Abstract
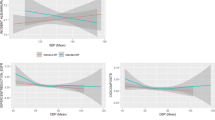
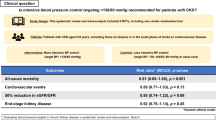
Time in target range (TTR) of systolic blood pressure is a novel measure to assess the effect of blood pressure control. However, few studies have explored the renoprotective value of systolic TTR in patients with type 2 diabetes (T2D). We analyzed the database of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) blood pressure (BP) trial. The systolic target range was established as 120–140 and 110–130 mm Hg for the standard group and intensive therapy, respectively. Multivariate linear regression was conducted to evaluate the relationship between systolic blood pressure and estimated glomerular filtration rate (eGFR) slope. After adjusting for covariates, systolic TTR showed a significant and positive association with two measures of eGFR slope (n = 4327, P < 0.04). The correlation of systolic TTR and eGFR slope was notably stronger in CKD patients (n = 1635) compared to those without (P for interaction < 0.05). When analyzing systolic TTR as a categorical variable, participants with CKD in the highest systolic TTR quantile had a significantly positive relationship with eGFR slope (P ≤ 0.0001). These findings were consistently observed across further subgroup analyses. Among T2D patients, systolic TTR exhibited a significant and positive relation to eGFR slope, with a stronger relationship noted in individuals diagnosed with CKD. This underscores the critical role of stable blood pressure control for renoprotection in patients with T2D, particularly in those with CKD. (Trial Registration: ClinicalTrials.gov number: NCT00000620).

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Derakhshan A, Bagherzadeh-Khiabani F, Arshi B, Ramezankhani A, Azizi F, Hadaegh F. Different combinations of glucose tolerance and blood pressure status and incident diabetes, hypertension, and chronic kidney disease. J Am Heart Assoc. 2016;55:e003917.
Hu G, Jousilahti P, Tuomilehto J. Joint effects of history of hypertension at baseline and type 2 diabetes at baseline and during follow-up on the risk of coronary heart disease. Eur Heart J. 2007;28:3059–66.
Ndumele CE, Rangaswami J, Chow SL, Neeland IJ, Tuttle KR, Khan SS, et al. Cardiovascular-kidney-metabolic health: a presidential advisory from the American Heart Association. Circulation. 2023;148:1606–35.
Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, et al. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension. 2013;61:964–71.
Pechere-Bertschi A, Greminger P, Hess L, Philippe J, Ferrari P. Swiss Hypertension and Risk Factor Program (SHARP): cardiovascular risk factors management in patients with type 2 diabetes in Switzerland. Blood Press. 2005;14:337–44.
Oizumi T, Daimon M, Jimbu Y, Wada K, Kameda W, Susa S, et al. Impaired glucose tolerance is a risk factor for stroke in a Japanese sample - the Funagata study. Metabolism. 2008;57:333–8.
Cui RZ, Iso H, Yamagishi K, Saito I, Kokubo Y, Inoue M, et al. Diabetes Mellitus and Risk of Stroke and Its Subtypes Among Japanese The Japan Public Health Center Study. Stroke. 2011;42:2611–4.
Van Buren PN, Toto R. Hypertension in diabetic nephropathy: epidemiology, mechanisms, and management. Adv Chronic Kidney Dis. 2011;18:28–41.
Mancia Chairperson G, Kreutz Co-Chair R, Brunstrom M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension Endorsed by the European Renal Association (ERA) and the International Society of Hypertension (ISH). J Hypertens. 2023;41:1874–2071.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e426–e483.
Berlowitz DR, Ash AS, Hickey EC, Glickman M, Friedman R, Kader B. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003;26:355–9.
Mancia G. Effects of intensive blood pressure control in the management of patients with type 2 diabetes mellitus in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Circulation. 2010;122:847–9.
Doumas M, Tsioufis C, Fletcher R, Amdur R, Faselis C, Papademetriou V. Time in therapeutic range, as a determinant of all-cause mortality in patients with hypertension. J Am Heart Assoc. 2017;6:e007131.
Chen KY, Li C, Cornelius V, Yu DH, Wang Q, Shi R, et al. Prognostic value of time in blood pressure target range among patients with heart failure. Jacc-Heart Fail. 2022;10:369–79.
Cheng Y, Wang D, Yang Y, Miao Y, Shen WL, Tian J, et al. Diastolic and systolic blood pressure time in target range as a cardiovascular risk marker in patients with type 2 diabetes: A post hoc analysis of ACCORD BP trial. Diabetes Res Clin Pract. 2023;203:110831.
Warren B, Rebholz CM, Sang Y, Lee AK, Coresh J, Selvin E, et al. Diabetes and trajectories of estimated glomerular filtration rate: a prospective cohort analysis of the atherosclerosis risk in communities study. Diabetes Care. 2018;41:1646–53.
Zoppini G, Targher G, Chonchol M, Ortalda V, Negri C, Stoico V, et al. Predictors of estimated GFR decline in patients with type 2 diabetes and preserved kidney function. Clin J Am Soc Nephrol. 2012;7:401–8.
De Cosmo S, Viazzi F, Piscitelli P, Giorda C, Ceriello A, Genovese S, et al. Blood pressure status and the incidence of diabetic kidney disease in patients with hypertension and type 2 diabetes. J Hypertens. 2016;34:2090–8.
Takao T, Matsuyama Y, Suka M, Yanagisawa H, Kikuchi M, Kawazu S. Time-to-effect relationships between systolic blood pressure and the risks of nephropathy and retinopathy in patients with type 2 diabetes. J Diabetes Complicat. 2014;28:674–8.
Coresh J, Turin TC, Matsushita K, Sang Y, Ballew SH, Appel LJ, et al. Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA. 2014;311:2518–31.
Cushman WC, Grimm RH Jr, Cutler JA, Evans GW, Capes S, Corson MA, et al. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007;99:44i–55i.
Group AS, Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85.
Bonds DE, Craven TE, Buse J, Crouse JR, Cuddihy R, Elam M, et al. Fenofibrate-associated changes in renal function and relationship to clinical outcomes among individuals with type 2 diabetes: the Action to Control Cardiovascular Risk in Diabetes (ACCORD) experience. Diabetologia. 2012;55:1641–50.
Schmitt L, Speckman J, Ansell J. Quality assessment of anticoagulation dose management: comparative evaluation of measures of time-in-therapeutic range. J Thromb Thrombolysis. 2003;15:213–6.
Burrows NR, Koyama A, Pavkov ME. Reported cases of end-stage kidney disease - United States, 2000–2019. MMWR Morb Mortal Wkly Rep. 2022;71:412–5.
Wang Z, do Carmo JM, Aberdein N, Zhou X, Williams JM, da Silva AA, et al. Synergistic interaction of hypertension and diabetes in promoting kidney injury and the role of endoplasmic reticulum stress. Hypertension. 2017;69:879–91.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313:603–15.
Huang RH, Lin YF, Liu MH, Xiong ZY, Zhang SZ, Zhong XB, et al. Time in target range for systolic blood pressure and cardiovascular outcomes in patients with heart failure with preserved ejection fraction. J Am Heart Assoc. 2022;11:e022765.
Fatani N, Dixon DL, Van Tassell BW, Fanikos J, Buckley LF. Systolic blood pressure time in target range and cardiovascular outcomes in patients with hypertension. J Am Coll Cardiol. 2021;77:1290–9.
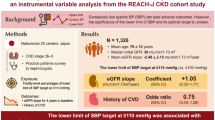
Park C, Kim H, Joo Y, Park J, Chang T, Yoo T, et al. Findings from the KNOW-CKD Study indicate that higher systolic blood pressure time in target range is associated with a lower risk of chronic kidney disease progression. Kidney Int. 2024;105:835–843.
de Galan BE, Perkovic V, Ninomiya T, Pillai A, Patel A, Cass A, et al. Lowering blood pressure reduces renal events in type 2 diabetes. J Am Soc Nephrol. 2009;20:883–92.
Kurasawa S, Yasuda Y, Kato S, Maruyama S, Okada H, Kashihara N, et al. Relationship between the lower limit of systolic blood pressure target and kidney function decline in advanced chronic kidney disease: an instrumental variable analysis from the REACH-J CKD cohort study. Hypertens Res. 2023;46:2478–87.
Decker E, Kendrick J. Research in the CKD clinic: highs and lows. Adv Chronic Kidney Dis. 2014;21:344–8. https://doi.org/10.1053/j.ackd.2014.02.012
Itano S, Kanda E, Nagasu H, Nangaku M, Kashihara N. eGFR slope as a surrogate endpoint for clinical study in early stage of chronic kidney disease: from The Japan Chronic Kidney Disease Database. Clin Exp Nephrol. 2023;27:847–56.
Kovesdy CP, Coresh J, Ballew SH, Woodward M, Levin A, Naimark DMJ, et al. Past decline versus current eGFR and subsequent ESRD risk. J Am Soc Nephrol. 2016;27:2447–55.
Turin TC, Coresh J, Tonelli M, Stevens PE, de Jong PE, Farmer CKT, et al. Change in the estimated glomerular filtration rate over time and risk of all-cause mortality. Kidney Int. 2013;83:684–91.
Oshima M, Jun M, Ohkuma T, Toyama T, Wada T, Cooper ME, et al. The relationship between eGFR slope and subsequent risk of vascular outcomes and all-cause mortality in type 2 diabetes: the ADVANCE-ON study. Diabetologia. 2019;62:1988–97.
Zannad F, Ferreira JP, Pocock SJ, Zeller C, Anker SD, Butler J, et al. Cardiac and kidney benefits of empagliflozin in heart failure across the spectrum of kidney function: Insights From EMPEROR-Reduced. Circulation. 2021;143:310–21.
Tawfik YMK, Van Tassell BW, Dixon DL, Baker WL, Fanikos J, Buckley LF. Effects of Intensive Systolic Blood Pressure Lowering on End-Stage Kidney Disease and Kidney Function Decline in Adults With Type 2 Diabetes Mellitus and Cardiovascular Risk Factors: A Post Hoc Analysis of ACCORD-BP and SPRINT. Diabetes Care. 2023;46:868–73.
Bi Y, Li M, Liu Y, Li T, Lu J, Duan P, et al. Intensive Blood-Pressure Control in Patients with Type 2 Diabetes. N Engl J Med. 2024. Online ahead of print.
Christensen PK, Hansen HP, Parving HH. Impaired autoregulation of GFR in hypertensive non-insulin dependent diabetic patients. Kidney Int. 1997;52:1369–74.
Cupples WA. Interactions contributing to kidney blood flow autoregulation. Curr Opin Nephrol Hypertens. 2007;16:39–45.
Acknowledgements
The investigators acknowledge and thank the ACCORD investigators and the National Heart, Lung, and Blood Institute for conducting the trials and making datasets publicly available.
Funding
This work was supported by the Chinese National Natural Science Foundation (82270452, 82088102, and 81770418), Shanghai Talent Development Fund (2021087), and Ministry of Health (2016YFC1300103 and 2016YFC0905001).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, Y., Zhu, XB., Xu, YL. et al. Time in target range of systolic blood pressure and eGFR slope in patients with type 2 diabetes. Hypertens Res 48, 1787–1798 (2025). https://doi.org/10.1038/s41440-025-02173-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02173-4
Keywords
This article is cited by
-
Role of time in target range in blood pressure management for preventing renal decline in type 2 diabetes
Hypertension Research (2025)