Abstract
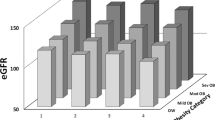
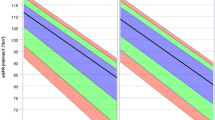
The definition of hyperfiltration, the main pathogenesis in renal impairment in obesity and diabetes mellitus, is uncertain. Glomerular filtration rate (GFR) declines physiologically with aging, and there is inaccuracy in GFR in obesity due to body surface area (BSA) correction. Here, we defined hyperfiltration using GFR without BSA correction, but with inclusion of aging, and investigated hyperfiltration using this definition and absolute GFR > 125 mL/min. The subjects were 180 kidney donor candidates (56.4 ± 11.3 years old, 79 males). GFR was evaluated using inulin clearance. A two-hour 75-g oral glucose tolerance test was also performed. The subjects were divided into four groups with and without a combination of glucose tolerance disorder and BMI. Normal glucose tolerance (NGT) and BMI < 25 kg/m2 were defined as normal, and hyperfiltration was defined as the upper 95% confidence interval of the relationship of aging and GFR in normal cases, and compared with GFR > 125 mL/min. RESULTS: GFR without BSA correction and UAE in non-NGT subjects with obesity were higher than in other groups, but GFR with BSA correction did not show this relationship. In multiple regression analysis, BMI was independently associated with GFR without BSA correction, but not with BSA correction. Aging was consistently associated with GFR. The prevalence of hyperfiltration by our definition (GFR = −0.883 × Age + 167.398) was significantly higher than that using GFR > 125 mL/min (P < 0.0001). Hyperfiltration in obesity and/or glucose tolerance disorder should be evaluated using GFR without BSA correction and including the decline of GFR due to aging.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Molitch ME, DeFronzo RA, Franz MJ, Keane WF, Mogensen CE, Parving HH, et al. Diabetic nephropathy. Diabetes Care. 2003;26:S94–8.
Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020;43:487–93.
Cardoso CRL, Leite NC, Salles GC, Ferreira MT, Salles GF. Aortic stiffness and ambulatory blood pressure as predictors of diabetic kidney disease: a competing risks analysis from the Rio de Janeiro Type 2 Diabetes Cohort Study. Diabetologia 2018;61:455–65.
Araki E, Goto A, Kondo T, Noda M, Noto H, Origasa H, et al. Japanese Clinical Practice Guideline for Diabetes 2019. J Diabetes Investig. 2020;11:1020–76.
Jerums G, Premaratne E, Panagiotopoulos S, MacIsaac RJ. The clinical significance of hyperfiltration in diabetes. Diabetologia 2010;53:2093–104.
Ruggenenti P, Porrini EL, Gaspari F, Motterlini N, Cannata A, Carrara F, et al. Glomerular hyperfiltration and renal disease progression in type 2 diabetes. Diabetes Care. 2012;35:2061–8.
Peti-Peterdi J, Kang JJ, Toma I. Activation of the renal renin-angiotensin system in diabetes-new concepts. Nephrol Dial Transpl. 2008;23:3047–9.
Chagnac A, Weinstein T, Korzets A, Ramadan E, Hirsch J, Gafter U. Glomerular hemodynamics in severe obesity. Am J Physiol Ren Physiol. 2000;278:F817–22.
Hara K, Boutin P, Mori Y, Tobe K, Dina C, Yasuda K, et al. Genetic variation in the gene encoding adiponectin is associated with an increased risk of type 2 diabetes in the Japanese population. Diabetes 2002;51:536–40.
Tsuda A, Ishimura E, Uedono H, Ochi A, Nakatani S, Morioka T, et al. Association of Albuminuria With Intraglomerular Hydrostatic Pressure and Insulin Resistance in Subjects With Impaired Fasting Glucose and/or Impaired Glucose Tolerance. Diabetes Care. 2018;41:2414–20.
Cortinovis M, Perico N, Ruggenenti P, Remuzzi A, Remuzzi G. Glomerular hyperfiltration. Nat Rev Nephrol. 2022;18:435–51.
Denic A, Lieske JC, Chakkera HA, Poggio ED, Alexander MP, Singh P, et al. The Substantial Loss of Nephrons in Healthy Human Kidneys with Aging. J Am Soc Nephrol. 2017;28:313–20.
Levey AS, Kramer H. Obesity, glomerular hyperfiltration, and the surface area correction. Am J Kidney Dis. 2010;56:255–8.
Ethics Committee of the Transplantation S. The consensus statement of the Amsterdam Forum on the Care of the Live Kidney Donor. Transplantation 2004;78:491–2.
Takahashi H, Mori M. [Characteristics and significance of criteria for obesity disease in Japan 2011]. Nihon Rinsho. 2013;71:257–61.
Horio M, Imai E, Yasuda Y, Hishida A, Matsuo S. Simple sampling strategy for measuring inulin renal clearance. Clin Exp Nephrol. 2009;13:50–4.
Tsuda A, Inaba M, Ichii M, Ochi A, Ohno Y, Nakatani S, et al. Relationship between serum TSH levels and intrarenal hemodynamic parameters in euthyroid subjects. Eur J Endocrinol. 2013;169:45–50.
Tsuda A, Ishimura E, Ohno Y, Ichii M, Nakatani S, Mori K, et al. Significant association of poor glycemic control with increased resistance in efferent arterioles-study of inulin and para-aminohippuric acid clearance in humans. Diabetes Res Clin Pr. 2014;104:234–40.
Tsuda A, Ishimura E, Ohno Y, Ichii M, Nakatani S, Machida Y, et al. Poor glycemic control is a major factor in the overestimation of glomerular filtration rate in diabetic patients. Diabetes Care. 2013. e-pub ahead of print 2013/10/17doi:dc13-1899 [pii]10.2337/dc13-1899)
Fliser D, Dikow R, Demukaj S, Ritz E. Opposing effects of angiotensin II on muscle and renal blood flow under euglycemic conditions. J Am Soc Nephrol: JASN. 2000;11:2001–6.
Daniele G, Winnier D, Mari A, Bruder J, Fourcaudot M, Pengou Z, et al. Sclerostin and insulin resistance in prediabetes: evidence of a cross talk between bone and glucose metabolism. Diabetes Care. 2015;38:1509–17.
American Diabetes A. Standards of medical care in diabetes-2014. Diabetes Care. 2014;37:S14–80.
Sun ZJ, Yang YC, Wu JS, Wang MC, Chang CJ, Lu FH. Increased risk of glomerular hyperfiltration in subjects with impaired glucose tolerance and newly diagnosed diabetes. Nephrol Dial Transpl. 2016;31:1295–301.
Berg UB. Differences in decline in GFR with age between males and females. Reference data on clearances of inulin and PAH in potential kidney donors. Nephrol Dial Transpl. 2006;21:2577–82.
Delanaye P, Radermecker RP, Rorive M, Depas G, Krzesinski JM. Indexing glomerular filtration rate for body surface area in obese patients is misleading: concept and example. Nephrol Dial Transpl. 2005;20:2024–8.
Hommos MS, Glassock RJ, Rule AD. Structural and functional changes in human kidneys with healthy aging. J Am Soc Nephrol. 2017;28:2838–44.
Hall JE. Guyton & hall physiology review. (e-pub ahead of print 4. Published 4.). 4. edn. Elsevier, Inc: Philadelphia, 2020.
Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152:561–7.
Schlaich MP, Schmitt D, Ott C, Schmidt BMW, Schmieder RE. Basal nitric oxide synthase activity is a major determinant of glomerular haemodynamics in humans. J Hypertens. 2008;26:110–6.
Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129–40.
Kiya M, Tamura Y, Takeno K, Someya Y, Kakehi S, Sato M, et al. Adipose insulin resistance and decreased adiponectin are correlated with metabolic abnormalities in nonobese men. J Clin Endocrinol Metab. 2021;106:e2228–e38.
Tomiyama H, Vlachopoulos C, Xaplanteris P, Nakano H, Shiina K, Ishizu T, et al. Usefulness of the SAGE score to predict elevated values of brachial-ankle pulse wave velocity in Japanese subjects with hypertension. Hypertens Res. 2020;43:1284–92.
Bohlen HG. Nitric oxide and the cardiovascular system. Compr Physiol. 2015;5:808–23.
Horio M, Yasuda Y, Kaimori J, Ichimaru N, Isaka Y, Takahara S, et al. Performance of the Japanese GFR equation in potential kidney donors. Clin Exp Nephrol. 2012;16:415–20.
Tsuda A, Ishimura E, Ohno Y, Ichii M, Nakatani S, Machida Y, et al. Poor glycemic control is a major factor in the overestimation of glomerular filtration rate in diabetic patients. Diabetes Care. 2014;37:596–603.
De Cosmo S, Menzaghi C, Prudente S, Trischitta V. Role of insulin resistance in kidney dysfunction: insights into the mechanism and epidemiological evidence. Nephrol Dial Transpl. 2013;28:29–36.
Ozarda Y, Sikaris K, Streichert T, Macri J, intervals ICoR, Decision L. Distinguishing reference intervals and clinical decision limits - A review by the IFCC Committee on Reference Intervals and Decision Limits. Crit Rev Clin Lab Sci. 2018;55:420–31.
Source of funding
This study was not funded by a grant from a funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
AT and EI acquired the data and wrote the manuscript. AT, KM, HU, SN, YN, MK, SY, TM, JU, and ME contributed to the discussion and reviewed the manuscript. AT had full access to all study data and took responsibility for the integrity of the data and accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsuda, A., Mori, K., Uedono, H. et al. Definition of hyperfiltration taking into account age-related decline in renal function in kidney donor candidates with obesity and glucose tolerance disorder. Hypertens Res 48, 1115–1124 (2025). https://doi.org/10.1038/s41440-024-02020-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-024-02020-y
Keywords
This article is cited by
-
Redefining glomerular hyperfiltration: pathophysiology, clinical implications, and novel perspectives
Hypertension Research (2025)
-
Response to Tsuda et al.: the glomerular filtration rate is both age and allometrically influenced
Hypertension Research (2025)