Abstract
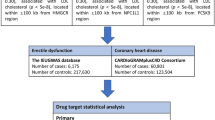
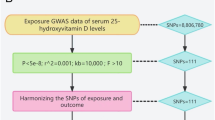
Erectile dysfunction is a common sexual disorder in men. Some studies have found a strong association between some serum metabolites and erectile dysfunction. To investigate this association further, we used bidirectional Mendelian randomisation to investigate causality and possible biological mechanisms.Firstly, this study screened the statistics of genome-wide association studies of serum metabolites and erectile dysfunction to obtain instrumental variables. Inverse variance weighting was used as the primary method for causal effect analysis of instrumental variables in forward or reverse Mendelian randomisation, and the results obtained by MR-Egger regression and the weighted median method were used as references. Subsequently, the metabolites causally associated with erectile dysfunction were subjected to replication analyses and meta-analyses, and the results of the meta-analyses were analysed by pathway analyses to find influential pathways. In this process, Mendelian randomisation results need to be assessed for stability and reliability using sensitivity analysis.It was found that a total of six serum metabolites were causally associated with erectile dysfunction in a forward Mendelian randomisation study. 1,3,7-trimethyluraten (0.85 (0.73–0.99), P = 0.0368), ergothioneine (0.65 (0.45–0.94), P = 0.0226) and gamma-glutamylglutamate (0.63 (0.46–0.88), P = 0.0059) were protective against the development of erectile dysfunction, whereas 2-hydroxyhippurate (1.10 (1.02–1.19), P = 0.0152), N2,N2-dimethylguanosine (1.57 (1.02–2.40), P = 0.0395) and octanoylcarnitine (1.38 (1.06–1.82), P = 0.0183) were able to induce the development of erectile dysfunction. In addition, metabolic pathway analysis showed that 1,3,7-trimethylurate was able to influence the development of erectile dysfunction via the caffeine metabolism pathway (P = 0.0454). On the other hand, reverse Mendelian randomisation analysis showed that erectile dysfunction reduced serum homocitrulline levels (0.99 (0.97–1.00), P = 0.0360). Sensitivity analyses, including heterogeneity tests and pleiotropy tests, confirmed the reliability of the results.In conclusion, this study demonstrated a bidirectional causal relationship between serum metabolites and erectile dysfunction using bidirectional Mendelian randomisation analysis and replication meta-analysis. On this basis, this study provides a new direction of thinking and strong evidence for the therapeutic application and adjunctive diagnosis of serum metabolites in erectile dysfunction, and provides a certain reference value for subsequent related studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article.
References
NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90.
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
Corona G, Lee DM, Forti G, O’Connor DB, Maggi M, O’Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS). J Sex Med. 2010;7:1362–80.
Yafi FA, Jenkins L, Albersen M, Corona G, Isidori AM, Goldfarb S, et al. Erectile dysfunction. Nat Rev Dis Primers. 2016;2:16003.
Hatzimouratidis K, Salonia A, Adaikan G, Buvat J, Carrier S, El-Meliegy A, et al. Pharmacotherapy for Erectile Dysfunction: Recommendations From the Fourth International Consultation for Sexual Medicine (ICSM 2015). J Sex Med. 2016;13:465–88.
Corona G, Rastrelli G, Burri A, Jannini EA, Maggi M. The safety and efficacy of Avanafil, a new 2(nd) generation PDE5i: comprehensive review and meta-analysis. Expert Opin Drug Saf. 2016;15:237–47.
Goldsmith P, Fenton H, Morris-Stiff G, Ahmad N, Fisher J, Prasad KR. Metabonomics: a useful tool for the future surgeon. J Surg Res. 2010;160:122–32.
Lopez DS, Advani S, Tsilidis KK, Wang R, Baillargeon J, Dobs A, et al. Association of Urinary Phthalate Metabolites With Erectile Dysfunction in Racial and Ethnic Groups in the National Health and Nutrition Examination Survey 2001-2004. Am J Mens Health. 2017;11:576–84.
Katsimardou A, Patoulias D, Zografou I, Siskos F, Stavropoulos K, Imprialos K, et al. The Impact of Metabolic Syndrome Components on Erectile Function in Patients with Type 2 Diabetes. Metabolites. 2023;13:617.
Rocca MS, Vignoli A, Tenori L, Ghezzi M, De Rocco Ponce M, Vatsellas G, et al. Evaluation of Serum/Urine Genomic and Metabolomic Profiles to Improve the Adherence to Sildenafil Therapy in Patients with Erectile Dysfunction. Front Pharmacol. 2020;11:602369.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27:1133–63.
Bowden J, Holmes MV. Meta-analysis and Mendelian randomization: A review. Res Synth Methods. 2019;10:486–96.
Wichmann HE, Gieger C, Illig T. KORA-gen-resource for population genetics, controls and a broad spectrum of disease phenotypes. Gesundheitswesen. 2005;67:S26–30. Suppl 1
Moayyeri A, Hammond CJ, Hart DJ, Spector TD. The UK Adult Twin Registry (TwinsUK Resource). Twin Res Hum Genet. 2013;16:144–9.
Shin SY, Fauman EB, Petersen AK, Krumsiek J, Santos R, Huang J, et al. An atlas of genetic influences on human blood metabolites. Nat Genet. 2014;46:543–50.
Kanehisa M, Goto S, Sato Y, Furumichi M, Tanabe M. KEGG for integration and interpretation of large-scale molecular data sets. Nucleic Acids Res. 2012;40:D109–14.
Bovijn J, Jackson L, Censin J, Chen CY, Laisk T, Laber S, et al. GWAS Identifies Risk Locus for Erectile Dysfunction and Implicates Hypothalamic Neurobiology and Diabetes in Etiology. Am J Hum Genet. 2019;104:157–63.
Burgess S, Thompson SG. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40:755–64.
Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol. 2011;40:740–52.
Emdin CA, Khera AV, Kathiresan S. Mendelian Randomization. JAMA. 2017;318:1925–6.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016;40:304–14.
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89.
Cohen JF, Chalumeau M, Cohen R, Korevaar DA, Khoshnood B, Bossuyt PM. Cochran’s Q test was useful to assess heterogeneity in likelihood ratios in studies of diagnostic accuracy. J Clin Epidemiol. 2015;68:299–306.
Greco MF, Minelli C, Sheehan NA, Thompson JR. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med. 2015;34:2926–40.
Wan B, Ma N, Lu W. Mendelian randomization investigation identified the causal relationship between body fat indexes and the risk of bladder cancer. PeerJ. 2023;11:e14739.
Hemani G, Bowden J, Davey Smith G. Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum Mol Genet. 2018;27:R195–r208.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193–206.
Viechtbauer W. Hypothesis tests for population heterogeneity in meta-analysis. Br J Math Stat Psychol. 2007;60:29–60.
Jewison T, Su Y, Disfany FM, Liang Y, Knox C, Maciejewski A, et al. SMPDB 2.0: big improvements to the Small Molecule Pathway Database. Nucleic Acids Res. 2014;42:D478–84. Database issue
Kot M, Daniel WA. Caffeine as a marker substrate for testing cytochrome P450 activity in human and rat. Pharmacol Rep. 2008;60:789–97.
Daniel WA, Kot M, Wójcikowski J. Effects of classic and newer antidepressants on the oxidation pathways of caffeine in rat liver. In vitro study. Pol J Pharmacol. 2003;55:1045–53.
Lopez DS, Wang R, Tsilidis KK, Zhu H, Daniel CR, Sinha A, et al. Role of Caffeine Intake on Erectile Dysfunction in US Men: Results from NHANES 2001-2004. PLoS One. 2014;10:e0123547.
Allen MS, Walter EE. Health-Related Lifestyle Factors and Sexual Dysfunction: A Meta-Analysis of Population-Based Research. J Sex Med. 2018;15:458–75.
Yang R, Wang J, Chen Y, Sun Z, Wang R, Dai Y. Effect of caffeine on erectile function via up-regulating cavernous cyclic guanosine monophosphate in diabetic rats. J Androl. 2008;29:586–91.
Gołembiowska K, Dziubina A, Kowalska M, Kamińska K. Paradoxical effects of adenosine receptor ligands on hydroxyl radical generation by L-DOPA in the rat striatum. Pharmacol Rep. 2008;60:319–30.
Lee C. Antioxidant ability of caffeine and its metabolites based on the study of oxygen radical absorbing capacity and inhibition of LDL peroxidation. Clin Chim Acta. 2000;295:141–54.
Salisbury D, Bronas U. Reactive oxygen and nitrogen species: impact on endothelial dysfunction. Nurs Res. 2015;64:53–66.
Zheng D, Liu J, Piao H, Zhu Z, Wei R, Liu K. ROS-triggered endothelial cell death mechanisms: Focus on pyroptosis, parthanatos, and ferroptosis. Front Immunol. 2022;13:1039241.
Terentes-Printzios D, Ioakeimidis N, Rokkas K, Vlachopoulos C. Interactions between erectile dysfunction, cardiovascular disease and cardiovascular drugs. Nat Rev Cardiol. 2022;19:59–74.
Burnett AL. Nitric oxide in the penis-science and therapeutic implications from erectile dysfunction to priapism. J Sex Med. 2006;3:578–82.
Suzuki T, Yamamoto H, Pfleiderer W. Nitrosation of N-methyl derivatives of uric acid and their transnitrosation ability to N-acetylcysteine. Chem Pharm Bull. 2010;58:1271–5.
Gründemann D, Harlfinger S, Golz S, Geerts A, Lazar A, Berkels R, et al. Discovery of the ergothioneine transporter. Proc Natl Acad Sci USA. 2005;102:5256–61.
Cheah IK, Halliwell B. Ergothioneine; antioxidant potential, physiological function and role in disease. Biochim Biophys Acta. 2012;1822:784–93.
Paul BD, Snyder SH. The unusual amino acid L-ergothioneine is a physiologic cytoprotectant. Cell Death Differ. 2010;17:1134–40.
Borodina I, Kenny LC, McCarthy CM, Paramasivan K, Pretorius E, Roberts TJ, et al. The biology of ergothioneine, an antioxidant nutraceutical. Nutr Res Rev. 2020;33:190–217.
Paul BD. Ergothioneine: A Stress Vitamin with Antiaging, Vascular, and Neuroprotective Roles? Antioxid Redox Signal. 2022;36:1306–17.
Koh SS, Ooi SC, Lui NM, Qiong C, Ho LT, Cheah IK, et al. Effect of Ergothioneine on 7-Ketocholesterol-Induced Endothelial Injury. Neuromolecular Med. 2021;23:184–98.
Li RW, Yang C, Sit AS, Kwan YW, Lee SM, Hoi MP, et al. Uptake and protective effects of ergothioneine in human endothelial cells. J Pharmacol Exp Ther. 2014;350:691–700.
Liu Q, Zhang Y, Wang J, Li S, Cheng Y, Guo J, et al. Erectile Dysfunction and Depression: A Systematic Review and Meta-Analysis. J Sex Med. 2018;15:1073–82.
Nakamichi N, Nakayama K, Ishimoto T, Masuo Y, Wakayama T, Sekiguchi H, et al. Food-derived hydrophilic antioxidant ergothioneine is distributed to the brain and exerts antidepressant effect in mice. Brain Behav. 2016;6:e00477.
Matsuda Y, Ozawa N, Shinozaki T, Wakabayashi KI, Suzuki K, Kawano Y, et al. Ergothioneine, a metabolite of the gut bacterium Lactobacillus reuteri, protects against stress-induced sleep disturbances. Transl Psychiatry. 2020;10:170.
Vangipurapu J, Fernandes Silva L, Kuulasmaa T, Smith U, Laakso M. Microbiota-Related Metabolites and the Risk of Type 2 Diabetes. Diabetes Care. 2020;43:1319–25.
Hidalgo-Tamola J, Chitaley K. Review type 2 diabetes mellitus and erectile dysfunction. J Sex Med. 2009;6:916–26.
Pallan PS, Kreutz C, Bosio S, Micura R, Egli M. Effects of N2,N2-dimethylguanosine on RNA structure and stability: crystal structure of an RNA duplex with tandem m2 2G:A pairs. RNA. 2008;14:2125–35.
Tormey DC, Waalkes TP, Gehrke CW. Biological markers in breast carcinoma-clinical correlations with pseudouridine, N2,N2-dimethylguanosine, and 1-methylinosine. J Surg Oncol. 1980;14:267–73.
Woo KB, Waalkes TP, Ahmann DL, Tormey DC, Gehrke CW, Oliverio VT. A quantitative approach to determining disease response during therapy using multiple biologic markers: application to carcinoma of the breast. Cancer. 1978;41:1685–703.
Ottosson F, Smith E, Gallo W, Fernandez C, Melander O. Purine Metabolites and Carnitine Biosynthesis Intermediates Are Biomarkers for Incident Type 2 Diabetes. J Clin Endocrinol Metab. 2019;104:4921–30.
Acknowledgements
We thank all the participants and investigators of the IEU consortium, FinnGen consortium and Metabolomics GWAS.
Funding
This work was supported the Young/Middle aged Talent Cultivation Project that was funded by the Fujian Provincial Health and Family Planning Commission and Xiamen Health and Family Planning Commission (No. 2021GGB028).
Author information
Authors and Affiliations
Contributions
RX and XW designed the study, contributed to the data analysis, and wrote the manuscript. SL, LL and YB contributed to the data analysis and data interpretation. PB and GL contributed to manuscript writing and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, R., Liu, S., Li, Ly. et al. Exploring the causal association between serum metabolites and erectile dysfunction: a bidirectional Mendelian randomisation study. Int J Impot Res 37, 601–611 (2025). https://doi.org/10.1038/s41443-024-00926-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41443-024-00926-2