Abstract
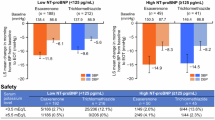
Five first-line classes of antihypertensive drugs are recommended for hypertension treatment. However, it is unclear which class should be chosen for hypertensive patients with pre-heart failure (pre-HF). The study aimed to investigate the association between antihypertensive drug classes and intensity with probability of NT-proBNP (N-terminal pro-B-type natriuretic peptide) improvement and risk of cardiovascular events among pre-HF hypertensive patients. Utilizing the data from SPRINT, we included pre-HF hypertensive patients, identified by NT-proBNP ≥125 pg/mL at baseline. NT-proBNP improvement is defined as a reduction of ≥50% to a level below 125 pg/mL. A total of 3293 patients (mean age: 71.9 years; female: 43.8%) were included. NT-proBNP improvement was observed in 415 patients (12.6%) over 1-year follow up. Thiazide-type diuretics users were associated with a higher likelihood of NT-proBNP improvement (odds ratio [OR], 1.33; 95% confidence interval [CI], 1.05–1.70), a lower risk of HF (hazard ratio [HR], 0.54; 95% CI, 0.37–0.78) and primary composite outcome (HR, 0.72; 95% CI, 0.57–0.89). ACEI/ARB users were only associated with a lower risk of primary composite outcome (HR, 0.80; 95% CI, 0.63–0.99). In contrast, beta-blockers users were associated with a lower likelihood of NT-proBNP improvement (OR, 0.43; 95% CI, 0.34–0.55), while a higher risk of HF (HR, 1.79; 95% CI, 1.21–2.64) and primary composite outcome (HR, 1.48; 95% CI, 1.18–1.87). These associations varied across subgroups of different drug intensities. This post hoc analysis supports the use of thiazide-type diuretics and ACEI/ARB for prevention of cardiovascular events. The use of beta-blockers is associated with an increased risk of HF and primary outcomes, which requires further validation.

Association between antihypertensive drug classes and intensity with NT-proBNP improvement and long-term clinical outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Messerli FH, Rimoldi SF, Bangalore S. The Transition From Hypertension to Heart Failure: Contemporary Update. JACC Heart Fail. 2017;5:543–51. https://doi.org/10.1016/j.jchf.2017.04.012.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021. https://doi.org/10.1016/j.cardfail.2021.01.022.
Bergamasco A, Luyet-Déruaz A, Gollop ND, Moride Y, Qiao Q. Epidemiology of Asymptomatic Pre-heart Failure: a Systematic Review. Curr Heart Fail Rep. 2022;19:146–56. https://doi.org/10.1007/s11897-022-00542-5.
Cai A, Zheng C, Qiu J, Fonarow GC, Lip G, Feng Y, et al. Prevalence of heart failure stages in the general population and implications for heart failure prevention: reports from the China Hypertension Survey 2012-15. Eur J Prev Cardiol. 2023;30:1391–1400. https://doi.org/10.1093/eurjpc/zwad223.
Gidding SS, Lloyd-Jones D, Lima J, Ambale-Venkatesh B, Shah SJ, Shah R, et al. Prevalence of American Heart Association Heart Failure Stages in Black and White Young and Middle-Aged Adults: The CARDIA Study. Circ Heart Fail. 2019;12:e005730 https://doi.org/10.1161/circheartfailure.118.005730.
Morbach C, Gelbrich G, Tiffe T, Eichner FA, Christa M, Mattern R, et al. Prevalence and determinants of the precursor stages of heart failure: results from the population-based STAAB cohort study. Eur J Prev Cardiol. 2021;28:924–34. https://doi.org/10.1177/2047487320922636.
Shah AM, Claggett B, Loehr LR, Chang PP, Matsushita K, Kitzman D, et al. Heart Failure Stages Among Older Adults in the Community: The Atherosclerosis Risk in Communities Study. Circulation. 2017;135:224–40. https://doi.org/10.1161/circulationaha.116.023361.
Xanthakis V, Enserro DM, Larson MG, Wollert KC, Januzzi JL, Levy D, et al. Prevalence, Neurohormonal Correlates, and Prognosis of Heart Failure Stages in the Community. JACC Heart Fail. 2016;4:808–15. https://doi.org/10.1016/j.jchf.2016.05.001.
Pugliese NR, Fabiani I, La Carrubba S, Carerj S, Conte L, Colonna P, et al. Prognostic Value of a Tissue Doppler Index of Systodiastolic Function in Patients with Asymptomatic Heart Failure. J Cardiovasc Echogr. 2018;28:95–100. https://doi.org/10.4103/jcecho.jcecho_59_17.
Miura M, Sakata Y, Nochioka K, Takada T, Tadaki S, Ushigome R, et al. Prevalence, predictors and prognosis of patients with heart failure requiring nursing care. Circ J. 2014;78:2276–83. https://doi.org/10.1253/circj.cj-14-0387
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104. https://doi.org/10.1093/eurheartj/ehy339.
Antonakoudis G, Poulimenos L, Kifnidis K, Zouras C, Antonakoudis H. Blood pressure control and cardiovascular risk reduction. Hippokratia. 2007;11:114–9.
Roberts E, Ludman AJ, Dworzynski K, Al-Mohammad A, Cowie MR, McMurray JJ, et al. The diagnostic accuracy of the natriuretic peptides in heart failure: systematic review and diagnostic meta-analysis in the acute care setting. BMJ. 2015;350:h910 https://doi.org/10.1136/bmj.h910.
Gori M, Lam CSP, D'elia E, Iorio AM, Calabrese A, Canova P, et al. Integrating natriuretic peptides and diastolic dysfunction to predict adverse events in high-risk asymptomatic subjects. Eur J Prev Cardiol. 2021;28:937–45. https://doi.org/10.1177/2047487319899618.
Ewald B, Ewald D, Thakkinstian A, Attia J. Meta-analysis of B type natriuretic peptide and N-terminal pro B natriuretic peptide in the diagnosis of clinical heart failure and population screening for left ventricular systolic dysfunction. Intern Med J. 2008;38:101–13. https://doi.org/10.1111/j.1445-5994.2007.01454.x.
Di Stasio E, Russo A, Mettimano M, Viviani D, Scagliusi A, Bruno A, et al. NT-proBNP: a marker of preclinical cardiac damage in arterial hypertension. Clin Chim Acta. 2011;412:1106–11. https://doi.org/10.1016/j.cca.2011.02.035.
Berry JD, Chen H, Nambi V, Ambrosius WT, Ascher SB, Shlipak MG, et al. Effect of Intensive Blood Pressure Control on Troponin and Natriuretic Peptide Levels: Findings From SPRINT. Circulation. 2023;147:310–23. https://doi.org/10.1161/circulationaha.122.059960.
Jia X, Al Rifai M, Hoogeveen R, Echouffo-Tcheugui JB, Shah AM, Ndumele CE, et al. Association of Long-term Change in N-Terminal Pro-B-Type Natriuretic Peptide With Incident Heart Failure and Death. JAMA Cardiol. 2023;8:222–30. https://doi.org/10.1001/jamacardio.2022.5309.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67. https://doi.org/10.1016/s0140-6736(15)01225-8.
Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, et al. Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis. JAMA. 2003;289:2534–44. https://doi.org/10.1001/jama.289.19.2534.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665 https://doi.org/10.1136/bmj.b1665.
SPRINT Research, G, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–16. https://doi.org/10.1056/NEJMoa1511939.
Ambrosius WT, Sink KM, Foy CG, Berlowitz DR, Cheung AK, Cushman WC, et al. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials. 2014;11:532–46. https://doi.org/10.1177/1740774514537404.
Derington CG, Bress AP, Moran AE, Weintraub WS, Herrick JS, Cushman WC, et al. Antihypertensive Medication Regimens Used in the Systolic Blood Pressure Intervention Trial. Hypertension. 2023;80:590–7. https://doi.org/10.1161/hypertensionaha.122.20373.
Levy PD, Willock RJ, Burla M, Brody A, Mahn J, Marinica A, et al. Total antihypertensive therapeutic intensity score and its relationship to blood pressure reduction. J Am Soc Hypertens. 2016;10:906–16. https://doi.org/10.1016/j.jash.2016.10.005.
Agarwal R, Sinha AD, Cramer AE, Balmes-Fenwick M, Dickinson JH, Ouyang F, et al. Chlorthalidone for Hypertension in Advanced Chronic Kidney Disease. N Engl J Med. 2021;385:2507–19. https://doi.org/10.1056/NEJMoa2110730.
Conway J, Lauwers P. Hemodynamic and hypotensive effects of long-term therapy with chlorothiazide. Circulation. 1960;21:21–7. https://doi.org/10.1161/01.cir.21.1.21.
Mehta RT, Pareek A, Dharmadhikari S. Compelling therapy of LVH: straight (and not-so-straight) inferences from evidence. Clin Hypertens. 2019;25:25 https://doi.org/10.1186/s40885-019-0131-y
Letsas KP, Filippatos GS, Pappas LK, Mihas CC, Markou V, Alexanian IP, et al. Determinants of plasma NT-pro-BNP levels in patients with atrial fibrillation and preserved left ventricular ejection fraction. Clin Res Cardiol. 2009;98:101–6. https://doi.org/10.1007/s00392-008-0728-8.
Ambler SK, Leite MF. Regulation of atrial natriuretic peptide secretion by alpha 1-adrenergic receptors: the role of different second messenger pathways. J Mol Cell Cardiol. 1994;26:391–402. https://doi.org/10.1006/jmcc.1994.1048.
Christensen G, Ilebekk A, Kiil F. Release of atrial natriuretic factor during infusion of isoproterenol and angiotensin II. Am J Physiol. 1989;257:R896–900. https://doi.org/10.1152/ajpregu.1989.257.4.R896.
Christensen G, Aksnes G, Ilebekk A, Kiil F. Release of atrial natriuretic factor during selective cardiac alpha- and beta-adrenergic stimulation, intracoronary Ca2+ infusion, and aortic constriction in pigs. Circ Res. 1991;68:638–44. https://doi.org/10.1161/01.res.68.3.638.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs-overview and meta-analyses. J Hypertens. 2015;33:195–211. https://doi.org/10.1097/hjh.0000000000000447.
Tsujimoto T, Kajio H. Thiazide Use and Decreased Risk of Heart Failure in Nondiabetic Patients Receiving Intensive Blood Pressure Treatment. Hypertension. 2020;76:432–41. https://doi.org/10.1161/hypertensionaha.120.15154.
Sciarretta S, Palano F, Tocci G, Baldini R, Volpe M. Antihypertensive treatment and development of heart failure in hypertension: a Bayesian network meta-analysis of studies in patients with hypertension and high cardiovascular risk. Arch Intern Med. 2011;171:384–94. https://doi.org/10.1001/archinternmed.2010.427.
DeCarolis DD, Gravely A, Olney CM, Ishani A. Impact of Antihypertensive Drug Class on Outcomes in SPRINT. Hypertension. 2022;79:1112–21. https://doi.org/10.1161/hypertensionaha.121.18369.
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145–53. https://doi.org/10.1056/nejm200001203420301.
Fox KM. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet. 2003;362:782–8. https://doi.org/10.1016/s0140-6736(03)14286-9.
Piepoli MF, Adamo M, Barison A, Bestetti RB, Biegus J, Böhm M, et al. Preventing heart failure: a position paper of the Heart Failure Association in collaboration with the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:275–300. https://doi.org/10.1093/eurjpc/zwab147.
Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545–53. https://doi.org/10.1016/s0140-6736(05)67573-3.
Messerli FH, Beevers DG, Franklin SS, Pickering TG. beta-Blockers in hypertension-the emperor has no clothes: an open letter to present and prospective drafters of new guidelines for the treatment of hypertension. Am J Hypertens. 2003;16:870–3. https://doi.org/10.1016/s0895-7061(03)01017-3.
Carlberg B, Samuelsson O, Lindholm LH. Atenolol in hypertension: is it a wise choice? Lancet. 2004;364:1684–9. https://doi.org/10.1016/s0140-6736(04)17355-8.
Acknowledgements
We thank all the investigators, staff, and participants of the SPRINT study for their valuable contributions. This manuscript was prepared using SPRINT Research Materials obtained from the NHLBI.
Funding
This research was funded by National High-Level Hospital Clinical Research Funding (No. 2023-GSP-GG-18).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, L., Yi, J., Wang, W. et al. Impact of first-line antihypertensive drug class and intensity on NT-proBNP improvement and cardiovascular outcomes among hypertensive patients with pre-heart failure: findings from SPRINT trial. Hypertens Res 47, 3447–3457 (2024). https://doi.org/10.1038/s41440-024-01873-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-01873-7