Abstract
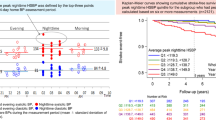
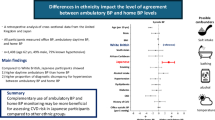
Ambulatory blood pressure monitoring (ABPM) studies for high altitude (HA) hypertensive patients are limited. We aimed to explore the hypertension phenotypes, and investigate their associations with hemoglobin in untreated hypertensives permanently living in HA. A total of 342 untreated hypertensive patients were included. Among the whole population, 91.80% had sustained hypertension (SH). In patients with SH, the proportions of isolated daytime hypertension, isolated nocturnal hypertension, and day-night hypertension were 2.87%, 2.87%, and 94.26%, respectively. Compared to patients with hemoglobin ≥16 g/dL, those with hemoglobin <16 g/dL had higher nocturnal average systolic blood pressure (SBP) (140.33 ± 17.46 vs. 136.26 ± 17.55 mmHg, P = 0.03) and a greater proportion of patients with nocturnal SBP fall<10% (55.00% vs. 43.30%, P = 0.03). Bivariate correlation analysis showed that hemoglobin was negatively correlated with the nocturnal average SBP (r = −0.145, P < 0.01) and was positively related to the nocturnal SBP fall (r = 0.136, P = 0.01). We found that the threshold effect value between hemoglobin and nocturnal blood pressure indices was 16 g/dL. The effect value between hemoglobin and nocturnal average SBP was −3.60 (−5.46, −1.74) for hemoglobin <16 g/dL and 0.88 (−1.07, 2.83) for hemoglobin ≥16 g/dL. Correspondingly, the effect values between hemoglobin and nocturnal SBP fall were 1.53 (0.61, 2.45) and −0.26 (−1.23, 0.70). In addition, hemoglobin was independently correlated with the above-mentioned nocturnal blood pressure indices in those with hemoglobin <16 g/dL. In conclusion, nocturnal hypertension was a prevalent ABPM phenotype in HA hypertensive patients. In those with hemoglobin levels <16 g/dL, hemoglobin concentration shows a significant inverse correlation with nocturnal SBP, suggesting that lower hemoglobin levels may warrant enhanced evaluation of nocturnal BP in this population.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Mallet RT, Burtscher J, Richalet JP, Millet GP, Burtscher M. Impact of High Altitude on Cardiovascular Health: Current Perspectives. Vasc Health Risk Manag. 2021;17:317–35.
Tremblay JC, Ainslie PN. Global and country-level estimates of human population at high altitude. Proc Natl Acad Sci USA. 2021;118:e2102463118.
Narvaez-Guerra O, Herrera-Enriquez K, Medina-Lezama J, Chirinos JA. Systemic Hypertension at High Altitude. Hypertension. 2018;72:567–78.
Beall CM. Two routes to functional adaptation: Tibetan and Andean high-altitude natives. Proc Natl Acad Sci USA. 2007;104:8655–60.
Parati G, Agostoni P, Basnyat B, Bilo G, Brugger H, Coca A, et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: A joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur Heart J. 2018;39:1546–54.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Zhao X, Li S, Ba S, He F, Li N, Ke L, et al. Prevalence, awareness, treatment, and control of hypertension among herdsmen living at 4,300 m in Tibet. Am J Hypertens. 2012;25:583–9.
Zhang X, Zhang Z, Ye R, Meng Q, Chen X. Prevalence of hypertension and its relationship with altitude in highland areas: a systematic review and meta-analysis. Hypertens Res. 2022;45:1225–39.
Mehata S, Shrestha N, Ghimire S, Atkins E, Karki DK, Mishra SR. Association of altitude and urbanization with hypertension and obesity: analysis of the Nepal Demographic and Health Survey 2016. Int Health. 2021;13:151–60.
Siebenmann C, Roche J, Schlittler M, Simpson LL, Stembridge M. Regulation of haemoglobin concentration at high altitude. J Physiol. 2024;602:5587–600.
Liu X, Yang C, Zhang X, Ye R, Li X, Zhang Z, et al. Association between hemoglobin concentration and hypertension risk in native Tibetans at high altitude. J Clin Hypertens (Greenwich). 2024;26:17–23.
Parati G, Bilo G, Faini A, Bilo B, Revera M, Giuliano A, et al. Changes in 24 h ambulatory blood pressure and effects of angiotensin II receptor blockade during acute and prolonged high-altitude exposure: a randomized clinical trial. Eur Heart J. 2014;35:3113–22.
Bilo G, Villafuerte FC, Faini A, Anza-Ramirez C, Revera M, Giuliano A, et al. Ambulatory blood pressure in untreated and treated hypertensive patients at high altitude: the High Altitude Cardiovascular Research-Andes study. Hypertension. 2015;65:1266–72.
Zheng X, Yao DK, Zhuo-Ma CR, Tang J, Wang TR, Zhang HH, et al. Prevalence, self-awareness, treatment, and control of hypertension in Lhasa, Tibet. Clin Exp Hypertens. 2012;34:328–33.
Norboo T, Stobdan T, Tsering N, Angchuk N, Tsering P, Ahmed I, et al. Prevalence of hypertension at high altitude: cross-sectional survey in Ladakh, Northern India 2007-2011. BMJ Open. 2015;5:e007026.
Medina-Lezama J, Herrera-Enriquez K, Narvaez-Guerra O, Chirinos JA. Influence of altitude on hypertension phenotypes and responses to antihypertensive therapy: Review of the literature and design of the INTERVENCION trial. J Clin Hypertens (Greenwich). 2020;22:1757–62.
Bilo G, Acone L, Anza-Ramirez C, Macarlupu JL, Soranna D, Zambon A, et al. Office and Ambulatory Arterial Hypertension in Highlanders: HIGHCARE-ANDES Highlanders Study. Hypertension. 2020;76:1962–70.
Kario K, Hoshide S, Chia YC, Buranakitjaroen P, Siddique S, Shin J, et al. Guidance on ambulatory blood pressure monitoring: A statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2021;23:411–21.
Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–302.
Multidisciplinary Expert Task Force on H, Related D. Chinese Multidisciplinary Expert Consensus on the Diagnosis and Treatment of Hyperuricemia and Related Diseases. Chin Med J (Engl). 2017;130:2473–88.
American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81–90.
Filippone EJ, Foy AJ, Naccarelli GV. Controversies in Hypertension III: Dipping, Nocturnal Hypertension, and the Morning Surge. Am J Med. 2023;136:629–37.
Huang QF, Yang WY, Asayama K, Zhang ZY, Thijs L, Li Y, et al. Ambulatory Blood Pressure Monitoring to Diagnose and Manage Hypertension. Hypertension. 2021;77:254–64.
Joint Committee for Guideline R. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16:182–241.
Huang J, Wildman RP, Gu D, Muntner P, Su S, He J. Prevalence of isolated systolic and isolated diastolic hypertension subtypes in China. Am J Hypertens. 2004;17:955–62.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55–61.
Yang WY, Melgarejo JD, Thijs L, Zhang ZY, Boggia J, Wei FF, et al. Association of Office and Ambulatory Blood Pressure With Mortality and Cardiovascular Outcomes. JAMA. 2019;322:409–20.
Tadic M, Cuspidi C, Grassi G, Mancia G. Isolated Nocturnal Hypertension: What Do We Know and What Can We Do?. Integr Blood Press Control. 2020;13:63–9.
Androulakis E, Papageorgiou N, Chatzistamatiou E, Kallikazaros I, Stefanadis C, Tousoulis D. Improving the detection of preclinical organ damage in newly diagnosed hypertension: nocturnal hypertension versus non-dipping pattern. J Hum Hypertens. 2015;29:689–95.
Ogedegbe G, Spruill TM, Sarpong DF, Agyemang C, Chaplin W, Pastva A, et al. Correlates of isolated nocturnal hypertension and target organ damage in a population-based cohort of African Americans: the Jackson Heart Study. Am J Hypertens. 2013;26:1011–6.
Torlasco C, Bilo G, Giuliano A, Soranna D, Ravaro S, Oliverio G, et al. Effects of acute exposure to moderate altitude on blood pressure and sleep breathing patterns. Int J Cardiol. 2020;301:173–9.
Phelan B, Mather L, Regmi N, Starling J, Twillmann D, McElwee M, et al. Ambulatory Blood Pressure at Sea Level and High Altitude in a Climber with a Kidney Transplant and Hypertension. High Alt Med Biol. 2019;20:307–11.
Zhou E, Lei R, Tian X, Liu C, Guo J, Jin L, et al. Association between salt sensitivity of blood pressure and the risk of hypertension in a Chinese Tibetan population. J Clin Hypertens (Greenwich). 2023;25:453–62.
Zhao X, Yin X, Li X, Yan LL, Lam CT, Li S, et al. Using a low-sodium, high-potassium salt substitute to reduce blood pressure among Tibetans with high blood pressure: a patient-blinded randomized controlled trial. PLoS One. 2014;9:e110131.
Bazmandegan G, Abbasifard M, Ostadebrahimi H, Gholamrezapour M, Kamiab Z. Positive Association between Hemoglobin Concentration and Blood Pressure in Adults: A Cross-Sectional Study Based on Rafsanjan Cohort Study. Int J Hypertens. 2023;2023:6283711.
Atsma F, Veldhuizen I, de Kort W, van Kraaij M, Pasker-de Jong P, Deinum J. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension. 2012;60:936–41.
Lee SG, Rim JH, Kim JH. Association of hemoglobin levels with blood pressure and hypertension in a large population-based study: the Korea National Health and Nutrition Examination Surveys 2008-2011. Clin Chim Acta. 2015;438:12–8.
Akdi A, Ozeke O, Karanfil M, Ertem AG, Yayla C, Demirtas K, et al. Diurnal rhythm of blood pressure in patients with polycythemia vera. Blood Press Monit. 2020;25:69–74.
Marketou M, Patrianakos A, Parthenakis F, Zacharis E, Arfanakis D, Kochiadakis G, et al. Systemic blood pressure profile in hypertensive patients with low hemoglobin concentrations. Int J Cardiol. 2010;142:95–6.
Schwartz NG, Rattner A, Schwartz AR, Mokhlesi B, Gilman RH, Bernabe-Ortiz A, et al. Group CCS: Sleep Disordered Breathing in Four Resource-Limited Settings in Peru: Prevalence, Risk Factors, and Association with Chronic Diseases. Sleep. 2015;38:1451–9.
Pham LV, Meinzen C, Arias RS, Schwartz NG, Rattner A, Miele CH, et al. Cross-Sectional Comparison of Sleep-Disordered Breathing in Native Peruvian Highlanders and Lowlanders. High Alt Med Biol. 2017;18:11–9.
Yang C, Liu H, Li Q, Wang X, Ma W, Liu C, et al. Human expansion into Asian highlands in the 21st Century and its effects. Nat Commun. 2022;13:4955.
Peng W, Li K, Yan AF, Shi Z, Zhang J, Cheskin LJ, et al. Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. Int J Environ Res Public Health. 2022;19:8787.
Shen Y, Chang C, Zhang J, Jiang Y, Ni B, Wang Y. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: a cross-sectional study. Environ Health Prev Med. 2017;22:19.
Liu J, Li Y, Zhang X, Bu P, Du X, Fang L, et al. Management of nocturnal hypertension: An expert consensus document from Chinese Hypertension League. J Clin Hypertens (Greenwich). 2024;26:71–83.
Liu J, Li Y, Asayama K, Zhang XJ, Cheng HM, Park S, et al. Asian Expert Consensus on Nocturnal Hypertension Management. Hypertension. 2025;82:945–56.
Acknowledgements
The authors sincerely thank the doctors, nurses, and medical laboratory staffs from the Jiulong, Luhuo, and Litang County People’s hospitals for their kind help in data collection. Second, we thank all participants who were enrolled in this investigation.
Funding
This manuscript was funded by the Science and Technology Program of Tibet Autonomous Region (Grant number: XZ202303ZY0004G) and the Sichuan Natural Science Foundation project (Grant number: 2022NSFSC0801 and 2023NSFSC1632).
Author information
Authors and Affiliations
Contributions
Study design: Xin Zhang, Xiaoping Chen. Data collection: Runyu Ye, Xiangyu Yang, Xinran Li, Zhipeng Zhang. Analysis and interpretation of data: Xin Zhang, Runyu Ye, Xiangyu Yang. Drafting of the manuscript: Xin Zhang, Xiangyu Yang. Correction: Qingtao Meng, Xiaoping Chen. Approval of the final version for publication: all the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
The research protocol was reviewed by the Medical Ethics Committee of West China Hospital, Sichuan University. All procedures performed in studies involving human participants were in accordance with the ethical guidelines of the Declaration of Helsinki. Informed written consent was obtained from patients before enrollment.
Consent for publication
All coauthors have given their consent for publication of this article in Hypertension Research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Ye, R., Yang, X. et al. Study on the ambulatory blood pressure phenotype and its correlation with hemoglobin concentration in untreated hypertensive individuals permanently living in plateau areas. Hypertens Res (2025). https://doi.org/10.1038/s41440-025-02350-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41440-025-02350-5