Abstract
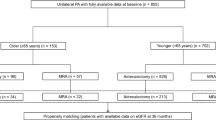
Emerging evidence has suggested a significant prevalence of mild autonomous cortisol secretion (MACS) among patients diagnosed with primary aldosteronism (PA). However, MACS’s clinical characteristics and implications in PA patients remain largely unexplored. To investigate the prevalence, comorbidities, and indicators of MACS in PA patients, we conducted a retrospective cohort study including 874 PA patients with dexamethasone suppression test results in the Taiwan Primary Aldosteronism Investigators (TAIPAI) cohort between February 2011 and February 2024. Additionally, we performed a systematic review and meta-analysis of 11 studies, encompassing a total of 2882 PA patients (CRD42023486755). After including the TAIPAI cohort data in the meta-analysis, the prevalence of MACS among PA patients was 21.9% (95% confidence interval [C.I.]: 18.1, 26.2), with a negative correlation with estimated glomerular filtration rate (eGFR) (r = –0.028, P < 0.01). The characteristics associated with MACS in PA patients included older age (mean difference [MD] = 5.51 year, P < 0.01), higher plasma aldosterone concentration (MD = 5.36 ng/dL, P < 0.01), lower plasma renin activity (MD = –0.15 ng/mL/h, P < 0.01), lower eGFR (MD = -4.91 mL/min/1.73 m2, P = 0.01), and larger adrenal tumor size (MD = 0.41 cm, P < 0.01). MACS was significantly associated with chronic kidney disease (odds ratio [OR] = 1.96, P < 0.01), diabetes mellitus (OR = 1.60, P = 0.04), and cardiovascular diseases (OR = 1.37, P = 0.02) among PA patients. The high prevalence and strong association of MACS with comorbidities underscore the importance of identifying it in PA patients. Clinical features such as advanced age, significant aldosterone-renin dysregulation, impaired kidney function, diabetes, cardiovascular disease, and large adrenal tumors are indicators for MACS screening in PA patients.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Vaidya A, Mulatero P, Baudrand R, Adler GK. The expanding spectrum of primary aldosteronism: implications for diagnosis, pathogenesis, and treatment. Endocr Rev. 2018;39:1057–88.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Colussi G, Catena C, Lapenna R, Nadalini E, Chiuch A, Sechi LA. Insulin resistance and hyperinsulinemia are related to plasma aldosterone levels in hypertensive patients. Diab care. 2007;30:2349–54.
Remde H, Hanslik G, Rayes N, Quinkler M. Glucose metabolism in primary aldosteronism. Horm Metab Res = Horm- und Stoffwechselforschung = Hormones et Metab. 2015;47:987–93.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diab Endocrinol. 2018;6:41–50.
Rossi R, Tauchmanova L, Luciano A, Di Martino M, Battista C, Del Viscovo L, et al. Subclinical Cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J Clin Endocrinol Metab. 2000;85:1440–8.
Fassnacht M, Tsagarakis S, Terzolo M, Tabarin A, Sahdev A, Newell-Price J, et al. European Society of Endocrinology clinical practice guidelines on the management of adrenal incidentalomas, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2023;189:G1–g42.
Prete A, Bancos I. Mild autonomous cortisol secretion: pathophysiology, comorbidities and management approaches. Nat Rev Endocrinol. 2024;20:460–73.
Nakajima Y, Yamada M, Taguchi R, Satoh T, Hashimoto K, Ozawa A, et al. Cardiovascular complications of patients with aldosteronism associated with autonomous cortisol secretion. J Clin Endocrinol Metab. 2011;96:2512–8.
Fujimoto K, Honjo S, Tatsuoka H, Hamamoto Y, Kawasaki Y, Matsuoka A, et al. Primary aldosteronism associated with subclinical Cushing syndrome. J Endocrinol Invest. 2013;36:564–7.
Gerards J, Heinrich DA, Adolf C, Meisinger C, Rathmann W, Sturm L, et al. Impaired glucose metabolism in primary aldosteronism is associated with cortisol cosecretion. J Clin Endocrinol Metab. 2019;104:3192–202.
Hiraishi K, Yoshimoto T, Tsuchiya K, Minami I, Doi M, Izumiyama H, et al. Clinicopathological features of primary aldosteronism associated with subclinical Cushing’s syndrome. Endocr J. 2011;58:543–51.
Yasuda S, Hikima Y, Kabeya Y, Iida S, Oikawa Y, Isshiki M, et al. Clinical characterization of patients with primary aldosteronism plus subclinical Cushing’s syndrome. BMC Endocr Disord. 2020;20:9.
Peng K-Y, Liao H-W, Chan C-K, Lin W-C, Yang S-Y, Tsai Y-C, et al. Presence of subclinical hypercortisolism in clinical aldosterone-producing adenomas predicts lower clinical success. Hypertension. 2020;76:1537–44.
Hung K, Lee BC, Chen PT, Liu KL, Chang CC, Wu VC, et al. Influence of autonomous cortisol secretion in patients with primary aldosteronism: subtype analysis and postoperative outcome. Endocr Connect. 2023;12:e230121.
Heinrich DA, Adolf C, Holler F, Lechner B, Schneider H, Riester A, et al. Adrenal insufficiency after unilateral adrenalectomy in primary aldosteronism: long-term outcome and clinical impact. J Clin Endocrinol Metab. 2019;104:5658–64.
Wu VC, Hu YH, Wu CH, Kao CC, Wang CY, Yang WS, et al. Administrative data on diagnosis and mineralocorticoid receptor antagonist prescription identified patients with primary aldosteronism in Taiwan. J Clin Epidemiol. 2014;67:1139–49.
Wu VC, Yang SY, Lin JW, Cheng BW, Kuo CC, Tsai CT, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta. 2011;412:1319–25.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism-the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Barker TH, Migliavaca CB, Stein C, Colpani V, Falavigna M, Aromataris E, et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med Res Methodol. 2021;21:189.
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49:1–15.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Tabuchi Y, Otsuki M, Kasayama S, Kosugi K, Hashimoto K, Yamamoto T, et al. Clinical and endocrinological characteristics of adrenal incidentaloma in Osaka region, Japan. Endocr J. 2016;63:29–35.
Inoue K, Yamazaki Y, Tsurutani Y, Suematsu S, Sugisawa C, Saito J, et al. Evaluation of cortisol production in aldosterone-producing adenoma. Horm Metab Res. 2017;49:847–53.
Bhatt PS, Sam AH, Meeran KM, Salem V. The relevance of cortisol co-secretion from aldosterone-producing adenomas. Hormones. 2019;18:307–13.
Gendreitzig P, Künzel HE, Adolf C, Handgriff L, Müller L, Holler F, et al. Autonomous cortisol secretion influences psychopathological symptoms in patients with primary aldosteronism. J Clin Endocrinol Metab. 2021;106:E2423–E33.
Kometani M, Yoneda T, Demura M, Aono D, Gondoh Y, Karashima S, et al. Genetic and epigenetic analyses of aldosterone-producing adenoma with hypercortisolemia. Steroids. 2019;151:6.
O’Toole SM, Sze W-CC, Chung T-T, Akker SA, Druce MR, Waterhouse M, et al. Low-grade cortisol cosecretion has limited impact on ACTH-stimulated AVS parameters in primary aldosteronism. J Clin Endocrinol Metab. 2020;105:e3776–e84.
Araujo-Castro M, Paja Fano M, Pla Peris B, González Boillos M, Pascual-Corrales E, García-Cano AM, et al. Autonomous cortisol secretion in patients with primary aldosteronism: prevalence and implications on cardiometabolic profile and on surgical outcomes. Endocr Connect. 2023;12:e230043.
Katabami T, Matsuba R, Kobayashi H, Nakagawa T, Kurihara I, Ichijo T, et al. Primary aldosteronism with mild autonomous cortisol secretion increases renal complication risk. Eur J Endocrinol. 2022;186:645–55.
Q-Q Plot (Quantile to Quantile Plot). In: The Concise Encyclopedia of Statistics.https://doi.org/10.1007/978-0-387-32833-1_331) Springer New York: New York, NY, 2008, 437-9.
Egger M, Smith Davey, Schneider G, Minder M. C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Olsen H, Olsen M. Associations of age, BMI, and renal function to cortisol after dexamethasone suppression in patients with adrenal incidentalomas. Front Endocrinol. 2023;13:1055298.
Li X, Xiang X, Hu J, Goswami R, Yang S, Zhang A, et al. Association between serum cortisol and chronic kidney disease in patients with essential hypertension. Kidney Blood Press Res. 2016;41:384–91.
Lai CF, Lin YH, Huang KH, Chueh JS, Wu VC. Kidney function predicts new-onset cardiorenal events and mortality in primary aldosteronism: approach of the 2021 race-free eGFR equation. Hypertens Res. 2024;47:233–44.
Kjellbom A, Lindgren O, Puvaneswaralingam S, Löndahl M, Olsen H. Association between mortality and levels of autonomous cortisol secretion by adrenal incidentalomas : a cohort study. Ann Intern Med. 2021;174:1041–9.
Singh S, Atkinson EJ, Achenbach SJ, LeBrasseur N, Bancos I. Frailty in patients with mild autonomous cortisol secretion is higher than in patients with nonfunctioning adrenal tumors. J Clin Endocrinol Metab. 2020;105:e3307–e15.
Catena C, Lapenna R, Baroselli S, Nadalini E, Colussi G, Novello M, et al. Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J Clin Endocrinol Metab. 2006;91:3457–63.
Fallo F, Veglio F, Bertello C, Sonino N, Della Mea P, Ermani M, et al. Prevalence and characteristics of the metabolic syndrome in primary aldosteronism. J Clin Endocrinol Metab. 2006;91:454–9.
Wu VC, Chan CK, Wu WC, Peng KY, Chang YS, Yeh FY, et al. New-onset diabetes mellitus risk associated with concurrent autonomous cortisol secretion in patients with primary aldosteronism. Hypertension Res. 2023;46:445–55.
Yokota K, Sone M. Autonomous cortisol secretion in patients with primary aldosteronism: a possible risk factor for new-onset diabetes mellitus. Hypertens Res. 2023;46:803–5.
Jiang Y, Zhou L, Zhang C, Su T, Jiang L, Zhou W, et al. The influence of cortisol co-secretion on clinical characteristics and postoperative outcomes in unilateral primary aldosteronism. Front Endocrinol (Lausanne). 2024;15:1369582.
Tauchmanovà L, Rossi R, Biondi B, Pulcrano M, Nuzzo V, Palmieri EA, et al. Patients with subclinical Cushing’s syndrome due to adrenal adenoma have increased cardiovascular risk. J Clin Endocrinol Metab. 2002;87:4872–8.
Adolf C, Köhler A, Franke A, Lang K, Riester A, Löw A, et al. Cortisol excess in patients with primary aldosteronism impacts left ventricular hypertrophy. J Clin Endocrinol Metab. 2018;103:4543–52.
Brosolo G, Catena C, Da Porto A, Bulfone L, Vacca A, Verheyen ND, et al. Differences in regulation of cortisol secretion contribute to left ventricular abnormalities in patients with essential hypertension. Hypertension (Dallas, Tex : 1979). 2022;79:1435–44.
Tsai CH, Liao CW, Wu XM, Chen ZW, Pan CT, Chang YY, et al. Autonomous cortisol secretion is associated with worse arterial stiffness and vascular fibrosis in primary aldosteronism: a cross-sectional study with follow-up data. Eur J Endocrinol. 2022;187:197–208.
Lee B-C, Chang C-C, Kang VJ-W, Huang J-Z, Lin Y-L, Chang Y-Y, et al. Autonomous cortisol secretion promotes vascular calcification in vivo and in vitro under hyperaldosteronism. Hypertens Res. 2025;48:366–77.
Bleier J, Pickovsky J, Apter S, Fishman B, Dotan Z, Tirosh A, et al. The association between adrenal adenoma size, autonomous cortisol secretion and metabolic derangements. Clin Endocrinol. 2022;96:311–8.
Wu WC, Peng KY, Lu JY, Chan CK, Wang CY, Tseng FY, et al. Cortisol-producing adenoma-related somatic mutations in unilateral primary aldosteronism with concurrent autonomous cortisol secretion: their prevalence and clinical characteristics. Eur J Endocrinol. 2022;187:519–30.
Acknowledgements
We thank Mrs. Yi-Jin Hsiao for her assistance in statistical analysis. We also thank the staff of the Second and Seventh Core Labs, Department of Medical Research at National Taiwan University Hospital, for technical assistance. We express sincere gratitude to all staff of the Taiwan Clinical Trial Consortium.
Funding
This work was supported by the National Science and Technology Council, Taiwan (110-2314-B-002-239, 111-2314-B-002-046); National Taiwan University Hospital (UN110-030); Ministry of Health and Welfare, Taiwan (110-TDU-B-212-124005); Mrs. Hsiu-Chin Lee Kidney Research Fund. The funds played no role in the study design, data collection, analysis and interpretation, manuscript writing, or in the decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, C., Chang, LY., Sheu, JY. et al. Exploring the high prevalence, comorbidities, and indicators of mild autonomous cortisol secretion in primary aldosteronism: a cohort study and systematic review. Hypertens Res 48, 1716–1729 (2025). https://doi.org/10.1038/s41440-025-02172-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02172-5
Keywords
This article is cited by
-
A systematic review to compare adrenalectomy and mineralocorticoid receptor antagonists in patients with unilateral primary aldosteronism
Hypertension Research (2025)
-
Mild autonomous cortisol secretion in primary aldosteronism: the origin of cortisol
Hypertension Research (2025)