Abstract
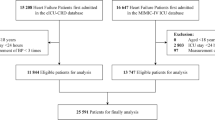
Long-term blood pressure (BP) variability (BPV) is associated with adverse prognosis in patients with heart failure. However, the clinical significance of very short-term (beat-to-beat) BPV is unclear. We collected data on nighttime pulse transit time-based continuous beat-to-beat BP measurement in patients with heart failure (n = 366, median age 72.0, male sex 53.3%). Coefficient of variation (CoV) of pulse transit time-based BP was considered as very short-term BPV. The primary outcome was a composite of heart failure hospitalization or cardiac death. Median values (25th and 75th percentiles) of systolic and diastolic BP CoV were 3.6% (2.8%, 4.5%) and 5.1% (3.8%, 6.5%), respectively. During a median follow-up period of 1084 days after BPV evaluation, 71 patients experienced the primary outcome. When the patients were divided into tertiles based on the systolic and diastolic BPV, the primary outcome occurred most frequently in the highest tertile of BPV. Multivariable Cox proportional hazard analysis revealed that systolic and diastolic BPV, as continuous variables, were independently associated with the primary outcome (hazard ratio 1.199 and 1.101, respectively). In conclusion, high nighttime very short-term BPV was associated with adverse prognosis in patients with heart failure.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Suzuki Y, Kaneko H, Okada A, Fujiu K, Takeda N, Morita H, et al. BP classification using the 2017 ACC/AHA BP guidelines with risk of cardiovascular events in older individuals. J Cardiol. 2024;84:394–403.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32:2285–95.
Butler J, Kalogeropoulos AP, Georgiopoulou VV, Bibbins-Domingo K, Najjar SS, Sutton-Tyrrell KC, et al. Systolic blood pressure and incident heart failure in the elderly. The Cardiovascular Health Study and the Health, Ageing and Body Composition Study. Heart. 2011;97:1304–11.
Group SR, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl J Med. 2015;373:2103–16.
Mancia G, Bombelli M, Facchetti R, Madotto F, Corrao G, Trevano FQ, et al. Long-term prognostic value of blood pressure variability in the general population: results of the Pressioni Arteriose Monitorate e Loro Associazioni Study. Hypertension. 2007;49:1265–70.
Mancia G. Short- and long-term blood pressure variability: present and future. Hypertension. 2012;60:512–7.
Sheikh AB, Sobotka PA, Garg I, Dunn JP, Minhas AMK, Shandhi MMH, et al. Blood Pressure Variability in Clinical Practice: Past, Present and the Future. J Am Heart Assoc. 2023;12:e029297.
Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol. 2013;10:143–55.
Narita K, Shimbo D, Kario K. Assessment of blood pressure variability: characteristics and comparison of blood pressure measurement methods. Hypertens Res. 2024;47:3345–55.
Mehlum MH, Liestol K, Kjeldsen SE, Julius S, Hua TA, Rothwell PM, et al. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J. 2018;39:2243–51.
Suchy-Dicey AM, Wallace ER, Mitchell SV, Aguilar M, Gottesman RF, Rice K, et al. Blood pressure variability and the risk of all-cause mortality, incident myocardial infarction, and incident stroke in the cardiovascular health study. Am J Hypertens. 2013;26:1210–7.
Kario K, Kanegae H, Hoshide S. Home blood pressure stability score is associated with better cardiovascular prognosis: data from the nationwide prospective J-HOP study. Hypertens Res. 2024. https://doi.org/10.1038/s41440-024-01940-z. e-pub ahead of print 20241012.
Chichareon P, Methavigul K, Lip GYH, Krittayaphong R. Systolic blood pressure visit-to-visit variability and outcomes in Asian patients with atrial fibrillation. Hypertens Res. 2024;47:1479–89.
Gesche H, Grosskurth D, Kuchler G, Patzak A. Continuous blood pressure measurement by using the pulse transit time: comparison to a cuff-based method. Eur J Appl Physiol. 2012;112:309–15.
Misaka T, Niimura Y, Yoshihisa A, Wada K, Kimishima Y, Yokokawa T, et al. Clinical impact of sleep-disordered breathing on very short-term blood pressure variability determined by pulse transit time. J Hypertens. 2020;38:1703–11.
Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–26.
Vidan MT, Bueno H, Wang Y, Schreiner G, Ross JS, Chen J, et al. The relationship between systolic blood pressure on admission and mortality in older patients with heart failure. Eur J Heart Fail. 2010;12:148–55.
Sato Y, Yoshihisa A, Oikawa M, Nagai T, Yoshikawa T, Saito Y, et al. Relation of Systolic Blood Pressure on the Following Day with Post-Discharge Mortality in Hospitalized Heart Failure Patients with Preserved Ejection Fraction. Int Heart J. 2019;60:876–85.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e263–e421.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Tsutsui H, Isobe M, Ito H, Ito H, Okumura K, Ono M, et al. JCS 2017/JHFS 2017 Guideline on Diagnosis and Treatment of Acute and Chronic Heart Failure- Digest Version. Circ J. 2019;83:2084–184.
Monzo L, Ferreira JP, Abreu P, Szumski A, Bohm M, McMurray JJV, et al. Visit-to-visit blood pressure variation and outcomes in heart failure with reduced ejection fraction: findings from the Eplerenone in Patients with Systolic Heart Failure and Mild Symptoms trial. J Hypertens. 2020;38:420–5.
Ferreira JP, Duarte K, Pitt B, Dickstein K, McMurray JJV, Zannad F, et al. Visit-to-visit blood pressure variation is associated with outcomes in a U-shaped fashion in patients with myocardial infarction complicated with systolic dysfunction and/or heart failure: findings from the EPHESUS and OPTIMAAL trials. J Hypertens. 2018;36:1736–42.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Misaka T, Sato Y, Sugawara Y, Ogawara R, Ichimura S, Tomita Y, et al. Elevated blood bicarbonate levels and long-term adverse outcomes in patients with chronic heart failure. ESC Heart Fail. 2024. https://doi.org/10.1002/ehf2.14900.
Ichimura S, Misaka T, Ogawara R, Tomita Y, Anzai F, Sato Y, et al. Neutrophil Extracellular Traps in Myocardial Tissue Drive Cardiac Dysfunction and Adverse Outcomes in Patients With Heart Failure With Dilated Cardiomyopathy. Circ Heart Fail. 2024;17:e011057.
Ogawara R, Misaka T, Ohashi N, Ichimura S, Tomita Y, Tani T, et al. Very short-term blood pressure variability by pulse transit time-based measurements during night-time predicts future cardiovascular events in patients with ischemic heart disease. Clin Res Cardiol. 2024. https://doi.org/10.1007/s00392-024-02539-7.
Sato Y, Yoshihisa A, Sugawara Y, Misaka T, Sato T, Kaneshiro T, et al. Malnutrition stratified by marasmus and kwashiorkor in adult patients with heart failure. Sci Rep. 2024;14:19722.
Rickham PP. Human Experimentation. Code of Ethics of the World Medical Association. Declaration of Helsinki. Br Med J 1964;2:177.
Ferber R, Millman R, Coppola M, Fleetham J, Murray CF, Iber C, et al. Portable recording in the assessment of obstructive sleep apnea. ASDA Stand Pract Sleep. 1994;17:378–92.
Misaka T, Yoshihisa A, Yokokawa T, Takeishi Y. Effects of continuous positive airway pressure on very short-term blood pressure variability associated with sleep-disordered breathing by pulse transit time-based blood pressure measurements. J Hypertens. 2023;41:733–40.
Hamaguchi S, Tsuchihashi-Makaya M, Kinugawa S, Yokota T, Ide T, Takeshita A, et al. Chronic kidney disease as an independent risk for long-term adverse outcomes in patients hospitalized with heart failure in Japan. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73:1442–7.
Hamaguchi S, Tsuchihashi-Makaya M, Kinugawa S, Yokota T, Takeshita A, Yokoshiki H, et al. Anemia is an independent predictor of long-term adverse outcomes in patients hospitalized with heart failure in Japan. A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73:1901–8.
Parati G, Ochoa JE, Bilo G. Blood pressure variability, cardiovascular risk, and risk for renal disease progression. Curr Hypertens Rep. 2012;14:421–31.
Hartupee J, Mann DL. Neurohormonal activation in heart failure with reduced ejection fraction. Nat Rev Cardiol. 2017;14:30–8.
Schrier RW. Water and sodium retention in edematous disorders: role of vasopressin and aldosterone. Am J Med. 2006;119:S47–53.
Minatoguchi S. Heart failure and its treatment from the perspective of sympathetic nerve activity. J Cardiol. 2022;79:691–7.
Arundel C, Lam PH, Gill GS, Patel S, Panjrath G, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Reduced Ejection Fraction. J Am Coll Cardiol. 2019;73:3054–63.
Ide T, Kaku H, Matsushima S, Tohyama T, Enzan N, Funakoshi K, et al. Clinical Characteristics and Outcomes of Hospitalized Patients With Heart Failure From the Large-Scale Japanese Registry Of Acute Decompensated Heart Failure (JROADHF). Circ J. 2021;85:1438–50.
Tsimploulis A, Lam PH, Arundel C, Singh SN, Morgan CJ, Faselis C, et al. Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction. JAMA Cardiol. 2018;3:288–97.
Mitchell GF. Arterial Stiffness in Aging: Does It Have a Place in Clinical Practice?: Recent Advances in Hypertension. Hypertension. 2021;77:768–80.
Wilcox JE, Fang JC, Margulies KB, Mann DL. Heart Failure With Recovered Left Ventricular Ejection Fraction: JACC Scientific Expert Panel. J Am Coll Cardiol. 2020;76:719–34.
Tsutsui H, Momomura SI, Saito Y, Ito H, Yamamoto K, Sakata Y, et al. Incidence and risk factors of hypotension-related adverse events among Japanese patients with heart failure receiving sacubitril/valsartan or enalapril: Results from the PARALLEL-HF study. J Cardiol. 2024. https://doi.org/10.1016/j.jjcc.2024.09.002.
Girerd N, Coiro S, Benson L, Savarese G, Dahlstrom U, Rossignol P, et al. Hypotension in heart failure is less harmful if associated with high or increasing doses of heart failure medication: Insights from the Swedish Heart Failure Registry. Eur J Heart Fail. 2024;26:359–69.
Sogunuru GP, Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, et al. Morning surge in blood pressure and blood pressure variability in Asia: Evidence and statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:324–34.
Acknowledgements
The authors thank Kumiko Watanabe, Yumi Yoshihisa, Shiori Togashi, and Tomiko Miura for their technical assistance. The acquisition of data was supported by Ayumi Haneda, Akito Endo, Mari Hoshi, Manami Akimoto, Mimori Itami, Shiori Urayama, and Yuuichi Yokoyama from the Office for Diversity and Inclusion, Fukushima Medical University, Fukushima, Japan. The present study was supported in part by grants-in-aid for Scientific Research (23K06870 and 24K18648) from the Japan Society for the Promotion of Science.
Funding
Grant-in-aid for Scientific Research (23K06870 and 24K18648) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sato, Y., Yoshihisa, A., Ohashi, N. et al. Association of nighttime very short-term blood pressure variability determined by pulse transit time with adverse prognosis in patients with heart failure. Hypertens Res 48, 1305–1314 (2025). https://doi.org/10.1038/s41440-025-02102-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02102-5
Keywords
This article is cited by
-
Nighttime phenotype in patients with heart failure: beat-to-beat blood pressure variability predicts prognosis
Hypertension Research (2025)
-
Comment on âAssociation of nighttime very short-term blood pressure variability determined by pulse transit time with adverse prognosis in patients with heart failureâ
Hypertension Research (2025)