW, Kim WW, et al. Short-term outcome of adrenal radiofrequency ablation of adrenal cysts: a single-center experience. Sci Rep. 2023;13:3267.
Acknowledgements
We acknowledge the Chongqing Endocrine Hypertension Collaborative Team for their contributions to this trial.
Chongqing Endocrine Hypertension Collaborative Team:
Hongyun Miao2, Zhiyong Li3, Ping Wei4, Min Long5, Xiaoli Chen6, Peijin Xia7, Xiaoyun Fan8, Wuquan Deng9, Yangjie He10, Qingbin Liao11, Xingrong Tan12, Liping Zhang13, Yong Luo14, Yong Liao15
Funding
This project has received funding from the National Natural Science Foundation of China (81920108010, 81900380, 81721001, U21A20354) and Third Military Medical University for funding of the Triple A program led by ZMZ.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, F., Zhang, H., He, H. et al. Rationality and implication of catheter-based adrenal ablation for bilateral primary aldosteronism. Hypertens Res 47, 2884–2894 (2024). https://doi.org/10.1038/s41440-024-01815-3
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01815-3
Keywords
This article is cited by
-
High salt intake exacerbates aldosterone-related target organ damage in patients with primary aldosteronism
Hypertension Research (2025)