Abstract
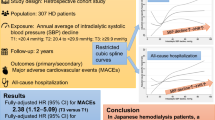
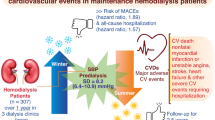
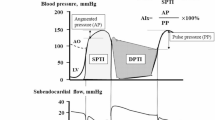
The prognostic utility of the combined assessment of pre-hemodialysis systolic blood pressure (SBP) and pulse rate compared to their independent assessment is unclear. In this nationwide cohort study, we aimed to determine whether their combined assessment could enhance the prognostic utility in patients on maintenance hemodialysis using the Japanese Renal Data Registry database. Exposure was defined as a combination of SBP and pulse rate. Forty-eight levels of exposure groups were created: SBP (<100, 100– < 120, 120– < 140, 140– < 160 [reference], 160– < 180, and ≥180 mmHg) and pulse rate (<50, 50– < 60, 60– < 70 [reference], 70– < 80, 80– < 90, 90– < 100, 100– < 110, and ≥110 beats/min). The primary and secondary outcomes were 1-year all-cause and cardiovascular mortalities, respectively. Multivariate Cox proportional hazards models were used, and multiplicative and additive interactions were assessed. The combined model for mortality and cardiac mortality was statistically better than the separate SBP and pulse rate model. Lower SBP was associated with higher risk of all-cause mortality irrespective of pulse rate. Most categories of lower SBP or higher pulse rate vs. the 120– < 140 mmHg and 70– < 80 beats/min category had positive relative excess risk due to interactions, with similar findings observed for cardiac mortality. Combined assessment of pre-dialysis SBP and pulse rate may help the simple stratification of patients with excess risks that cannot be identified by separate SBP and pulse rate assessment.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data will be available immediately after publication with no end dates. Data will be shared upon reasonable request to the corresponding author with permission from the JRDR investigators. Restrictions apply to the availability of the data analyzed in this study to preserve patient confidentiality.
References
Kurita N, Akizawa T, Fukuhara S. Vitality measured as self-reported energy level and clinical outcomes in hemodialysis patients: the Japanese Dialysis Outcomes and Practice Pattern Study (J-DOPPS). Am J Kidney Dis. 2019;73:486–95. https://doi.org/10.1053/j.ajkd.2018.10.001
Hannedouche T, Roth H, Krummel T, London GM, Jean G, Bouchet J-L, et al. Multiphasic effects of blood pressure on survival in hemodialysis patients. Kidney Int. 2016;90:674–84. https://doi.org/10.1016/j.kint.2016.05.025
Zager PG, Nikolic J, Brown RH, Campbell MA, Hunt WC, Peterson D, et al. U” curve association of blood pressure and mortality in hemodialysis patients. Med Dir Dial Clin Inc Kidney Int. 1998;54:561–9. https://doi.org/10.1046/j.1523-1755.1998.00005.x
Robinson BM, Tong L, Zhang J, Wolfe RA, Goodkin DA, Greenwood RN, et al. Blood pressure levels and mortality risk among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2012;82:570–80. https://doi.org/10.1038/ki.2012.136
Inoue T, Tokuyama K, Yoshi S, Nagayoshi N, Iseki C, Iseki K. Elevated resting heart rate is an independent predictor of all-cause death and cardiovascular events in Japanese ambulatory hemodialysis patients. Clin Exp Nephrol. 2012;16:938–44. https://doi.org/10.1007/s10157-012-0641-3
Iseki K, Nakai S, Yamagata K, Tsubakihara Y. Committee of Renal Data Registry of the Japanese Society for Dialysis Therapy. Tachycardia as a predictor of poor survival in chronic haemodialysis patients. Nephrol Dial Transpl. 2011;26:963–9. https://doi.org/10.1093/ndt/gfq507
Jiang X, Li X, Peng H, Li M, Wang C. Prognostic value of nighttime double product in nondialysis chronic kidney disease with hypertension. J Am Heart Assoc. 2023;12:e031627 https://doi.org/10.1161/JAHA.123.031627
Inoue R, Ohkubo T, Kikuya M, Metoki H, Asayama K, Kanno A, et al. Predictive value for mortality of the double product at rest obtained by home blood pressure measurement: the Ohasama study. Am J Hypertens. 2012;25:568–75. https://doi.org/10.1038/ajh.2012.3
Jiang Z-H, Aierken A, Wu T-T, Zheng Y-Y, Ma Y-T, Xie X. Rate pressure product as a novel predictor of long-term adverse outcomes in patients after percutaneous coronary intervention: a retrospective cohort study. BMJ Open. 2023;13:e067951 https://doi.org/10.1136/bmjopen-2022-067951
Stoschitzky K. Blood pressure, heart rate, or the Rate Pressure Product: what is the best predictor of clinical outcome? Eur Heart J Open. 2022;2:oeac063 https://doi.org/10.1093/ehjopen/oeac063
van Vliet BN, Montani JP. Baroreflex stabilization of the double product. Am J Physiol. 1999;277:H1679–89. https://doi.org/10.1152/ajpheart.1999.277.5.H1679
Huang B, Yang Y, Zhu J, Liang Y, Tan H, Yu L, et al. Usefulness of the admission shock index for predicting short-term outcomes in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2014;114:1315–21. https://doi.org/10.1016/j.amjcard.2014.07.062
El-Menyar A, Al Habib KF, Zubaid M, Alsheikh-Ali AA, Sulaiman K, Almahmeed W, et al. Utility of shock index in 24,636 patients presenting with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2020;9:546–56. https://doi.org/10.1177/2048872619886307
de Mutsert R, de Jager DJ, Jager KJ, Zoccali C, Dekker FW. Interaction on an additive scale. Nephron Clin Pr. 2011;119:c154–7. https://doi.org/10.1159/000327596
de Jager DJ, de Mutsert R, Jager KJ, Zoccali C, Dekker FW. Reporting of interaction. Nephron Clin Pr. 2011;119:c158–61. https://doi.org/10.1159/000327598
Nitta K, Goto S, Masakane I, Hanafusa N, Taniguchi M, Hasegawa T, et al. Annual dialysis data report for 2018, JSDT Renal Data Registry: Survey methods, facility data, incidence, prevalence, and mortality. Ren Replace Ther. 2020;6:41 https://doi.org/10.1186/s41100-020-00286-9
Nitta K. 2019 annual dialysis data report, JSDT renal data registry. Nihon Toseki Igakkai Zasshi. 2020;53:579–632. https://doi.org/10.4009/jsdt.53.579
Hanafusa N, Abe M, Joki N, Hoshino J, Kikuchi K, Goto S, et al. 2020 annual dialysis data report, JSDT renal data registry. J Jpn Soc Dial Ther. 2021;54:611–57. https://doi.org/10.4009/jsdt.54.611. In Japanese except for abstract
Murakami M, Fujii N, Kanda E, Kikuchi K, Wada A, Hamano T, et al. Association of four types of vascular access including arterial superficialization with mortality in maintenance hemodialysis patients: a nationwide cohort study in Japan. Am J Nephrol. 2023;54:83–94. https://doi.org/10.1159/000529991
Wakasugi M, Kazama JJ, Wada A, Hamano T, Masakane I, Narita I. Functional impairment attenuates the association between high serum phosphate and mortality in dialysis patients: a nationwide cohort study. Nephrol Dial Transpl. 2019;34:1207–16. https://doi.org/10.1093/ndt/gfy253
Textor J, Hardt J, Knüppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22:745 https://doi.org/10.1097/EDE.0b013e318225c2be
Etminan M, Collins GS, Mansournia MA. Using causal diagrams to improve the design and interpretation of medical research. Chest. 2020;158:S21–S28. https://doi.org/10.1016/j.chest.2020.03.011
Greenland S. Tests for interaction in epidemiologic studies: a review and a study of power. Stat Med. 1983;2:243–51. https://doi.org/10.1002/sim.4780020219
Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20:575–9. https://doi.org/10.1007/s10654-005-7835-x
Ohannessian R, Bénet T, Argaud L, Guérin C, Guichon C, Piriou V, et al. Heat map for data visualization in infection control epidemiology: An application describing the relationship between hospital-acquired infections, Simplified Acute Physiological Score II, and length of stay in adult intensive care units. Am J Infect Control. 2017;45:746–9. https://doi.org/10.1016/j.ajic.2017.02.012
Jann B. Color palettes for stata graphics. Stata J. 2018;18:765–85. https://doi.org/10.1177/1536867X1801800402
Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–98. https://doi.org/10.1002/sim.4780100410
Turner JM, Peixoto AJ. Blood pressure targets for hemodialysis patients. Kidney Int. 2017;92:816–23. https://doi.org/10.1016/j.kint.2017.01.038
Loutradis C, Sarafidis PA, Ferro CJ, Zoccali C. Volume overload in hemodialysis: diagnosis, cardiovascular consequences, and management. Nephrol Dial Transpl. 2021;36:2182–93. https://doi.org/10.1093/ndt/gfaa182
Port FK, Hulbert-Shearon TE, Wolfe RA, Bloembergen WE, Golper TA, Agodoa LY, et al. Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patients. Am J Kidney Dis. 1999;33:507–17. https://doi.org/10.1016/s0272-6386(99)70188-5
Palmer BF. Why are some dialysis patients chronically hypotensive in the absence of heart disease and volume depletion? Semin Dial. 2011;24:404–5. https://doi.org/10.1111/j.1525-139X.2011.00915.x
Bajpai D, Puttarajappa CM. Chronic hypotension and transplant outcomes-the known unknowns. Kidney Int Rep. 2024;9:1571–3. https://doi.org/10.1016/j.ekir.2024.04.065
Agarwal R, Sinha AD, Pappas MK, Abraham TN, Tegegne GG. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transpl. 2014;29:672–81. https://doi.org/10.1093/ndt/gft515
Hirakata H, Nitta K, Inaba M, Shoji T, Fujii H, Kobayashi S, et al. Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis: JSDT guidelines for CVD in HD patients. Ther Apher Dial. 2012;16:387–435. https://doi.org/10.1111/j.1744-9987.2012.01088.x
de Mutsert R, Grootendorst DC, Axelsson J, Boeschoten EW, Krediet RT, Dekker FW, et al. Excess mortality due to interaction between protein-energy wasting, inflammation and cardiovascular disease in chronic dialysis patients. Nephrol Dial Transpl. 2008;23:2957–64. https://doi.org/10.1093/ndt/gfn167
Davenport A. Why is intradialytic hypotension the commonest complication of outpatient dialysis treatments? Kidney Int Rep. 2023;8:405–18. https://doi.org/10.1016/j.ekir.2022.10.031
VanderWeele TJ. The interaction continuum. Epidemiology. 2019;30:648–58. https://doi.org/10.1097/EDE.0000000000001054
Woodward M, Webster R, Murakami Y, Barzi F, Lam T-H, Fang X, et al. The association between resting heart rate, cardiovascular disease and mortality: evidence from 112,680 men and women in 12 cohorts. Eur J Prev Cardiol. 2014;21:719–26. https://doi.org/10.1177/2047487312452501
Acknowledgements
We wish to acknowledge the efforts of the members of the Subcommittee for JRDR Regional Cooperation and staff members of the dialysis facilities who participated in the survey and responded to the questionnaires. This study utilized data from the JRDR. The interpretation and reporting of these data are solely the responsibility of the authors and do not reflect the official views or policies of the JSDT.
Author information
Authors and Affiliations
Contributions
Research idea and study design: NJ, NK; data acquisition: NJ, MA, NH; data analysis/interpretation: NJ, TT, K. Niihata, RI, K. Nakata; statistical analysis: TT, K. Niihata, NK; supervision or mentorship: MA, NH. Each author contributed important intellectual content during manuscript drafting or revision, agreed to be personally accountable for the individual’s own contributions, and ensured that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, were appropriately investigated and resolved, including documentation in the literature, if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
TT received consulting fees from Astellas Pharma Inc., as well as payments and educational events from Torii Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Kyowa Kirin Co., Ltd., AstraZeneca K.K., and Nobelpharma Co., Ltd. RI received payment for speaking from Astellas Pharma, Inc., Novartis Pharma K.K., and Otsuka Pharmaceutical. MA received payment for speaking from Novartis Pharma K.K. and Otsuka Pharmaceutical. NK received consulting fees from GlaxoSmithKline K.K. and payments for speaking and educational events from Eisai Co., Ltd., Taisho Pharmaceutical Co., Ltd., Kyowa Kirin Co., Ltd., GlaxoSmithKline K.K., Takeda Pharmaceutical Co., Ltd., Kissei Pharmaceutical Co., Ltd., and Baxter Corporation.
Consent
The requirement for written informed consent was waived owing to the retrospective nature of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joki, N., Toida, T., Niihata, K. et al. Combined pre-dialysis systolic blood pressure and pulse rate assessment for 1-year all-cause and cardiovascular mortality in patients on hemodialysis: a nationwide cohort study. Hypertens Res 48, 2045–2057 (2025). https://doi.org/10.1038/s41440-025-02231-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02231-x
Keywords
This article is cited by
-
Combined blood pressure and pulse rate as a new risk marker for mortality in hemodialysis patients
Hypertension Research (2025)