Abstract
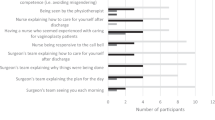
This retrospective study examines 58 transgender women who presented with cosmetic concerns following gender-affirming vaginoplasty between January 2020 and April 2023. The cohort’s mean age was 36.8 years (±9.8), with a mean BMI of 29.5 kg/m² (±7.1). Most patients were Black or African American (41.4%) or White (31.4%), and 43.0% had wound healing comorbidities. Of the total cohort, 62.1% (36/58) underwent penile inversion vaginoplasty (PIV), 31.0% (18/58) robotic-assisted vaginoplasty with peritoneal flaps, and 6.9% (4/58) shallow-depth vaginoplasty. A total of 36.2% (21/58) patients reported cosmetic concerns, most frequently labial (20.7%), clitoral (12.1%), hypergranulation tissue (8.6%), mons pubis fullness (5.2%), and introital scarring (5.2%). Management included expectant care, in-office procedures (e.g., silver nitrate for hypergranulation), and surgical revision. Surgical revision was performed in 80.9% of patients, with all reporting post-operative cosmetic satisfaction. A guide to surgical revision is discussed for each cosmetic concern subgroup. A tiered approach involving expectant management, in-office interventions, and surgical revision can effectively address these issues and enhance patient satisfaction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Our data will be made available upon request.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed., text rev. Arlington (VA): American Psychiatric Publishing; 2022.
Budge SL, Adelson JL, Howard KAS. Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J Consult Clin Psychol. 2013;81:545–57.
De Vries ALC, McGuire JK, Steensma TD, Wagenaar ECF, Doreleijers TAH, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. 2014;134:696–704.
De Cuypere G, TSjoen G, Beerten R, Selvaggi G, De Sutter P, Hoebeke P, et al. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005;34:679–90.
Green R. Sexual functioning in post-operative transsexuals: male-to-female and female-to-male. Int J Impot Res. 1998;10 Suppl 1:S22–24.
Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. 2018;199:760–5.
Maurer V, Howaldt M, Feldmann I, Ludwig T, Vetterlein MW, Gild P, et al. Penile flap inversion vaginoplasty in transgender women: contemporary morbidity and learning-curve analysis from a high-volume reconstructive center. Front Surg. 2022;9:836335.
Falcone M, Timpano M, Ceruti C, Sedigh O, Oderda M, Gillo A, et al. A single-center analysis on the learning curve of male-to-female penoscrotal vaginoplasty by multiple surgical measures. Urology. 2017;99:234–9.
Dy GW, Jun MS, Blasdel G, Bluebond-Langner R, Zhao LC. Outcomes of gender affirming peritoneal flap vaginoplasty using the Da Vinci single port versus Xi robotic systems. Eur Urol. 2021;79:676–83.
Kocjancic E, Vigneswaran H, Sofer L, Jaunarena J, Whitehead D, Morgantini L, et al. V10-01 novel vaginoplasty technique: inversion of penile skin and use of scrotal graft without sacrospinal fixation. J Urol [Internet]. 2018 Apr [cited 2025 Jan 9];199. Available from: http://www.jurology.com/doi/10.1016/j.juro.2018.02.2657.
Acar O, Sofer L, Dobbs RW, Greenwald DT, Halgrimson WR, Crivellaro S, et al. Single port and multiport approaches for robotic vaginoplasty with the davydov technique. Urology. 2020;138:166–73.
Mañero I, Arno AI, Herrero R, Labanca T. Cosmetic revision surgeries after transfeminine vaginoplasty. Aesthetic Plast Surg. 2023;47:430–41.
Dy GW, Salibian AA, Blasdel G, Zhao LC, Bluebond-Langner R. External genital revisions after gender-affirming penile inversion vaginoplasty: surgical assessment, techniques, and outcomes. Plast Reconstr Surg. 2022;149:1429–38.
Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. 2013;64:141–9.
Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int. 2007;100:607–13.
Boas SR, Ascha M, Morrison SD, Massie JP, Nolan IT, Shen JK, et al. Outcomes and predictors of revision labiaplasty and clitoroplasty after gender-affirming genital surgery. Plast Reconstr Surg. 2019;144:1451–61.
Peters BR, Carboy JA, Richards H, Dy GW, Dugi Iii D. Optimizing aesthetics in gender-affirming vaginoplasty and vulvoplasty: a narrative review and discussion based on over 600 cases of transfeminine vulvar construction. Transl Androl Urol. 2024;13:274–92.
Dodsworth L. Womanhood: the bare reality. London: Pinter & Martin; 2019.
McCartney J. The great wall of vagina. Brighton: Jamie McCartney; 2011.
Herbenick D, Schick V, Reece M, Sanders S, Dodge B, Fortenberry JD. The Female Genital Self-Image Scale (FGSIS): results from a nationally representative probability sample of women in the United States. J Sex Med. 2011;8:158–66.
Vedovo F, Di Blas L, Perin C, Pavan N, Zatta M, Bucci S, et al. Operated male-to-female sexual function index: validity of the first questionnaire developed to assess sexual function after male-to-female gender affirming surgery. J Urol. 2020;204:115–20.
Funding
No funding was provided for this work.
Author information
Authors and Affiliations
Contributions
JS analyzed data, critically reviewed, and wrote the final manuscript. AH conceptualized and designed the study and performed data collection and analysis. GC performed data collection and analysis and contributed to the writing of the manuscript. EK conceptualized and designed the study, and approved the final manuscript as submitted. OA conceptualized and designed the study, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interests.
Ethical approval
All methods were performed per the Helsinki protocols. Institutional review board approval from the Ethics Committee of University of Illinois Hospital (STUDY2023-0642) was obtained. Informed consent was obtained from all participants. Written informed consent was obtained for the publication of all patient images involved.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Smith, J.B., Hefnawy, A., Chen, G. et al. Management of cosmetic concerns after gender-affirming vaginoplasty: a retrospective case series and guide to revisions. Int J Impot Res 37, 914–919 (2025). https://doi.org/10.1038/s41443-025-01039-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-025-01039-0
This article is cited by
-
Comment on: Management of cosmetic concerns after gender-affirming vaginoplasty: a retrospective case series and guide to revisions
International Journal of Impotence Research (2025)