Abstract
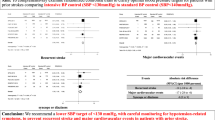
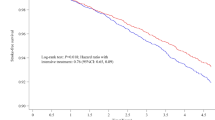
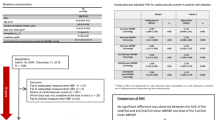
The effect of intensive blood pressure (BP) reduction on the prevention of cardiovascular events in patients with diabetes remains unclear. This study evaluated the impact of intensive BP-lowering on cardiovascular events in patients with diabetes compared to standard treatment. A systematic review and meta-analysis of randomized controlled trials (RCTs) was conducted, comparing intensive treatment (target systolic BP < 130 mmHg or diastolic BP < 80 mmHg) with standard treatment in patients with diabetes. Eligible studies were identified through Ovid MEDLINE, Cochrane Library, and Ichushi. Outcomes included cardiovascular events, coronary artery disease, stroke, all-cause and cardiovascular death, and serious adverse events. Data were analyzed using a random-effects model. Sensitivity analyses were performed to assess the effects of systolic and diastolic BP targets separately. The search identified eight eligible trials comprising 16634 patients with diabetes. Intensive BP-lowering treatment significantly reduced cardiovascular events (risk ratio: 0.848; 95% confidence interval: 0.760, 0.947) and stroke (risk ratio: 0.705; 95% confidence interval: 0.541, 0.918), but not coronary artery disease or all-cause death in analyses including J-DOIT3 trial. Sensitivity analyses showed that DBP-targeted treatment was not associated with the risk of cardiovascular events. Incorporating the latest RCT strengthened the association between intensive treatment and reduced coronary artery disease risk, without significantly increasing the risk of serious adverse events. These findings recommend an intensive BP-lowering strategy targeting SBP < 130 mmHg or DBP < 80 mmHg to prevent cardiovascular events, particularly stroke, in patients with diabetes.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
World Heart Federation. World Heart Report 2023. Confronting the world’s number one killer. 2023:1–52. (https://world-heart-federation.org/resource/world-heart-report-2023/) Accessed on Oct 2nd, 2024.
Mensah GA, Fuster V, Murray CJL, Roth GA. Global burden of cardiovascular diseases and risks, 1990–2022. J Am Coll Cardiol. 2023;82:2350–473.
Blood Pressure Lowering Treatment Trialists. ’ Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–36.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison HC, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:1269–324.
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, et al. ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J 2024. 2024;45:3912–4018.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. International society of hypertension global hypertension practice guidelines. Hypertension 2020. 2020;75:1334–57.
Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Liu J, Li Y, Ge J, Yan X, Zhang H, Zheng X, et al. Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial. Lancet. 2024;404:245–55.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Bi Y, Li M, Liu Y, Li T, Lu J, Duan P, et al. Intensive blood-pressure control in patients with type 2 diabetes. N Engl J Med. 2025;392:1155–67.
Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group Lancet. 1998;351:1755–62.
Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisoldipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998;338:645–52.
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85.
Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, Pearce LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15.
Ueki K, Sasako T, Okazaki Y, Kato M, Okahata S, Katsuyama H, et al. Effect of an intensified multifactorial intervention on cardiovascular outcomes and mortality in type 2 diabetes (J-DOIT3): an open-label, randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5:951–64.
Kitagawa K, Yamamoto Y, Arima H, Maeda T, Sunami N, Kanzawa T, et al. Effect of standard vs intensive blood pressure control on the risk of recurrent stroke: a randomized clinical trial and meta-analysis. JAMA Neurol. 2019;76:1309–18.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
Yang Q, Zheng R, Wang S, Zhu J, Li M, Wang T, et al. Systolic blood pressure control targets to prevent major cardiovascular events and death in patients with type 2 diabetes: a systematic review and network meta-analysis. Hypertension. 2023;80:1640–53.
Ioannidou E, Shabnam S, Abner S, Kaur N, Zaccardi F, Ray KK, et al. Effect of more versus less intensive blood pressure control on cardiovascular, renal and mortality outcomes in people with type 2 diabetes: A systematic review and meta-analysis. Diabetes Metab Syndr. 2023;17:102782.
Blood Pressure Lowering Treatment Trialists’ Collaboration. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet. 2021;398:1053–64.
Nazarzadeh M, Bidel Z, Canoy D, Copland E, Bennett DA, Dehghan A, et al. Blood pressure-lowering treatment for prevention of major cardiovascular diseases in people with and without type 2 diabetes: an individual participant-level data meta-analysis. Lancet Diabetes Endocrinol. 2022;10:645–54.
Collard D, Brouwer TF, Peters RJG, Vogt L, van den Born BH. Creatinine rise during blood pressure therapy and the risk of adverse clinical outcomes in patients with type 2 diabetes mellitus. Hypertension. 2018;72:1337–44.
Tawfik YMK, Van Tassell BW, Dixon DL, Baker WL, Fanikos J, Buckley LF. Effects of Intensive Systolic Blood Pressure Lowering on End-Stage Kidney Disease and Kidney Function Decline in Adults With Type 2 Diabetes Mellitus and Cardiovascular Risk Factors: A Post Hoc Analysis of ACCORD-BP and SPRINT. Diabetes Care. 2023;46:868–73.
Bangalore S, Messerli FH, Wun CC, Zuckerman AL, DeMicco D, Kostis JB, et al. J-curve revisited: An analysis of blood pressure and cardiovascular events in the Treating to New Targets (TNT) Trial. Eur Heart J. 2010;31:2897–908.
Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, et al. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016;388:2142–52.
Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017;389:2226–37.
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Reboldi G. Aggressive blood pressure lowering is dangerous: the J-curve: con side of the arguement. Hypertension. 2014;63:37–40.
Kalkman DN, Brouwer TF, Vehmeijer JT, Berger WR, Knops RE, de Winter RJ, et al. J curve in patients randomly assigned to different systolic blood pressure targets: an experimental approach to an observational paradigm. Circulation. 2017;136:2220–9.
Kai H, Ueno T, Kimura T, Adachi H, Furukawa Y, Kita T, et al. Low DBP may not be an independent risk for cardiovascular death in revascularized coronary artery disease patients. J Hypertens. 2011;29:1889–96.
Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med. 2006;144:884–93.
Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, et al. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27:1360–9.
Mancia G, Grassi G. Aggressive blood pressure lowering is dangerous: the J-curve: pro side of the argument. Hypertension. 2014;63:29–36.
Beddhu S, Chertow GM, Greene T, Whelton PK, Ambrosius WT, Cheung AK, et al. Effects of intensive systolic blood pressure lowering on cardiovascular events and mortality in patients with type 2 diabetes mellitus on standard glycemic control and in those without diabetes mellitus: reconciling results From ACCORD BP and SPRINT. J Am Heart Assoc. 2018;7:e009326.
Vishram JK, Borglykke A, Andreasen AH, Jeppesen J, Ibsen H, Jørgensen T, et al. Impact of age on the importance of systolic and diastolic blood pressures for stroke risk: the Monica, Risk, Genetics, Archiving, and Monograph (MORGAM) Project. Hypertension. 2012;60:1117–23.
Schrier RW, Estacio RO, Mehler PS, Hiatt WR. Appropriate blood pressure control in hypertensive and normotensive type 2 diabetes mellitus: a summary of the ABCD trial. Nat Clin Pr Nephrol. 2007;3:428–38.
He J, Ouyang N, Guo X, Sun G, Li Z, Mu J, et al. Effectiveness of a non-physician community health-care provider-led intensive blood pressure intervention versus usual care on cardiovascular disease (CRHCP): an open-label, blinded-endpoint, cluster-randomised trial. Lancet. 2023;401:928–38.
Zanchetti A, Liu L, Mancia G, Parati G, Grassi G, Stramba-Badiale M, et al. Continuation of the ESH-CHL-SHOT trial after publication of the SPRINT: rationale for further study on blood pressure targets of antihypertensive treatment after stroke. J Hypertens. 2016;34:393–6.
Liao CT, Toh HS, Sun L, Yang CT, Hu A, Wei D, et al. Cost-effectiveness of intensive vs standard blood pressure control among older patients with hypertension. JAMA Netw Open. 2023;6:e230708.
Funding
This research was supported by Fukuoka University (GW2324).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abe, M., Segawa, H., Kinguchi, S. et al. Intensive blood pressure-lowering treatment to prevent cardiovascular events in patients with diabetes: a systematic review and meta-analysis. Hypertens Res 48, 2024–2033 (2025). https://doi.org/10.1038/s41440-025-02209-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02209-9
Keywords
This article is cited by
-
The conservative–challenging paradigm of antihypertensive therapy in JSH2025: a comparative perspective with contemporary Western guidelines
Hypertension Research (2026)
-
Advancing evidence-based blood pressure targets in JSH2025
Hypertension Research (2026)
-
The Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025)
Hypertension Research (2026)
-
Achievement rate of blood pressure control <130/80 mmHg as the core metric of implementation hypertension, based on the new JSH2025 and AHA/ACC2025 guidelines
Hypertension Research (2025)
-
Key highlights of the Japanese Society of Hypertension Guidelines for the management of elevated blood pressure and hypertension 2025 (JSH2025)
Hypertension Research (2025)