Abstract
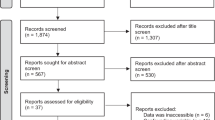
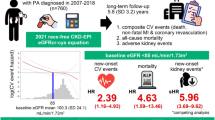
Many studies have investigated optimal blood pressure (BP) targets in patients with chronic kidney disease (CKD); however, no consensus has been reached. We therefore conducted a systematic review and meta-analysis, including the latest randomized controlled trials (RCTs). We searched MEDLINE, the Cochrane Library, and Ichushi Web for publications up to 13 June 2024, supplemented by hand searches. We included RCTs comparing the benefits and risks of more intensive (target BP: <130/80 mmHg) versus less intensive BP control (target BP: 130–149/80–89 mmHg or usual care) in patients with CKD aged ≥18 years, regardless of diabetes status. Primary outcomes were all-cause mortality and cardiovascular events. Secondary outcomes included renal events, including 50% reduction in estimated glomerular filtration rate (eGFR)/GFR, and end-stage kidney disease (ESKD). We calculated the risk ratio (RR) and variance, and obtained summary estimates of the effects with 95% confidence intervals (CIs) using a random-effects model with inverse variance weighting. Our meta-analysis included nine RCTs. More intensive BP control tended to reduce all-cause mortality (RR = 0.81; 95% CI 0.65–1.00; p = 0.051) and cardiovascular events (RR = 0.89; 95% CI 0.77–1.03; p = 0.13), but the differences were not significant. More intensive BP control did not increase the risk of serious renal events, including 50% reduction in eGFR/GFR (RR = 0.95; 95% CI 0.74–1.22; p = 0.69) or progression to ESKD (RR = 0.92; 95% CI 0.75–1.14; p = 0.45). These findings suggest that intensive BP control targeting <130/80 mmHg may reduce the risk of all-cause mortality and cardiovascular events in patients with CKD, without increasing the risk of serious renal events.

This meta-analysis of nine RCTs in patients with CKD found that more intensive BP control tended to reduce all-cause mortality and CVD events compared with less intensive control, without increasing serious kidney events, including 50% eGFR/GFR reduction, or ESKD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, et al. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:26072.
Burnier M, Damianaki A. Hypertension as cardiovascular risk factor in chronic kidney disease. Circ Res. 2023;132:1050–63.
Peralta CA, Norris KC, Li S, Chang TI, Tamura MK, Jolly SE, et al. KEEP Investigators. Blood pressure components and end-stage renal disease in persons with chronic kidney disease: the Kidney Early Evaluation Program (KEEP). Arch Intern Med. 2012;172:41–7.
Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, et al. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med. 1994;330:877–84.
Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288:2421–31.
Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M, et al. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365:939–46.
ACCORD Study Group, Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85.
SPS3 Study Group, Benavente OR, Coffey CS, Conwit R, Hart RG, McClure LA, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15.
SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Blood Pressure Lowering Treatment Trialists’ Collaboration, Ninomiya T, Perkovic V, Turnbull F, Neal B, Barzi F, et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ. 2013;347:5680.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43.
Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more Intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:1498–505.
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021;99:S1–S87.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Japanese Society of Nephrology. Essential points from evidence-based clinical practice guideline for chronic kidney disease 2023. Clin Exp Nephrol. 2024;28:473–95.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. 2017
Tsai WC, Wu HY, Peng YS, Yang JY, Chen HY, Chiu YL, et al. Association of intensive blood pressure control and kidney disease progression in nondiabetic patients with chronic kidney disease: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:792–9.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
He J, Ouyang N, Guo X, Sun G, Li Z, Mu J, et al. Effectiveness of a non-physician community health-care provider-led intensive blood pressure intervention versus usual care on cardiovascular disease (CRHCP): an open-label, blinded-endpoint, cluster-randomised trial. Lancet. 2023;401:928–38.
Liu J, Li Y, Ge J, Yan X, Zhang H, Zheng X, et al. Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial. Lancet. 2024;404:245–55.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sakima A, Satonaka H, Nishida N, Yatsu K, Arima H. Optimal blood pressure targets for patients with hypertension: a systematic review and meta-analysis. Hypertens Res. 2019;42:483–95.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105:S117–S314.
Schrier RW, Abebe KZ, Perrone RD, Torres VE, Braun WE, Steinman TI, et al. Blood pressure in early autosomal dominant polycystic kidney disease. N Engl J Med. 2014;371:2255–66.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [RoB2]
Tawfik YMK, Van Tassell BW, Dixon DL, Baker WL, Fanikos J, Buckley LF. Effects of intensive systolic blood pressure lowering on end-stage kidney Disease and kidney function decline in adults with type 2 diabetes mellitus and cardiovascular risk factors: a post hoc analysis of ACCORD-BP and SPRINT. Diabetes Care. 2023;46:868–73.
Higgins J, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions, version 6.5. The Cochrane Collaboration, 2024. http://handbook.cochrane.org. Accessed 10 September 10 2024.
Cheung AK, Rahman M, Reboussin DM, Craven TE, Greene T, Kimmel PL, et al. SPRINT Research Group. Effects of intensive BP control in CKD. J Am Soc Nephrol. 2017;28:2812–23.
Agarwal A, Cheung AK, Ma J, Cho M, Li M. Effect of baseline kidney function on the risk of recurrent stroke and on effects of intensive blood pressure control in patients with previous lacunar stroke: a post hoc analysis of the SPS3 Trial (Secondary Prevention of Small Subcortical Strokes). J Am Heart Assoc. 2019;8:e013098.
Bi Y, Li M, Liu Y, Li T, Lu J, Duan P, et al. BPROAD Research Group. Intensive blood-pressure control in patients with type 2 diabetes. N Engl J Med. 2024. https://doi.org/10.1056/NEJMoa2412006.
Sarnak MJ, Greene T, Wang X, Beck G, Kusek JW, Collins AJ, et al. The effect of a lower target blood pressure on the progression of kidney disease: long-term follow-up of the modification of diet in renal disease study. Ann Intern Med. 2005;142:342–51.
Appel LJ, Wright JT Jr, Greene T, Agodoa LY, Astor BC, Bakris GL, et al. AASK Collaborative Research Group. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010;363:918–29.
Lv J, Ehteshami P, Sarnak MJ, Tighiouart H, Jun M, Ninomiya T, et al. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ. 2013;185:949–57.
Acknowledgements
The authors would like to thank Fukuoka University Medical Library. We also thank Susan Furness, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tada, K., Fujiwara, A., Sugano, N. et al. Evaluating blood pressure targets in chronic kidney disease: a systematic review and meta-analysis. Hypertens Res 48, 2358–2367 (2025). https://doi.org/10.1038/s41440-025-02262-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-025-02262-4
Keywords
This article is cited by
-
Impact of office and home blood pressure control on cardiovascular events in relation to KDIGO risk categories: findings from the J-HOP study
Hypertension Research (2026)
-
Advancing evidence-based blood pressure targets in JSH2025
Hypertension Research (2026)
-
Blood pressure control in patients with chronic kidney disease: comparison between JSH2025 and other international guidelines
Hypertension Research (2026)
-
The conservative–challenging paradigm of antihypertensive therapy in JSH2025: a comparative perspective with contemporary Western guidelines
Hypertension Research (2026)
-
Achievement rate of blood pressure control <130/80 mmHg as the core metric of implementation hypertension, based on the new JSH2025 and AHA/ACC2025 guidelines
Hypertension Research (2025)